Translate this page into:
Solutions for India’s Leading Health Challenge: Adopting recommendations from the Disease Control Priorities Network
2 Centre for Chronic Disease Control, Public Health Foundation of India New Delhi, India; London School of Hygiene and Tropical Medicine, London, UK,
Corresponding Author:
Shuchi Anand
Department of Medicine, Division of Nephrology, Stanford University School of Medicine, California
USA
sanand2@stanford.edu
| How to cite this article: Anand S, Prabhakara D. Solutions for India’s Leading Health Challenge: Adopting recommendations from the Disease Control Priorities Network. Natl Med J India 2018;31:257-261 |
Over the past decade, India’s non-communicable disease (NCD) burden has become a focus of intense national and international research and programmatic work. It is easy to see why, in a densely populated country, NCDs are now the leading cause of death in all states, regardless of their level of economic development.[1] Furthermore, Indians face a disproportionate risk for certain conditions, developing diabetes even at a normal body mass index (BMI)[2] or manifesting heart attacks nearly a decade earlier than other ethnicities.[3] In combination with the lack of patient awareness of early-stage disease, the excess relative risk for cardiovascular disease and diabetes applied to a large, ageing population leads to a staggering absolute burden of both early-stage disease and late-stage complications.
Even as an increasing number of studies recount the heavy burden and dismal management, we lack clear evidence-based pathways to tackle NCDs.[4] Since its inception in 1993, the Disease Control Priorities (DCP3) initiative has attempted to fill this evidence gap by identifying priority areas for health intervention for policy-makers working in resource-constrained countries. In Volume 5 of its third edition, the DCP3 initiative has identified evidence-based, effective and cost-effective interventions that can be implemented at various levels within the health system, from health policy interventions to subspecialty/third-level hospital care. Many of the interventions identified in the essential package of cardiovascular, respiratory and related disorders (CVRDs) volume overlap with strategies set forth in India’s National Health Mission, especially the National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS). We highlight and recommended interventions specifically relevant to the Indian context and their overlap or differences from the National Health Mission.
Methodology for disease control priorities
The DCP initiative takes on the perspective of health policy-makers who face tight budgets and competing demands. By distilling the existing clinical evidence and assembling multidisciplinary experts including epidemiologists, clinical researchers and health economists, DCP generates recommendations to policy-makers for effective and affordable interventions, feasible to their context.[5] The first edition of DCP was a companion to the World Bank’s World Development Report in identifying priorities for health. The second edition assembled more than 600 contributors, was widely disseminated to policy-makers and translated into multiple languages. The third edition presents 9 volumes, covering a range of essential health interventions or conditions including cancer and surgery. Volume 5 is on CVRD including diabetes and kidney disease, with the rationale that these interlinked disorders share common pathways for risk factor control and many overlapping early-stage interventions. After a comprehensive review of the literature—the depth and scope of which has increased exponentially after the 2011 United Nations’ spotlight on NCD as the major health challenge for all countries—the volume’s authors and editors created a package of 36 interventions. Cost of implementation for a low-middle income country was estimated at US$ 23 per person, or an additional 1.25% of India’s gross national income devoted to health.
While India’s relatively advanced health technologies are capable of adopting the entire proposed essential package interventions, the following are more relevant to the Indian context:
Policy interventions
- Tobacco control implementation: India has adopted many of the nPOWER policy recommendations. The latest Global Adult Tobacco Survey[6] shows a drop in the prevalence of Indian tobacco users, with uniformly higher prices and effective pictorial warnings on tobacco packages. Yet, 28% of persons 15 years and older continue to use tobacco. Attention to implementing and enforcing additional strategies, including bans on advertising and on smoking in a public place, may lead to further declines in this substantial population that remains at high risk for CVRDs.
- Salt and trans-fat in manufactured foods: Salt intake among adults in India is at or above 9–10 g/day in rural and urban areas,[7] well above the WHO guidelines to restrict intake to 5 g/day. A range of salt-reduction initiatives have been adopted worldwide;[8] working with food industry to reduce the salt content of manufactured food products may be one of the most effective and cost-effective strategies for salt reduction and is recommended by DCP3.
- Community health workers: India was an early adopter of the community health model with its ASHA and anganwadi workers for maternal and child care and immunizations. With a strong sense of community and family ties in many rural areas of India, community health workers who conduct screening and detection of early-stage disease are likely to be welcomed; DCP3 recommends wider adoption of this role. However, we need to generate additional evidence to support their role in behavioural modification and pharmacological interventions.[11]
- Combination therapy: DCP3 encourages the use of combination therapy (using polypill if available) for multiple risk factor control. With India’s booming and innovative pharmaceutical industry—and with data on the effectiveness of polypill being generated primarily via research done in India[12]—use of generic combination therapy or polypill to tackle multiple risk factors is feasible at a mass scale.
Few studies quantify the amount of trans-fat in the Indian diet,[9] but indirect evidence suggests that some of it at least come from commercial oil preparations and re-use of these oils. Drawing on powerful data showing drop in cardiovascular mortality following Denmark’s trans-fat bans,[10] many countries have adopted a complete ban on trans-fats in manufactured and restaurant food products. While India’s Food Safety and Standard Authority is making progress towards this goal by restricting the allowable proportion of trans-fats in oils, we have yet to see a complete ban on transfats in manufactured food products.
Disease-specific interventions
- Hypertension: DCP3 recommends opportunistic screening for all adults and management at the first-level hospital (community health centres) with the use of generic medications. Hypertension afflicts nearly a third of rural and urban adults in India, and fewer than 1 in 5 are reaching systolic levels <140 mmHg, even as international guidelines call for even stricter blood pressure control. Further single-centre studies indicate a wide variation in approach to therapy (mono v. combination) and use of generic medications.[13] A simplified roster of treatments is recommended with essential medications available at the community health centre level.
- Diabetes: We recommend opportunistic screening for diabetes for high-risk groups (not all adults) and aggressive glycaemic management in those with diabetes. Complications of diabetes, especially foot care and albuminuria, could be addressed at the primary care level. A study done in India provides the basis for a recommendation to use telemedicine for retinopathy screening.[14]
- Myocardial infarction: Latest evidence indicates that protocols for acute myocardial infarction can improve timely access to care for a considerable number of patients.[15] In DCP3, it is recommended that primary health centres be empowered with basic treatment strategies including early administration of aspirin and pathways for timely transfer to the ‘hub’ hospital for advanced care, whether that involve thrombolytics or percutaneous coronary intervention.
- Heartfailure: It represents an understudied burden of disease in India. Ischaemic heart disease seems to cause a majority of the burden in Thiruvananthapuram,[16] but little nationwide data exist. A few inexpensive treatments—beta-blockers and renin angiotensin enzyme receptor blockers—can improve survival in patients with heart failure, yet fewer than a quarter of hospitalized patients in India receive this treatment post-hospitalization for an acute episode.[16] Thus, quality improvement initiatives and efforts to improve medical management, before consideration of more advanced therapies (e.g. implantable cardioverter defibrillator devices), are recommended. Since rheumatic heart disease and consequent heart failure remain a major burden in India, DCP3 also recommends development of national guidelines for appropriate antibiotic use for children with pharyngitis and for secondary prevention in patients with established rheumatic heart disease.
- End-stage kidney disease: India’s end-stage kidney disease population is growing exponentially, and the government is attempting to address this advanced condition by subsidizing dialysis and transplant costs. However, one major resource to optimize the most effective and cost-effective therapy remains untapped: deceased donor transplant. Given the availability of highly trained transplant surgeons and nephrologists, development of a national deceased donor registry that further facilitates transplant for a larger portion of end-stage kidney disease patients is recommended to tackle the growing burden of this advanced, costly-to-treat disease.
- Asthma and chronic obstructive pulmonary disease: Algorithm-based care at secondary hospitals for acute exacerbations can improve outcomes including protecting from admission to an intensive care unit.[17] In chronic phases, teaching patients to identify symptoms and consistently use inhaled corticosteroids and beta-agonists as indicated prevents hospitalizations and improves quality of life. These 4 major interventions are recommended in DCP3 and, if implemented successfully, could provide substantial benefits to the growing burden of persons living with chronic obstructive pulmonary disease in India.
Overlap and distinction from the National Health Mission
The National Health Mission of India lays out several policy priorities for addressing NCDs and designates several new centres or institutes to address specific conditions. Several of these institutes are relevant to CVRD, including the NPCDCS, National Tobacco Control Programme (NTCP) and National Programme for Palliative Care.
On a policy level, the NTCP framework emphasizes ongoing enforcement of plans for public smoking and pharmacological treatments for nicotine addiction, all recommendations in line with the WHO mPOWER and DCP3’s Essential Package. Evaluation of fiscal policies aimed at altering dietary patterns (e.g. compulsory salt reduction or bans of transfats in manufactured food products) is not emphasized in the framework to tackle CVRDs but is recommended for consideration by DCP3.
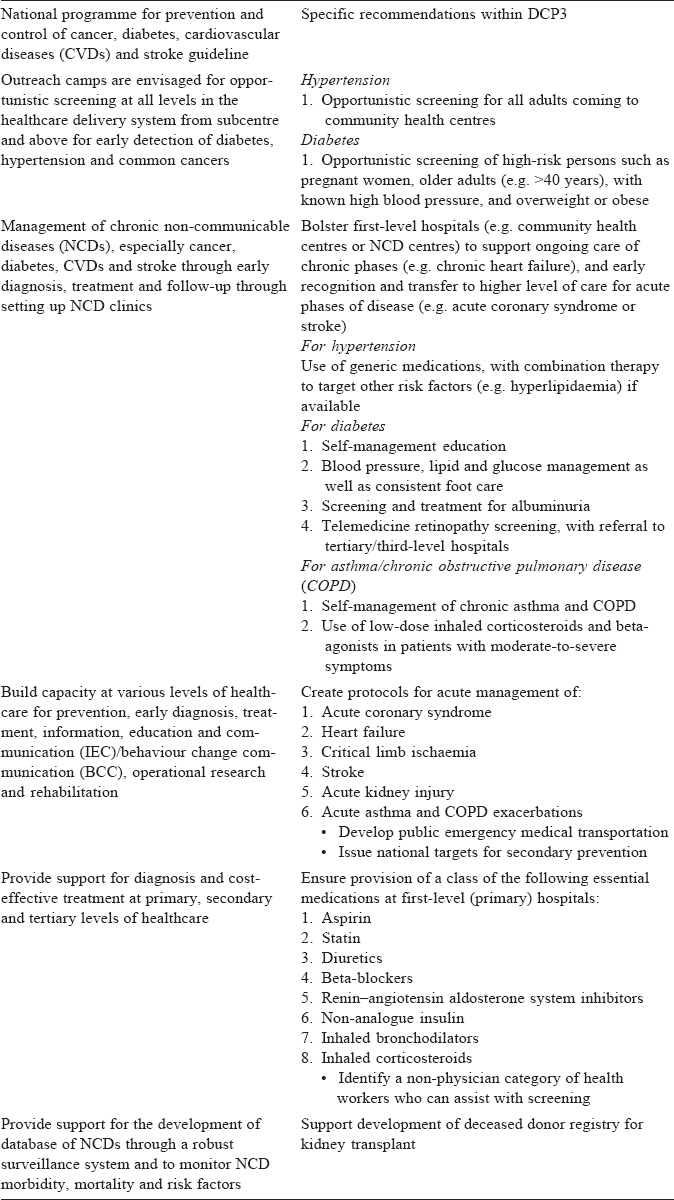
On a disease-specific level, the NPCDCS outlines a general framework for health promotion, screening and management. Further, via a new initiative called Aayushman Bharat, direct support is being provided to supplanting subcentres with health and wellness clinics, with a heavy and broad focus on primary care. [Table - 1] gives some specific recommendations drawn from DCP3 work that could help to operationalize this framework.
Conclusions
The National Health Protection Scheme and Aayushman Bharat make important strides by placing NCDs on India ' s health agenda. There are several similarities to recommendations made by DCP3—the most impactful of which is emphasis on bolstering primary care— but there are some differences. DCP3 recommends opportunistic screening for hypertension and diabetes, while the Government of India envisages universal screening, which is likely to be an expensive strategy with marginal incremental benefits. Effectiveness of screening depends on screened persons’ health-seeking behaviour and easy access to appropriate medical care, both of which are not likely to be optimal when mass screening is used. Second, the DCP3 proposes a limited set of specific interventions (e.g. use of generic medications to control blood pressure, or provision of regular foot care in diabetes) that can not only be implemented in a universal healthcare package, but are also likely to provide for financial protection of affected families and individuals. Third, DCP has recommendations on what not to invest in, for example, advanced therapies for heart failure such as implantable cardioverter defibrillators or analogue insulin, whereas the NPCDCS does not attempt to prioritize the menu of interventions available for specific interventions. Despite these differences, we believe that the broad framework laid out by NPCDCS in Aayushman Bharat can accommodate several evidence-based and cost-effective interventions advocated by DCP3, particularly when disease-specific protocols are developed and implemented.
Conflicts of interest. None declared
| 1. | India State-Level Disease Burden Initiative Collaborators. Nations within a nation: Variations in epidemiological transition across the states of India, 1990-2016 in the Global Burden of Disease Study. Lancet 2017;390:2437-60. [Google Scholar] |
| 2. | Gujral UP, Vittinghoff E, Mongraw-Chaffin M, Vaidya D, Kandula NR, Allison M, et al Cardiometabolic abnormalities among normal-weight persons from five racial/ethnic groups in the United States: A cross-sectional analysis of two cohort studies. Ann Intern Med 2017;166:628-36. [Google Scholar] |
| 3. | Prabhakaran D, Jeemon P, Roy A. Cardiovascular diseases in India: Current epidemiology and future directions. Circulation 2016;133:1605-20. [Google Scholar] |
| 4. | Kanaya AM. India’s call to action-prioritize chronic cardiovascular disease. JAMA Intern Med 2018;178:373-4. [Google Scholar] |
| 5. | Prabhakaran D, Anand S, Gaziano T, Mbanya JC, Wu Y, Nugent R (eds). Cardiovascular, respiratory, and related disorders. Disease Control Priorities. 2017 ed. Washington, D.C.:World Bank; 2017. [Google Scholar] |
| 6. | World Health Organization. Global Adult Tobacco Survey. Geneva:World Health Organization; 2017. [Google Scholar] |
| 7. | Johnson C, Praveen D, Pope A, Raj TS, Pillai RN, Land MA, et al. Mean population salt consumption in India: A systematic review. J Hypertens 2017;35:3-9. [Google Scholar] |
| 8. | Trieu K, Neal B, Hawkes C, Dunford E, Campbell N, Rodriguez-Fernandez R, et al. Salt reduction initiatives around the world—a systematic review of progress towards the global target. PLoS One 2015;10:e0130247. [Google Scholar] |
| 9. | Bhardwaj S, Passi SJ, Misra A, Pant KK, Anwar K, Pandey RM, et al. Effect of heating/reheating of fats/oils, as used by Asian Indians, on trans fatty acid formation. Food Chem 2016;212:663-70. [Google Scholar] |
| 10. | Restrepo BJ, Rieger M. Denmark’s policy on artificial trans fat and cardiovascular disease. Am J Prev Med 2016;50:69-76. [Google Scholar] |
| 11. | Joshi R, Alim M, Kengne AP, Jan S, Maulik PK, Peiris D, et al. Task shifting for non-communicable disease management in low and middle income countries—a systematic review. PLoS One 2014;9:e103754. [Google Scholar] |
| 12. | Indian Polycap Study (TIPS), Yusuf S, Pais P, Afzal R, Xavier D, Teo K, et al. Effects of a polypill (Polycap) on risk factors in middle-aged individuals without cardiovascular disease (TIPS): A phase II, double-blind, randomised trial. Lancet 2009;373:1341-51. [Google Scholar] |
| 13. | Anchala R, Kannuri NK, Pant H, Khan H, Franco OH, Di Angelantonio E, et al. Hypertension in India: A systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens 2014;32:1170-7. [Google Scholar] |
| 14. | Rachapelle S, Legood R, Alavi Y, Lindfield R, Sharma T, Kuper H, et al. The cost-utility of telemedicine to screen for diabetic retinopathy in India. Ophthalmology 2013;120:566-73. [Google Scholar] |
| 15. | Alexander T, Mullasari AS, Joseph G, Kannan K, Veerasekar G, Victor SM, et al. A system of care for patients with ST-segment elevation myocardial infarction in India: The Tamil Nadu-ST-segment elevation myocardial infarction program. JAMA Cardiol 2017;2:498-505. [Google Scholar] |
| 16. | Harikrishnan S, Sanjay G, Anees T, Viswanathan S, Vijayaraghavan G, Bahuleyan CG, et al. Clinical presentation, management, in-hospital and 90-day outcomes of heart failure patients in Trivandrum, Kerala, India: The Trivandrum Heart Failure Registry. Eur J Heart Fail 2015;17:794-800. [Google Scholar] |
| 17. | McFadden ER Jr, Elsanadi N, Dixon L, Takacs M, Deal EC, Boyd KK, et al. Protocol therapy for acute asthma: Therapeutic benefits and cost savings. Am J Med 1995;99:651-61. [Google Scholar] |
Fulltext Views
1,531
PDF downloads
808




