Translate this page into:
Errors of inclusion and exclusion in income-based provisioning of public healthcare: Problems associated with below poverty line cards
2 Department of Gastroenterology and Human Nutrition, All India Institute of Medical Sciences, New Delhi 110029, India
Corresponding Author:
Anoop Saraya
Department of Gastroenterology and Human Nutrition, All India Institute of Medical Sciences, New Delhi 110029
India
ansaraya@yahoo.com
| How to cite this article: Bajpai V, Singh N, Sardana H, Kumari S, Vettiyil B, Saraya A. Errors of inclusion and exclusion in income-based provisioning of public healthcare: Problems associated with below poverty line cards. Natl Med J India 2017;30:348-351 |
Abstract
This study examined the effect of out-of-pocket expenditure of patients on their illness and other household changes impacting on their well-being, and assessed the socioeconomic status and below poverty line (BPL) card status among patients at the All India Institute of Medical Sciences, New Delhi. We did a hospital-based cross-sectional study of 374 inpatients and outpatients. Among the 374 study subjects, more than 69% of poor did not possess a BPL card. On the other hand, 5.5% of the above poverty line patients among the respondents possessed a BPL card. Of those having BPL cards, 84.4% belonged either to the lower middle, upper lower and lower socioeconomic status categories. Our data suggest that the inaccuracies in providing BPL cards limit access of the genuine poor to healthcare. In the light of national-level surveys on accessing healthcare and out-of-pocket expenditure by patients there is a case against ‘targeting’ in the delivery of public health services and user charges have an adverse impact on access to healthcare by the poor.
Introduction
Levying of user charges at the time of availing healthcare services is widely prevalent in publicly financed healthcare in India. This practice affects the ability of the poor to access healthcare services is often dismissed on the ground that those possessing below poverty line (BPL) cards are exempt from such payments. A few hospital-based studies provide evidence[1] that there are major errors in the inclusion and exclusion of people in the BPL category. Hence, whether poor patients are actually being excluded from the healthcare safety net remains a matter of conjecture. We did this survey at the All India Institute of Medical Sciences (AIIMS), New Delhi to examine the effect of out-of-pocket (OOP) expenditure of patients on their illness, dietary consumption and other household changes, as well as to assess the socioeconomic and BPL card status of the respondents.
Methods
This hospital-based, descriptive, cross-sectional study was done among outpatients and inpatients of the Departments of Gastroenterology and Human Nutrition, and Cardiology as well as Comprehensive Rural Health Services Project hospital, Ballabgarh, Haryana between September–October 2005 and January 2006. The patient and/or any adult family member was the respondent. After obtaining verbal consent, the interviewer explained all the pertinent information of the study and allowed the respondents an opportunity to ask questions and verified that they understood the information.
A pre-designed and pre-tested semi-structured interview schedule with both closed- and open-ended questions was used. The interview schedule was pre-tested by administering it to 20 participants (data not included in this study). Besides questions on per capita income, dietary consumption, expenditure patterns, indebtedness, specific questions on the BPL card were asked including those related to awareness, possession, the ‘free of cost’ services using the card, if eligible have they made efforts to obtain such a card, what problems were faced while making such a card, have they seen/heard of a bribe being paid for making a BPL card, whether they have availed of free treatment at a government hospital using the BPL card, etc.
The patients' family per capita income was also asked for and their socioeconomic status as per the Kuppuswamy socioeconomic[2] status scale revision for the year 2003 was obtained. The BPL/ APL (above poverty line) bifurcation of the respondents was done using the all India poverty cut-offs for 2004–05 as declared by the Planning Commission (2009).[3] These were ₹446.68 for rural and ₹578.80 for urban areas.
Statistical analysis
Categorical variables were summarized as frequency (%). Quantitative variables were checked for normal distribution. Variables following normal distribution were summarized as mean (SD) while those following non-normal distribution were summarized as median (range). All statistical analyses were done using STATA 9.0 (Statacorp, Texas, US).
Results
Of the 374 patients included (convenience sample), 237 were males (63.4%). Most of the patients came from rural areas (243; 65%), were outpatients (310; 83.3%) and their median (range) per capita family income (n=278; 74.3%) was ₹1085 (₹80–₹250 000); 96 patients declined to disclose their income. Based on the cut-off income for poverty, 42 of 278 patients (15%) were BPL while the rest were APL (236, 85%). Only 19 of 42 patients (45.2%) who were BPL by the cut-off income were aware of the BPL card, whereas 157 of 236 (66.5%) among the APL were aware of the BPL card.
Forty-eight patients had a BPL card. Of these 22 declined to disclose their income, and 13 each were BPL and APL by the income cut-off. Hence, 69% (13/42) of the BPL patients did not have a BPL card but 5.5% (13/236) of those who were APL had a BPL card.
The median per capita income of BPL patients based on the income cut-off was almost half that of those who had BPL cards [Table - 1]. Based on the socioeconomic status, 17.7% (8/45) of those with BPL cards belonged to the lower middle category and 66.7% (30/45) to the upper lower and lower categories [Table - 1].
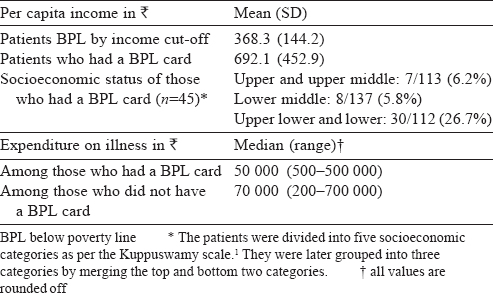
It is also important that over 50% among those in the BPL category by the income cut-off were not aware of the BPL card.
Discussion
Poor people being excluded from official security nets are common and have been part of the policy debate in India.[4],[5],[6],[7],[8],[9],[10],[11],[12] Despite the fact that these errors occur in various targeted social sector programmes, policy planners in both developed and developing countries have continued ‘targeting’ and trying to refine the design of these programmes to improve the delivery of social services to the poor.
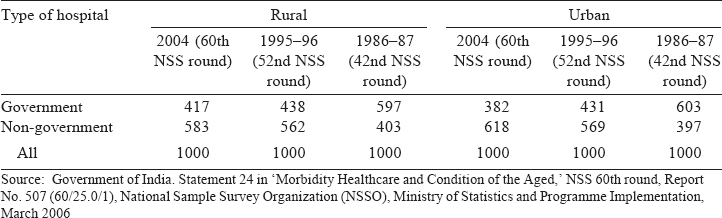
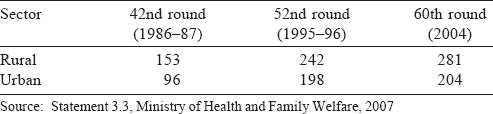
The evidence from national-level surveys [Table - 2],[Table - 3],[Table - 4],[Table - 5],[Table - 6],[Table - 7] suggests that the strategy of refining designs has not worked. The share of government hospitals for non-hospitalized treatment was already low but this been decreasing over the years even for hospitalized patients [Table - 2]. Thus patients, including those who are in the BPL category have to increasingly depend on private healthcare. This is often because the healthcare facilities are too far (19% responders), they are dissatisfied with the treatment by the doctor/facilities (42%), because of long waiting hours (11%) and lack of required services (5%).[13] Therefore, fewer poor patients are able (or willing) to avail of free treatment that they are entitled to in government hospitals.
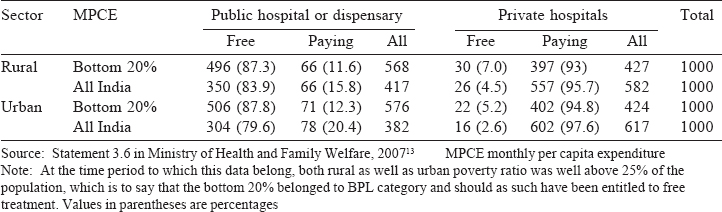
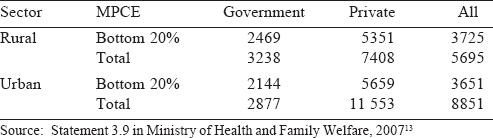
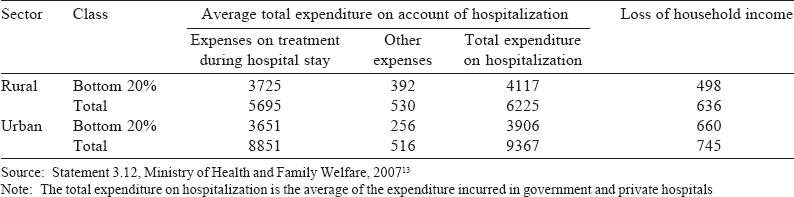
In rural areas, 87.3% of patients from the bottom 20% of the monthly per capita expenditure (MPCE) who sought hospitalization in a government hospital were treated in free wards [Table - 3]. Overall, this proportion was 83.9% for rural areas and 87.8% for bottom 20% of the MPCE and 79.6% all India for urban areas. However, despite the overwhelming number of patients in the bottom 20% being treated under the category of free beds in both rural and urban areas, there was a huge OOP expenditure incurred on hospitalization by these patients [Table - 4]. Much of this expenditure was not due to incidental expenses such as travel, food or accommodation, etc. but due to treatment-related expenses in the hospital. Hence, despite availing of concessions due to BPL patients, there was a large OOP expenditure.
Economic access to healthcare has become increasingly difficult for the poor due to a real increase in the cost of treatment, and financial difficulties have resulted in an increasing proportion of untreated illness [Table - 6] and [Table - 7].
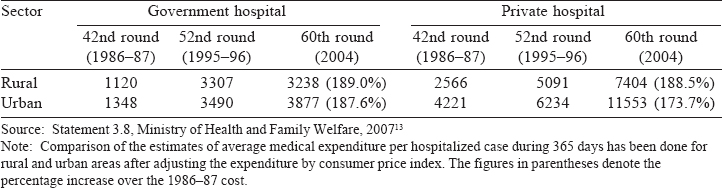
Publicly funded social security nets for the poor can be best ensured when delivered through public facilities. However, deterioration in services at public hospitals has resulted in a drop in their share of hospitalized treatment and even the poor have to access hospitalized care in the private sector. Simultaneously, there has been a real increase in the cost of care in both public and private hospitals over the years, with the rate of increase being marginally higher for public hospitals.[14] This shows that levying user charges in public hospitals on the plea of cross-subsidizing care for the poor by charging those who can afford to pay while exempting those with a BPL card from paying these charges is inappropriate because:
- There are errors in the inclusion and exclusion of patients from those who are in the BPL category and hence entitled to free/ subsidized treatment. In our study 69.1% of BPL patients by the income cut-off did not possess a BPL card.
- A number of those not entitled to free/subsidized treatment possessed BPL cards and hence were able to avail of services that they were not entitled to. In our study, 5.5% of the APL category by income cut-off had BPL cards. Further, the mean per capita incomes of those who had BPL cards was higher than that of patients below the income cut-off for both rural and urban areas.
- For social security schemes to be implemented efficiently and effectively, these need to be supported proactively. There needs to be a much greater awareness among all the stakeholders regarding the provisions of the scheme otherwise the objectives of these schemes can be derailed by lack of awareness among the stakeholders regarding the importance and provisions of the schemes.
We are not aware of any systematic proactive measures being taken either at AIIMS or at other public hospitals in Delhi, to make poor patients aware of the privileges due to them on possession of a BPL card and the obligation on the part of healthcare providers to honour these provisions. Even if targeted interventions for the poor in hospitals are desirable over universal service delivery, waivers for BPL cardholders can be efficiently facilitated through measures such as posters and notice boards at prominent places within hospital premises providing complete information regarding the rights of BPL cardholders and the process for availing these rights. Help desks can be made available to enable poor patients to avail of their rights. However, getting sanctions for such waivers is cumbersome serving as a deterrent for patients to avail of the facility.
The objective of ‘targeting’ in welfare policy is to narrow down the scope of recipients by applying diagnostic criterion of means or income, through claw back taxes, behavioural requirements or status characteristics.[15]
However, these are camouflaged as ‘cost containment’ and ‘efficiency’ in reaching resources to the genuinely needy because an obvious attempt to dismantle the ‘universal welfare’ model would be untenable in view of its continuing popular appeal, especially in developing countries.
The rhetoric of ‘exempting the poor from user charges’ is further undermined by the receding role of public healthcare in health service delivery. Privatization of the social sector services is a characteristic of the economic liberalization.[16],[17],[18] In India, the growth of private healthcare has come at the cost of public sector healthcare.[19],[20],[21] These developments have implied a gradual deterioration in the services of the public sector due to under-financing and lack of resources resulting in non-availability of drugs and other consumables, non-availability of routine diagnostic tests and deficiency of health manpower. This obliges the patients, including the poor, to source drugs and other consumables and diagnostic tests from the market. All that is then available to them for free is the doctors' consultation, provided they are available, and the hospital bed, presuming that patients are not asked for any informal payments.
As per the 60th NSS round 42.7% of patients even in the bottom 20% of the MPCE class accessed hospitalized care from the private sector [Table - 2]. Thus, if the poor are to be assured of any healthcare services it can be only through strengthening of public provisioning free from the motive of profit.
Limitations
Our study data are old and hence there may have been changes in the overall performance of the healthcare sector. However, the focus has even recently been on introducing and enhancing user charges. Hence, it is unlikely that the overall situation with regard to access to healthcare with the use of BPL cards has improved. Of all the questions we had planned to ask, data were satisfactorily gathered from all the patients only regarding knowledge and possession of BPL card as these were closed-ended questions with ‘yes’ and ‘no’ answers. Satisfactory data could not be collected with respect to other questions from all the patients because (i) a substantial number of patients did not have any knowledge regarding the BPL card, (ii) many among those who did know about the BPL card or had one were poorly informed regarding the benefits of such a card, (iii) as most were outpatients (82.9%), it was difficult to obtain and record detailed information from them in a crowded outpatient.
Conclusion
The shift from ‘universalism’ to ‘targeting’ in healthcare policy has come with the rightward shift in the political and economic discourse worldwide. This is a generalized thrust towards privatization and commercialization of the healthcare sector where the state is sought to be absolved of its responsibilities towards the welfare of the people. Consequently, all attempts to remedy the numerous errors of exclusion and inclusion in such targeted social sector interventions by improving their design are unlikely to succeed. The need is to create policies to provide healthcare to poor universally without levying user charges or with a motive of profit.
| 1. | Bajpai V, Singh N, Sardana H, Kumari S, Vettiyil B, Saraya A. Economic and social impact of out-of pocket expenditure on households of patients attending public hospitals. Natl Med J India 2017;30:15-20. [Google Scholar] |
| 2. | Mishra D, Singh HP. Kuppuswamy socioeconomic status scale:A revision. Indian J Pediatr 2003;70:273-4. [Google Scholar] |
| 3. | Planning Commission. Report of the expert group to review the methodology for estimation of poverty. Government of India, Planning Commission; November 2009. [Google Scholar] |
| 4. | Hirway I. Identification of BPL households for poverty alleviation program. Econ Polit Wkly 2003;38:4803-8. [Google Scholar] |
| 5. | Mahamallik M, Sahu GB. Identification of the poor: Errors of exclusion and inclusion. Econ Polit Wkly 2011 ;46:71-7. [Google Scholar] |
| 6. | Bapat M. ‘Poverty lines and lives of the poor:Underestimation of urban poverty: The case of India’, Poverty Reduction in Urban Areas Working Paper 20. London:International Institute for Environment and Development (IIED); 2009. [Google Scholar] |
| 7. | Mane RP. Targeting the poor or poor targeting: A case for strengthening the public distribution system of India. J Asian African Studies 2006; 41: 299-317. [Google Scholar] |
| 8. | Chhotoray S. The poor fight to stay on BPL list. Infochange News and Features; Oct 2011. Available at http://infochangeindia.org/poverty/features/the-poor-fight-to-stay-on-bpl-list/print.html (accessed on 12 Feb 2014). [Google Scholar] |
| 9. | Lavallée E, Olivier A, Pasquier-Doumer L, Robilliard AS. Poverty alleviation policy targeting: A review of experiences in developing countries. Document De Travail DT/2010-10. Paris:Instutut de recherché pour le developpement, 2010. [Google Scholar] |
| 10. | Skoufias E, Davis B, de la Vega S. ‘Targeting the poor in Mexico: An evaluation of the selection of households for PROGRESA’. FCND Discussion Paper No. 103. Washinghton DC:Food Consumption and Nutrition Division, International Food Policy Research Institute; March 2001. [Google Scholar] |
| 11. | Mkandawire T. ‘Targeting and universalism in poverty reduction’. Social Policy and Development Programme Paper Number 23. Geneva, Switzerland:United Nations Research Institute for Social Development; December 2005. [Google Scholar] |
| 12. | Pritchett L. ‘Political economy of targeted safety nets’. Social Protection Discussion Paper Series, No 0501. Social Protection Unit, Human Development Network. Washington DC:The World Bank; Jan 2005. [Google Scholar] |
| 13. | Ministry of Health and Family Welfare (MOHFW). Select health parameters: A comparative analysis across the National Sample Survey Organization (NSSO) 42nd, 52nd and 60th Rounds. New Delhi:MOHFW, Government of India; 2007. [Google Scholar] |
| 14. | Thakur JS. Key recommendations of high-level expert group report on universal health coverage for India. Indian J Community Med 2011;36:S84-S85. [Google Scholar] |
| 15. | Gilbert N (ed). Targeting social benefits: International perspectives and trends. New Brunswick, NJ:Transaction Publishers; 2001:xviii. [Google Scholar] |
| 16. | Navarro V. Neoliberalism as a class ideology; or, the political causes of the growth of inequalities. Int J Health Serv 2007;37:47-62. [Google Scholar] |
| 17. | World Bank. World Development Report 1993: Investing in health. New York:Oxford University Press; 1993. Available at https://openknowledge.worldbank.org/handle/10986/5976 License: CC BY 3.0 IGO (accessed on 23 Jun 2017). [Google Scholar] |
| 18. | Quiggin J. Globalisation, neoliberalism and inequality in Australia. Econ Labour Relat Rev 1999;10:240-59. [Google Scholar] |
| 19. | Jan Swasthya Abhiyan. Health system in India: Crisis and alternatives; Towards the National Health Assembly II, Booklet 2. New Delhi:National Coordination Committee, JSA; October 2006. [Google Scholar] |
| 20. | Hazarika I. Medical tourism: Its potential impact on the health workforce and health systems in India. Health Policy Plan 2010;25:248-51. [Google Scholar] |
| 21. | Baru RV. Challenges for regulating the private health services in India for achieving universal health care. Indian J Public Health 2013;57:208-11. [Google Scholar] |
Fulltext Views
1,493
PDF downloads
374




