Translate this page into:
Orbital tuberculosis with involvement of the eyelid: An unusual presentation
2 Department of Respiratory Medicine, Command Hospital (Central Command), Lucknow, Uttar Pradesh, India
Corresponding Author:
Surya Kant
Department of Respiratory Medicine, King George Medical University, Chowk, Lucknow 226003, Uttar Pradesh
India
skantpulmed@gmail.com
| How to cite this article: Verma AK, Singh A, Kishore K, Pandey MK, Kant S. Orbital tuberculosis with involvement of the eyelid: An unusual presentation. Natl Med J India 2018;31:279-280 |
Abstract
Although cases of ocular tuberculosis (TB) are increasing, involvement of the eyelid and orbit are unusual. These cases occur secondary to the presence of TB elsewhere in the body, usually pulmonary TB. The primary infection of orbit or eyelid is a rare occurrence. We report a 4-year-old child with primary orbital TB and involvement of the eyelid. The diagnosis of TB should not be missed in patients with ocular symptoms (especially in India) as it is a treatable condition and delays in diagnosis or incorrect diagnosis can lead to serious sequelae.
Introduction
As per the Global Tuberculosis (TB) report 2017, the estimated incident cases of TB in India in 2016 were 28 lakhs (2.8 million) accounting for about one-quarter of the world’s cases of TB.[1] Around 10% of those infected develop disease, either pulmonary or extrapulmonary TB. Extrapulmonary TB comprises 10%-15% of the total burden of TB. The incidence of extrapulmonary TB is on the rise because of human immunodeficiency virus (HIV)-TB correlation and emergence of drug resistance. Ocular TB includes TB infection of the intraocular structures as well as adnexa such as eyelid and lacrimal glands. Involvement of orbit and lacrimal glands is uncommon, more so as a primary infection. We report a case of eyelid TB with sinus formation, with involvement of bones of orbit in a 4-year-old girl child, without any evidence of TB focus elsewhere in the body. This case highlights that a high index of suspicion is required for evaluation of patients with ocular symptoms to rule out TB as a cause in TB endemic countries such as India.
The Case
A 4-year-old girl child presented to the Department of Ophthalmology with complaints of swelling of the right upper eyelid for the past 6 months. The swelling gradually increased in size and was associated with increased lacrimation from the right eye, occasionally with purulent discharge. She was unable to close the right eye due to the swelling. She also had low-grade fever. Despite several courses of antibiotics, the purulent discharge continued to increase.
Local examination of the right eye showed a sinus at the inferolateral aspect of the upper eyelid. The eye was wet due to purulent discharge from the sinus. There was a globular, fluctuant, non-tender swelling on the bulbar surface of the right eye, measuring 1.5 cmx1.5 cm. Exposure keratopathy was present [Figure - 1].
 |
| Figure 1: Photograph showing a globular swelling on the bulbar surface of the eye, measuring 1.5 cmx1.5 cm. Exposure keratopathy and eyelid oedema are also seen. |
A computed tomography (CT) scan of the orbit [Figure - 2] showed an ill-defined cystic lesion at the fornix of the right upper lid on the superolateral aspect along with thickening of both upper and lower eyelids and stranding of fat planes. Furthermore, it revealed osteolytic changes over the temporal process of the right frontal bone and an irregular tract extending in diploic space, suspicious of an infectious pathology. The patient was referred to us to rule out TB.
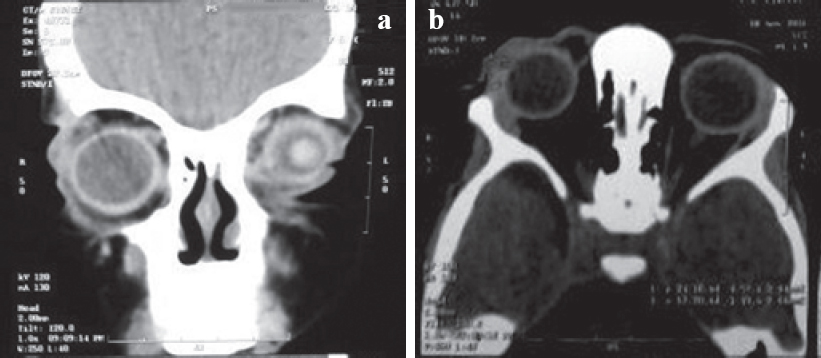 |
| Figure 2: Computed tomography of the right orbit (a coronal view; b axial view) showing an ill-defined cystic lesion at the fornix of the right upper lid on the superolateral aspect along with thickening of both the upper and lower eyelids and stranding of fat planes. Osteolytic changes over the temporal process of the right frontal bone are also seen. |
She had a history of contact with a patient who had pulmonary TB (her uncle who lived with her). There was no peripheral lymphadenopathy. Abdominal examination showed no organomegaly. The Mantoux test showed 13 mm induration. Chest X-ray revealed no abnormality. Histopathological examination of the tissue from the swelling showed epithelioid cell granulomas in the background of dense lymphocytic infiltration of the stroma. After consultation with the ophthalmologist and review of the clinico-radiological features, she was prescribed CAT 1 antituberculosis therapy (ATT) under the Revised National Tuberculosis Control Programme (RNTCP). At the next follow- up visit, there was reduction in lid oedema and eye discharge. However, the exposure keratopathy did not abate.
Discussion
After primary infection, which usually occurs during childhood, there can be 2 fates of the bacilli. Either the infection spreads through bloodstream to various organs, causing fulminant disease (primary TB), or it is contained by the body’s immunity and the bacilli remain dormant in those organs, without causing disease. Later in life, with suppression of immunity, these bacilli can be reactivated causing disease (secondary TB).
Similar to TB elsewhere, ocular TB can be either primary (external infection directly in the eyes or its appendages) or secondary to infection elsewhere (lung, haematogenous spread; sinuses or skin, direct spread).
Ocular TB includes involvement of the intraocular structures as well as adnexa such as the eyelid and lacrimal glands. Ocular TB affects around 1% of the population.[2] The most common clinical presentations of ocular TB are anterior uveitis, choroiditis and sclerokeratitis. Among the various intraocular structures, the most common site of involvement is the uveal tract, because of the profuse blood supply. Although primary ocular TB is unusual, only 40% patients with features suggestive of ocular TB have evidence of coexisting pulmonary TB.[3]
Involvement of the orbit and eyelids by TB is uncommon. TB of the eyelids can present as lupus vulgaris (a form of cutaneous TB), a cold abscess of the eyelid or a chalazion.[4] In the past 50 years, only 5 cases of orbital TB have been reported in the western literature.[4] These patients can present with swelling of the eyelid, pain, proptosis, headache, diminished vision and increased lacrimation. Orbital involvement can also be in the form of TB of the lacrimal gland (dacryoadenitis).[5] It mimics bacterial dacryoadenitis, with abscess formation being reported rarely. All the information about clinical features and radiological imaging is based on anecdotal case reports.
Diagnosis requires a suggestive history and radiology and is confirmed by histopathological evidence of caseating granulomas in the tissue or acid-fast bacilli (AFB) in smear and culture. Polymerase chain reaction (PCR) is emerging as the investigation of choice in patients with ocular TB, because of faster results and requirement of a smaller sample. It can be used in the tissue obtained from the skin of the eyelid, conjunctiva, vitreous and choroid. However, the sensitivity and specificity of PCR for the diagnosis of ocular TB have not been studied in large studies.[4] It is difficult to diagnose intraocular TB as the sensitivity of culture or PCR for the detection of Mtb in intraocular fluids is low.[6] Moreover, it is difficult to obtain a biopsy from the retina, choroid and optic nerve. The disease being paucibacillary, AFB are seen rarely in stained smears. The Mantoux test is an important ancillary test in suspected patients as it tells about infection with Mtb. However, it gives false- negative results in 30% of patients with active TB.[6] Besides, it has limited sensitivity in patients with immunosuppression.
There are no standard guidelines for the treatment of ocular TB. Various studies have described the use of ATT for 6-18 months, with variable results. The use of steroids in combination with ATT is also controversial. Kee et al. did a meta-analysis of 28 studies to analyse the efficacy of ATT in patients with intraocular TB.[7] They found that the difference in outcome between patients treated with ATT alone and those treated with ATT with systemic steroids was minimal. In addition, 84% of patients treated with ATT had no recurrence of inflammation. ATT can be prescribed along with oral steroids in patients with TB uveitis to control inflammation and reduce macular oedema.[3] Various studies have been done in the past for supplementary topical use of ATT along with systemic therapy, mainly in patients with external or appendage disease. The use of rifampicin, isoniazid and streptomycin has been evaluated but they are no longer recommended.[8] It is recommended to follow the RNTCP-based regimen for extrapulmonary TB. In certain cases of orbital TB, surgical intervention is required along with ATT.
The diagnosis of ocular TB requires a high index of suspicion and a multidisciplinary team with an ophthalmologist and a pulmonologist. Since no clinical or radiological features are characteristic, the diagnosis has to be made on the basis of a suggestive history, radiological features and the results of the Mantoux test. In certain instances, the response to ATT confirms the presumptive diagnosis. In our patient, as there was no bacteriological confirmation, the diagnosis was based on clinico- radiological features, with a positive history of contact and a suggestive histology. The delay in diagnosis of around 6 months (before reporting to our centre) perhaps proved to be detrimental to the child.
Conclusion
Akin to TB elsewhere, ocular TB can present in many ways. The symptoms can be non-specific and atypical; thus, a high index of suspicion is required for diagnosis, especially in a TB endemic country such as India. This case highlights that TB should be ruled out in patients with ocular symptoms, as early diagnosis and prompt treatment provides a better outcome and prevents long- term sequelae.
Conflicts of interest. None declared
| 1. | India TB report 2018, Revised National TB Control Programme Annual Status Report. Available at https://tbcindia.gov.in/showfile.php?lid=3314 (accessed on 6 Jun 2018). [Google Scholar] |
| 2. | De Benedetti ZM, Carranza LB, Gotuzzo HE, Rolando CI. Ocular tuberculosis. Rev Chilena Infectol 2007;24:284-95. [Google Scholar] |
| 3. | Gupta V, Gupta A, Arora S, Bambery P, Dogra MR, Agarwal A. Presumed tubercular serpiginous like choroiditis: Clinical presentations and management. Ophthalmology 2003;110:1744-9. [Google Scholar] |
| 4. | Thompson MJ, Albert DM. Ocular tuberculosis. Arch Ophthalmol 2005;123:844-9. [Google Scholar] |
| 5. | van Assen S, Lutterman JA. Tuberculous dacryoadenitis: A rare manifestation of tuberculosis. Neth J Med 2002;60:327-9. [Google Scholar] |
| 6. | Alvarez GG, Roth VR, Hodge W. Ocular tuberculosis: Diagnostic and treatment challenges. Int J Infect Dis 2009;13:432-5. [Google Scholar] |
| 7. | Kee AR, Gonzalez-Lopez JJ, Al-Hity A, Gupta B, Lee CS, Gunasekeran DV, et al Anti-tubercular therapy for intraocular tuberculosis: A systematic review and meta- analysis. Surv Ophthalmol 2016;61:628-53. [Google Scholar] |
| 8. | Kratka WH. Isoniazid and ocular tuberculosis; an evaluation of experimental and clinical studies. Arch Ophthalmol 1955;54:330-44. [Google Scholar] |
Fulltext Views
1,620
PDF downloads
270




