Translate this page into:
Family planning training needs of auxiliary nurse midwives in Jharkhand, India: Lessons from an assessment
Corresponding Author:
Nerges Mistry
Foundation for Research in Community Health, Trimiti B Apartments, 85 Anand Park, Lane No. 1, Aundh, Pune 411007, Maharashtra
India
frchpune@gmail.com
| How to cite this article: Karvande S, Sonawane D, Samal J, Mistry N. Family planning training needs of auxiliary nurse midwives in Jharkhand, India: Lessons from an assessment. Natl Med J India 2018;31:73-78 |
Abstract
Background. Auxiliary nurse midwives (ANMs), who play a pivotal role in the provision of maternal health services including family planning services, must be adequately trained and skilled. Systematic assessment of their training needs helps in determining this adequacy. We did a systematic assessment of the training needs of ANMs in Jharkhand.
Methods. We designed a multi-stakeholder study including (i) meeting with government officials and international development partners (n = 1 5); (ii) structured observation of health facilities (n=1 7); (iii) review of health management information system data; (iv) interviews with ANMs (n =19); and (v) interviews with contraceptive users (n = 31 ). The data were thematically analysed based on gaps in technical knowledge, skills and practices; communication and counselling; infrastructural gaps; uptake of contraceptives and emerging training needs and approaches.
Results. The ANMs lacked knowledge, e.g. in natural contraceptive methods and skills, e.g. counselling and record- keeping. Gaps in infrastructure further hampered the provision of uninterrupted service. The belief system of the community about contraception was perceived as a barrier. The lacunae in their knowledge and skills could be attributed to systemic issues such as quality of pre-service education, absence or poor implementation of in-service trainings or individual issues such as incompetence or apathy towards the provision of service. Government training to ANMs in family planning was inadequate.
Conclusion. Our study found inadequacy in the training of ANMs in family planning. We suggest the need for systemic efforts with the life cycle approach to family planning, a mix of theory and practical training, appropriate duration of training, careful selection of trainers, a confidence-building approach and supportive environment to raise competencies of ANMs to help them manage their health facilities.
Introduction
Jharkhand is the thirteenth most populated state in India, witnessing a 22.3% decadal growth higher than the national average ( 17%).[1] The state has committed to provide contraceptives to 2.1 million new users by 2020.[2] However, there are challenges and problems related to non/poor use of contraception such as opposition by men and lack of knowledge resulting in negation of use[3] or consideration of the contraceptive pill as a social taboo even in urban pockets.[4] Lack of knowledge and use of temporary contraceptive methods is considerably lower among tribal women compared to their non-tribal counterparts in the three states: Jharkhand, Madhya Pradesh and Chhattisgarh.[5] These studies point towards the persistent need for systemic efforts including enhancing counselling and communication skills of health providers, especially the auxiliary nurse midwives (ANMs) who play a pivotal role in the provision of family planning services in the public health sector.
India has a total of 1 757 416 nursing personnel with 3405 registered ANMs in Jharkhand.[6] The state has 10 government[7] and 50 private ANM training schools.[6] Despite efforts to increase the number of seats for medical and paramedical courses, the availability of quality trained human resource in the public health sector, especially specialist doctors, MBBS doctors, staff nurses and ANMs, is a problem in the state.[8] There are lacunae in the implementation of clinical practices in the pre-service training or lack of opportunities and skill upgradation during in-service training.[6]
The current curriculum of ANM training with a duration of 2 years covers community health, health promotion, primary healthcare, child health, midwifery and health centre management. In India, the original role of the ANM was to serve the community through the provision of care at the time of birth (skilled birth care) and basic curative services. Over time, the prioritization of provision of family planning and immunization services has been reported by some to have led to the dilution of the role of ANMs, and concerns have been raised that the ANM can no longer be considered ‘fit for purpose’.[9] However, there is a need to assess whether ANMs are adequately trained and skilled to perform their role in priority areas such as family planning.
The state of Jharkhand runs several trainings on its own and in partnership with international development partners for training of health providers in family planning, especially about postpartum or post-abortion contraception or natural methods of contraception. Hence, a systematic assessment of training needs was considered to be a prerequisite since it provides the evidence for designing further training interventions.[10]
We assessed the knowledge, technical and communication skills, infrastructure, uptake of family planning methods, and emerging opportunities for future training.
Methods
The Government of Jharkhand was approached for formal approval to conduct the research. A team of three public health researchers from the Foundation for Research in Community Health (FRCH), a not-for-profit research organization, collected data between November 2014 and January 2015. Recommendations from government and international development partners, district- level indicators related to family planning and district characteristics such as the presence of public-private initiative governed the selection of districts. District X (population of 2 293 919 with 11 blocks) and district Y (population of 1 063 458 with 9 blocks) with contrasting family planning indicators were selected. There were five components of our study, each with their distinct tools and methods of data collection.
Meeting with government officials and international development partners
FRCH, in collaboration with the Government of Jharkhand, invited officials from the state department of family planning and repre sentati ve s of international development partners for a meeting. It involved a brainstorming session about training needs for ANMs and suggestions to improve the same. Fifteen stakeholders who were involved in ANM training and/or family planning initiatives for the state were approached for one-to-one interviews. Participation was voluntary and not influenced by any monetary incentives or preferences. All of them agreed and were interviewed using a structured interview guide. The questions included factual information about family planning use, training coverage for ANMs and bottlenecks in the capacity-building initiatives for ANMs. Detailed documentation of the brainstorming session as well as one-to-one interviews helped in the selection of districts for data collection and provided pointers regarding gaps in the existing training and potential approaches for improving training. Blocks, health facilities, ANMs and men and women users were selected through systematic random sampling. Two administrative blocks (a block covers a population of 200 000) were selected from each district by a lottery method.
Structured observation of selected health facilities (n=17)
Three categories of health facilities were selected for structured observations: (i) block-level community health centres (CHCs) of the four selected blocks; (ii) one primary health centre (PHC) per CHC using the lottery method; and (iii) all the health subcentres (HSCs) under the selected PHC. Structured observations of health facilities were undertaken with the help of a checklist that included essential equipment, materials and services at the facility. The Indian Public Health Standards (IPHS 2011)[11] were used as a reference for preparing the checklist. This dataset provided information about gaps related to infrastructure and resources related to family planning services.
Review of the health management information system data
Data of the health management information system (HMIS) were accessed from the state, district and block level to understand the training coverage, needs, gaps related to human resource, infrastructure and services, and uptake of various family planning methods.
Interviews with auxiliary nurse midwives (n=19)
The total number of ANMs in the selected blocks in both districts was 208 (92 in district X and 116 in district Y). Twenty ANMs from the identified health facilities were selected for a one-to-one interview by a lottery method. The interviews were scheduled at the health facilities as per mutual convenience of the respondent and the researchers. Participation in the study was voluntary and not influenced by any monetary gains or preferences. This dataset provided information on issues such as needs and opportunities related to nursing education and training, gaps in family planning services, perspective regarding uptake of family planning services, experiences and needs about communication and counselling for family planning, gaps related to technical knowledge, and skills and practices regarding provision of family planning services to the community. Skills and practices of ANMs in the area of family planning were assessed with the help of a questionnaire having a list of various routine activities for ANMs as per their job description (Indian Nursing Council, 2012) and their responses to two questions: '(i) How important is this activity for your performance?; and (ii) How well do you think you can perform this activity? ‘1σ The responses were graded on a 5-point scale with ‘1’ as the lowest and ‘5’ as the highest value. The roles and responsibilities of ANMs, as per their job description, include being a counsellor, communicate with men and relatives/family members and counsel special populations such as tribal and adolescents on issues of family planning.[12]
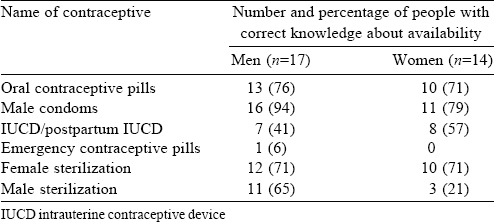
Interviews with users of family planning services (n=31)
This component of data highlighted users’ perspectives, experiences and needs regarding family planning with a focus on counselling and communication. From the list of contraceptive users available with the selected ANMs, men and women users were selected randomly and approached by the ANMs for seeking consent for the interview. The researchers then approached the respondents who agreed to participate in the interview and sought their written consent for the same. One woman user refused to participate in the interview. The interviews were conducted at a place and time convenient to the respondents. The interviews were conducted in Hindi or in Odia by an Odia-speaking researcher. Each interview lasted 30-40 minutes. The questions primarily focused on their demographic details, knowledge regarding availability of family planning services, episodes of interaction with ANMs, source of knowledge and experience of any counselling related to family planning. The interviews with the ANMs and users were conducted with the help of a structured interview schedule. Additional responses from the respondents were pre-coded and analysed quantitatively. The quantitative data were processed with SPS S 22 (IBM Corporation and Others 1989, 2013). The data were analysed to learn from experiences and communication and counselling needs.
The research proposal received ethics clearance from the Institutional Research and Ethics Committee of FRCH (IREC/ 2014/03/11/1). Written permission to conduct this research was obtained from the Jharkhand state health department. Each respondent was interviewed at the health facility after obtaining written informed consent for conducting and audio-recording of the interview. Privacy during the interview, and anonymity and confidentiality of information shared were strictly maintained.
Results
Nursing education and training: Needs and gaps related to technical knowledge, skills and practices of ANMs The state had 10 ANM training centres. However, at the time of this study, only one ANM training centre (ANMTC) had permission to admit new students.
‘Less number of faculties, lack of building and teaching material are the main issues (ANMTC level).
Additionally, poor governance by district health office has resulted in loss of recognition of government ANMTC.'
—Principal ANMTC, District X
This resulted in inadequate number of trained ANMs at health facilities. The number of ANMs who received various in-service trainings, especially training related to family planning, was even lower.
The gap between sanctioned and filled posts was 50% and 22% in districts X and Y, respectively (filled/sanctioned in district X 355/715 and in district Y 423/542). It indicated the need for a trained workforce in the state as well as explains the reason for the unmet need. There was poor coverage of government training of ANMs in the study blocks of both the districts in most of the maternal health subjects except for HMIS [Table - 1]. Figures for HMIS training in district Y were higher as compared to training received in other subjects. However, the district programme manager for district Y mentioned:
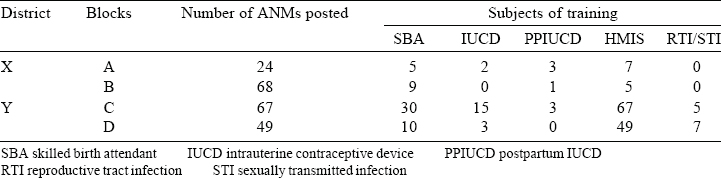
‘All ANMs are just “told” about HMIS at the block level; however, they are not specially trained on the subject.'
—District Programme Manager
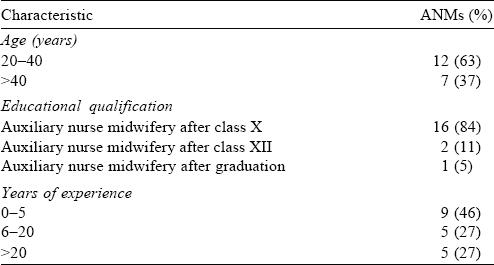
The ANMs interviewed in the study were divided almost equally in the age groups ‘below 40’ (63%) and ‘above 40’ (37%) years. Sixteen per cent of them had >10 years of schooling before joining the ANM course; 58% of ANMs had >5 years of work experience [Table - 2].
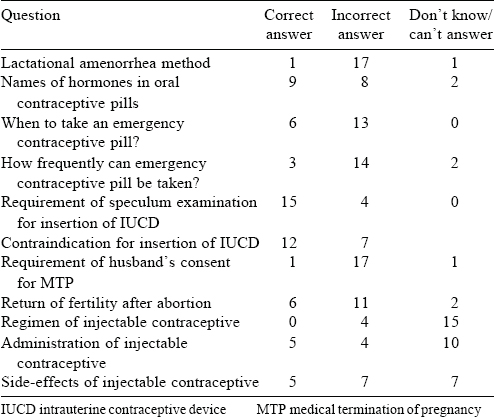
Their assessment for technical knowledge through individual interviews [Table - 3] pointed towards gaps in the following areas: (i) criteria for lactational amenorrhoea method (LAM); (ii) appropriate frequency for administration of emergency contraceptive pills; (iii) contraindications for insertion of intrauterine contraceptive device (IUCD); (iv) return of fertility after abortion; and (v) requirement of husband’s consent for medical termination of pregnancy. In addition, the ANMs lacked knowledge regarding administration or side-effects of injectable contraceptives since inj ectable contraceptives were not part of the family planning programme in the public sector at the time of this study. (Injectable contraceptives have been included in the Government of India family planning programme in early 2016.) However, the ANMs expressed the need to have knowledge on this subject since they had to administer this method of contraception on the demand of the community.
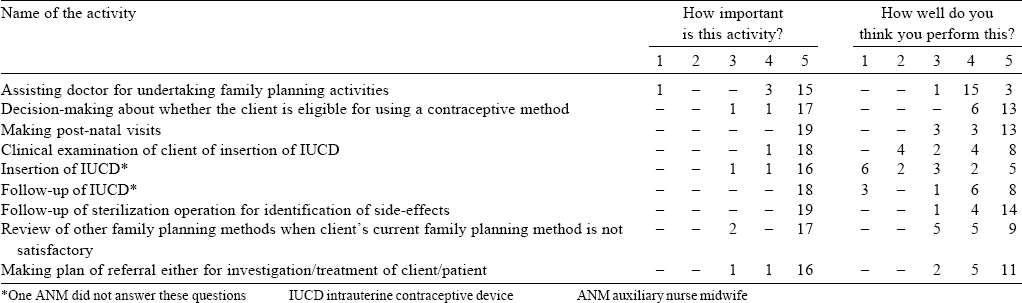
Clinical examination of a woman for insertion of IUCD, insertion of IUCD and follow-up for IUCD were regarded as important activities with a relatively poor performance by ANMs. Although this self-assessment of ANMs suggested that IUCD was the only concern and needed improvement, field observations while conducting their interviews contradicted this and pointed towards gaps in other areas such as provision of information regarding side-effects of oral contraceptive pills and record- keeping skills.
Communication and counselling: Experiences and needs We attempted to learn about the communication and counselling needs from the perspectives of programme officials, ANMs themselves and from the community. Programme officials while expressing their opinions regarding ANMs counselling skills and challenges said:
‘ANMs lack skills and need training and there is no regular hand-holding for them… During the Village Health Nutrition Day, the ANMs are supposed to spend time counselling on family planning as well. In reality, their focus is only on routine immunization and there is nothing discussed regarding family planning. '
—State health programme official (A)
The ANMs were asked to grade importance and actual performance of counselling and communication activities using a questionnaire. All of them graded these activities to be of high importance (grade 5 on a scale of 1 to 5). Except two ANMs (grade 2 on a scale of 1 to 5), the rest were confident about their performance related to counselling [Table - 4]. Responses from the community contradicted this. Community members interviewed during the study mentioned that ANMs and ASHAs were the primary counsellors for family planning. However, counselling involved mere instruction in terms of ' take this pill every night’ or ‘you can stop this pill if you have vomiting’'. All the interviewed women users mentioned not receiving any counselling or follow- up after IUCD/post-partum IUCD insertion. No female respondent received any counselling before or after the operation at the venue. All women users mentioned the follow-up visit of the ANMs on the 7th/8th day of operation for removal of stitches or enquiry about the health of the woman.
Gaps related to infrastructure and resources forfamily planning In district X only 69 of 244 and in district Y only 81 of 194 HSCs were functional in a health department-owned building (8th Common Review Mission Report, 2014-15).
‘Some of the upgraded CHCs have only recently constructed buildings but do not provide necessary services in absence of infrastructure. They are underutilized.'
—State health programme official (B)
Resources and services, e.g. emergency contraceptive pills, were not available in 13 of 17 health facilities visited during the study period.
In addition to infrastructure, family planning services have to be complemented with a regular supply of contraceptives and equipment, workforce and other support services. No health facility visited by us as a part of the study had a special room for family planning services. Of all the health facilities visited, only one HSC reported to have a designated day (Friday) for family planning services in a week. Nevertheless, all health facilities reported that they offer counselling and refer eligible beneficiaries for terminal methods to the nearest CHC.
In general, compliance with IPHS was 20%-30% across HSCs and 40%-50% across PHCs.
Emerging training needs and approaches There were government provisions for in-service training of ANMs in various areas such as IUCD, condom, skilled birth attendance, HIV, integrated management of neonatal and childhood illness, mother and child protection card and HMIS. Of the 19 ANMs interviewed, 7 did not receive in-service training in any of these subjects and 2 had received training in one subject, either in IUCD or condom. They were asked to report about topics covered during their ANM curriculum. Comprehensive training in family planning was mentioned to be the first preference (13 of 19 ANMs) for further training, followed by enhancement of counselling skills (7 of 19) and IUCD (5 of 19) insertion. An equally important aspect of training was the approach adapted for training. Interactive games or simulation were preferred by 16 of 19 ANMs. Practical approach and classroom teaching were preferred by 13 of 19 and 10 of 19 ANMs, respectively, whereas 8 of 19 ANMs expressed an interest towards in-service training with the use of computers and mobiles.
State-level programme officials were requested to provide their views and suggestions regarding further training of ANMs.
‘After the reproductive and child health programmes, there have been no dedicated trainings for the ANMs. There is a need to focus on the basket approach of family planning methods, follow-ups, monitoring and evaluation, etc. Mobile message can be useful for LAM (lactational amenorrhoea method) or ECP (emergency contraceptive pill) subjects. '
—State programme officer, International development partner (1) for family planning
‘The trainings should generally have a confidence- building approach because these are adult learners. ' —Senior Adviser International development partner (2) for family planning
‘Inclusion of private doctors as trainers will be a good idea—an outsider is more respected. '
—State training official
‘An ANM is the manager of her HSC. She should have the data and should know how to analyse the data at her level. Enhancing her skill in this regard may help her in planning and organizing her work more efficiently. ' —State health programme official (B)
These responses stress the need for further training with suggestions such as use of mobile phones, inclusion of private practitioner as a trainer and confidence-building approach of training to raise the competencies of an ANM as a manager for her health facility.
Discussion
The purpose of this systematic needs assessment was to assess the knowledge and skills, training needs and opportunities for ANMs in the provision of family planning services, in the backdrop of existing pre- and in-service training programmes. The results have indicated gaps in the knowledge and skills of ANMs, e.g. in the area of emergency contraceptives, routine investigation before insertion of IUCD or communication with men and other family members for uptake of contraceptive methods. The study has pointed towards preferences, suggestions and opportunities for further training of ANMs. There is a need to review these issues against the pre- as well as in-service training received by ANMs.
India faces a shortage of nursing staff with an estimated deficit of 2 million.[13] The nurse and population ratio in India is 1:2500 compared with ratios of 1: 150 to 1:200 in high-income countries.[14] Nursing education faces constraints related to enriching the curriculum, strengthening faculty development and use of innovative teaching techniques.[15] Nursing and midwifery in India face challenges in the implementation of competencies in actual clinical practice, constraints faced by educational institutes, lack of innovative ideas on teaching and training, and lack of supervision and accountability.[6]
A mismatch between a functional health facility and fully trained health functionaries will be detrimental to providing quality health services. Our study has indicated the infrastructural gaps in the provision of family planning services. Although the Ministry of Health and National Health Mission (NHM) have emphasized on the compliance of health facilities with standards such as IPHS, it varies from state to state and even within facilities in a state. A study that assessed health system competency for maternal health services among health facilities in Odisha found poor IPHS compliance.[16] Inadequacy of quality infrastructure in terms of physical infrastructure, transport, equipment, etc. was identified as one of the health system challenges in another study done in Jharkhand.[17] Hence, the benefits of training healthcare providers can only be realized with the presence of an optimal infrastructure.
The global literature shows wide variation in the roles of midwives. While midwives in developed countries have a strong role to play in reproductive health, midwifery in developing countries has been relegated to a secondary role, especially in India where the ANM’s role is that of a multipurpose worker.[9],[18],[19],[20],[21],[22],[23],[24],[25] The multiple competencies expected from an ANM during her service should obviously be directly proportional to the pre- service education she has received. Jharkhand similar to other Indian states provides 2 years of pre-service training and conducts various in-service training programmes for ANMs with support from international development partners. However, poor presence of government ANM training schools with poor quality of training is clear from issues related to retention of knowledge questions. Insufficient in-service training of ANMs further hampers the availability of skilled workforce. An Indian study showed that students from the diploma and degree programmes of nursing and midwifery lacked confidence in core midwifery skills listed by the ICM.[26] Another study in India reported that a little more than half of ANMs in the study had never received any in-service training even though a majority of them had been in service for more than 5 years.[27] Studies undertaken in Pakistan and Indonesia for the assessment of training of frontline health workers including nurse-midwives have endorsed the need for improvization in clinical and non-clinical skills.[28]·[29] The lacunae in knowledge and skills of ANMs in our study could be attributed to systemic issues such as quality of pre-service education, absence or poor implementation of in-service trainings or individual issues such as incompetence or apathy towards service provision. The pre- and in-service trainings should ultimately result in raising competency of an ANM to be a manager for her health facility.
Since the beginning of the National Rural Health Mission (NRHM) in 2005, there is a distinct perception of a shift of health programme priorities to family planning and immunization and monitoring of most maternal and child health activities with dominance of family planning targets.[9] Despite family planning being one of the ‘priority’ areas, there are gaps in knowledge and skills of family planning service providers, primarily ANMs. These gaps invite more attention towards the approach, methods, tools and evaluation of training programmes.
ANMs in our study expressed a preference for the mixed- methods approach of training with classroom-based theoretical and practical training, and state-level health programme officials have provided valuable suggestions regarding tools and approaches for future trainings. Various studies in India and abroad have shown effective use of mixed-methods including virtual classroom, simulation techniques and games,[30],[31],[32] for increasing the level of competency among nurses. Other studies[33],[34],[35] have pointed towards various attributes of training programmes such as duration, effectiveness over time period and approach and tools used, which have ultimately impacted expected outcomes in terms of increase in knowledge, skills and maternal and neonatal health indicators.
Cultural beliefs seem to play a crucial role in family planning and choice of contraceptive methods. A study from Uttar Pradesh revealed that providers make decisions for family planning based on clients’ education, needs and ability to understand family planning.[36] Hence, providers should be equipped with knowledge of their community and with skills to influence it positively.
In general, strengthening the public health system with an enabling environment, technical capacity, functional health systems, etc. has to be the platform for generating trained health workforce. The functionality of even a well-trained workforce is likely to be reduced in a poor work environment including ill- developed infrastructure. On the other hand, good training can engender a demand for improvement in environment and infrastructure and equip personnel with necessary skill sets for its maintenance and sustainability. Specifically, training initiatives should engender capacities for (i) undertaking advocacy for modifying existing cultures and beliefs in the community served; and (ii) basic management skills directed towards uninterrupted service provision, e.g. drug supplies. Empowering ANMs through instilling leadership qualities by promoting their communication and managerial skills would be symbiotic with the creation of a structure within the public health system that can address workforce feedback and concerns. Ultimately, training must strive to go beyond technical knowledge and skills towards motivation for serving the needy and vulnerable population, since in many locations, ANMs will be the only reflection of a functioning health system. These key changes in training approaches can only be brought about though concerted political will.
Lessons from our study of ANMs are drawn from Jharkhand based on an exploratory study. Hence, more states and districts would need to be studied for programme and policy recommendations regarding ANM education. However, our information is valuable as it provides insights into training needs, opportunities and challenges from multiple perspectives and hence should be the starting point for designing large-scale research studies as well as further training initiatives. The methodology in terms of having multi-stakeholder enquiries, use of standardized scale to assess knowledge and skills and mixed- method approach of observation and interviews can be adapted to other training needs assessment studies.
Only a well-structured training programme with an in-built mechanism for monitoring and evaluation will have the potential to impact competencies of ANMs. The presence of proficient ANMs will ultimately have a cascading effect on the delivery of other health services.
Conflicts of interest. None declared
| 1. | Census of India: Sample Registration System. Available at www.censusindia.gov.in/ 2011-Common/Sample_Registration_System.html_(accessed on 27 Aug 2016). [Google Scholar] |
| 2. | Ministry of Health, Government of Jharkhand. Overview of Family Planning Programme, Department of Family Planning; November 2014. [Google Scholar] |
| 3. | Sengupta R, Das A. Contraceptive practices and unmet need among young currently married rural women in empowered action group (EAG) states of India. J Fam Welf 2012;58:1–4. [Google Scholar] |
| 4. | Kislaya K. Modern Birth Control Methods Still Taboo. Times of India; March 5, 2013. Available at www.timesof1ndia.indiatimes.com/city/ranchi/Modern-birth- control-methods-still-taboo/articleshow/18804957.cms? (accessed on 25 Aug 2016). [Google Scholar] |
| 5. | Prusty RK. Use of contraceptives and unmet need for family planning among tribal women in India and selected hilly states. J Health Popul Nutr 2014;32:342. [Google Scholar] |
| 6. | National Institute of Health and Family Welfare and World Health Organization. Study on Nursing and Midwifery in India: A critical review; December 2012. Available at www.planningcommission.nic.in/data/ngo/csw/csw_nurse.pdf1(accessed on 19 Aug 2016). [Google Scholar] |
| 7. | Ministry of Health and Family Welfare, Government of India. 7th Common Review Mission-Jharkhand, Report, 2013-14. Available at www.nrhm.gov.in/monitoring/ common-review-mission/7th-common-review-mission.html (accessed on 19 Aug 2016). [Google Scholar] |
| 8. | Government of India. National Health Mission, 8th Common Review Mission, Report; 2014. Available at www.nrhm.gov.in/monitoring/common-review-mission/ 8th-common-review-mission.html (accessed on 20 Aug 2016). [Google Scholar] |
| 9. | 9 Mavalankar D, Vora KS. The changing role of auxiliary nurse midwife (ANM) in India: Implications for maternal and child health (MCH). Indian Institute of Management; 1 March 2008. Available at www.iimahd.ernet.in/publications/data/ 2008-03-01Mavalankar.pdf (accessed on 19 Dec 2016). [Google Scholar] |
| 10. | Hennessy DA, Hick CM. University of Birmingham and World Health Organization; 2006. Available at www.who.int/wortforcealliance/knowledge/HennessyHicks_ trainingneedstool.pdf (accessed on 19 Aug 2016). [Google Scholar] |
| 11. | Ministry of Health and Family Welfare. Indian Public Health Standards, Directorate General of Health Services. New Delhi, Government of India; 2012. Available at www.nrhm.gov.in/nhm/nrhm/guidelines/indian-public-health-standards.html (accessed on 19 Aug 2016). [Google Scholar] |
| 12. | Government of Maharashtra. Primary Health Care Manual, Directorate of Health Services, Maharashtra, Mumbai; 2006. [Google Scholar] |
| 13. | Wanted: 2.4 Million Nurses, and That’s Just in India. WHO; 2010. Available at www.who.int/bulletin/volumes/88/5/10-020510.pdf (accessed on 23 Sep 2016). [Google Scholar] |
| 14. | Raha S, Berman P, Bhatnagar A. Some priority challenges of the nursing sector in India. India Health Beat; 2009. Available at www.openknowledge.worldbank.org/ bitstream/handle/10986/12820/702430BRI0P1020k0Final000Vol010no05.pdf? (accessed on 30 Jun 2016). [Google Scholar] |
| 15. | Tiwari RR, Sharma K, Zodpey SP. Situational analysis of nursing education and work force in India. Nurs Outlook 2013;61:129-36. [Google Scholar] |
| 16. | Dehury RK, Samal J. Health system competency for maternal health services in Balasore district and Jaleswar block, Balasore, Odisha, India: An assessment. J Clin DiagnRes 2016;10:IC01. [Google Scholar] |
| 17. | Karvande S, Sonawane D, Chavan S, Mistry N. What does quality of care mean for maternal health providers from two vulnerable states of India? Case study of Bihar and Jharkhand. J Health Popul Nutr 2016;35:6. [Google Scholar] |
| 18. | Malik G. Role of auxiliary nurse midwives in National Rural Health Mission. Nurs J India 2009;100:88–90. [Google Scholar] |
| 19. | De Vries R, Nieuwenhuijze M, Buitendijk SE; Members of Midwifery Science Work Group. What does it take to have a strong and independent profession of midwifery? Lessons from the Netherlands. Midwifery 2013;29:1122-8. [Google Scholar] |
| 20. | Nursing and Midwifery Board of Australia. National Competency Standards for the Registered Nurse; 2006. Available at www.file:///C:/Users/frch%20pune/Downloads/ Nursing-and-Midwifery-Board—Standard—National-competency-standards-for-the-registered-nurse.PDF (accessed on 25 June 2017). [Google Scholar] |
| 21. | Homer CS, Passant L, Brodie PM, Kildea S, Leap N, Pincombe J, et al. The role of the midwife in Australia: Views of women and midwives. Midwifery 2009;25: 673–81. [Google Scholar] |
| 22. | Thornley C. A question of competence? Re-evaluating the roles of the nursing auxiliary and health care assistant in the NHS. J Clin Nurs 2000;9:451-8. [Google Scholar] |
| 23. | Pearcey P. Shifting roles in nursing--does role extension require role abdication? J Clin Nurs 2008;17:1320-6. [Google Scholar] |
| 24. | McKenna H, Hasson F, Smith M. A Delphi survey of midwives and midwifery students to identify non-midwifery duties. Midwifery 2002;18:314-22. [Google Scholar] |
| 25. | American College of Nurse-Midwives, Definition of Midwifery and Scope of Practice of Certified Nurse-Midwives and Certified Midwives; 2011. Available at www.midwife.org/Our-Scope-of-Practice (accessed on 23 Dec 2016). [Google Scholar] |
| 26. | Sharma B, Hildingsson I, Johansson E, Prakasamma M, Ramani KV, Christensson K. Do the pre-service education programmes for midwives in India prepare confident ‘registered midwives’? A survey from India. Glob Health Action 2015;8:29553. [Google Scholar] |
| 27. | Rao AC, Shetty P. Evaluative study on effectiveness of maternal and child health care participatory training program among staff nurses, auxiliary nurse midwives and lady health visitors. J South Asian Fed Obstet Gynaecol 2012;4:120–2. [Google Scholar] |
| 28. | Ariff S, Soofi SB, Sadiq K, Feroze AB, Khan S, Jafarey SN, et al. Evaluation ofhealth workforce competence in maternal and neonatal issues in public health sector of Pakistan: An assessment of their training needs. BMC Health Serv Res 2010; 10:319. [Google Scholar] |
| 29. | Hennessy D, Hicks C, Koesno H. The training and development needs of midwives in Indonesia: Paper 2 of 3. Hum Resour Health 2006;4:9. [Google Scholar] |
| 30. | Agrawal PK, Agrawal S, Ahmed S, Darmstadt GL, Williams EK, Rosen HE, et al Effect of knowledge of community health workers on essential newborn health care: A study from rural India. Health Policy Pian 2011;27:115–26. [Google Scholar] |
| 31. | Arbour MW, Nypaver CF, Wika JC. Innovative uses of technology in online midwifery education. J Midwifery Womens Health 2015;60:278-82. [Google Scholar] |
| 32. | Lundgren R, Sinai I, Jha P, Mukabatsinda M, Sacieta L, León FR. Assessing the effect of introducing a new method into family planning programs in India, Peru, and Rwanda. Reprod Health 2012;9:17. [Google Scholar] |
| 33. | USAID. An MCHIP initiative, strengthening nursing and midwifery pre-service education in India. Facilitators’ guide. March 2012. Available at http://nursingand mi dwife ry. gov. in/prese rvice/Facili tators °%20gu i de-9th °%2 0Ap ri l %202012-final- cg.pdf (accessed on 2 Feb 2018) [Google Scholar] |
| 34. | Singhal N, Lockyer J, Fidler H, Keenan W, Little G, Bucher S, et al. Helping babies breathe: Global neonatal resuscitation program development and formative educational evaluation. Resuscitation 2012;83:90–6. [Google Scholar] |
| 35. | Ronsmans C, Endang A, Gunawan S, Zazri A, McDermott J, Koblinsky M, et al. Evaluation of a comprehensive home-based midwifery programme in South Kalimantan, Indonesia. Trop Med Int Health 2001;6:799–810. [Google Scholar] |
| 36. | Calhoun LM, Speizer IS, Rimal R, Sripad P, Chatterjee N, Achyut P, et al. Provider imposed restrictions to clients’ access to family planning in urban Uttar Pradesh, India: A mixed methods study. BMC Health Serv Res 2013;13:532. [Google Scholar] |
Fulltext Views
2,199
PDF downloads
516




