Translate this page into:
Removing highly hazardous pesticides from Indian agriculture will reduce suicides
Corresponding Author:
Leah Utyasheva
QMRI E3.20, 47 Little France Cres, Edindurgh EH16 4TJ
UK
lutyasheva@gmail.com
| How to cite this article: Utyasheva L, Eddleston M. Removing highly hazardous pesticides from Indian agriculture will reduce suicides. Natl Med J India 2018;31:317-318 |
We read with interest Dr Jacob’s article on suicide in India.[1] We agree with his holistic public health and socioeconomic view of the reasons for suicide. However, we believe that there is one key approach that will rapidly reduce the number of suicides occurring in India, i.e. to regulate sale and distribution of pesticides by removing highly hazardous pesticides (HHPs) from Indian agriculture.
Pesticide self-poisoning is a major issue in India. According to official statistics, 10.9% (14 352) of 131 666 suicides in 2014 were due to insecticide poisoning.[2] This is likely to be an underestimate of poisoning with any pesticide—a national survey estimated that 38.8% (72 500) of 187 000 Indian suicides in 2010 resulted from ingestion of pesticides.[3]
Restricting supply of pesticides is an effective approach to suicide prevention.[4] Implementation of legislation to limit the use of HHPs has been highly successful in reducing overall suicide numbers in countries such as Sri Lanka, South Korea and Bangladesh, where small-scale farming is common.[5]
The best evidence comes from Sri Lanka. After the introduction of HHPs into small-scale rural agricultural practice in the 1960s, the suicide rate among those above 8 years of age increased from 5/100 000 in the 1960s to 57/100 000 population in 1995.[6] The pesticide registrar started banning HHPs (parathion and methyl parathion) in 1984 and in 1995 all WHO Class I toxicity pesticides were banned.[7] There was a sudden, rapid fall in numbers of total suicides [Figure - 1]. Subsequent ban in 1998 of the WHO Toxicity Class II pesticides such as endosulfan, dimethoate, fenthion and paraquat (in 2008-2011) led to major reductions in case fatality for pesticide poisoning and suicides.[8],[9],[10] The present overall suicide rate is 17/100 000—a 70% reduction over 20 years—and continues to fall.
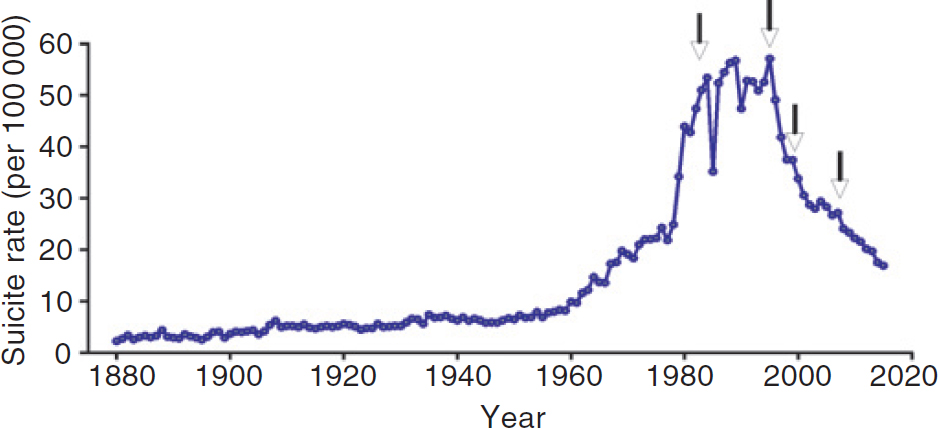 |
| Figure 1: Incidence of all suicides in Sri Lanka, 1880-2015. The arrows indicate the timing of pesticide bans (1984: parathion, methyl parathion; 1995: all remaining WHO Class I toxicity pesticides, including methamidophos and monocrotophos; 1998: endosulfan; 2008: dimethoate, fenthion and paraquat). Data obtained from police records.[6] |
Pesticide self-poisoning has become safer in Sri Lanka by allowing people to survive impulsive episodes of self-poisoning and offering psychosocial, economic or medical support they need. A few have switched to other lethal means, such as hanging, but the increase has been small and has not compensated for the major fall in the number of suicides due to pesticides.[8] This reduction has been obtained without any apparent effect on agricultural output[11] and at modest direct cost to the government (about US$ 50 per life saved).[6]
India has instituted extensive measures such as regulation of pesticides and banning multiple HHPs; but their effect is not yet visible. It is essential to urgently identify the pesticides that are causing most deaths across India as well as their effect on agricultural output. This will help in reviewing the effectiveness of the regulation.
As described by Dr Jacob, effective suicide prevention requires a comprehensive strategy that works at the patient, community and national levels. Pesticide regulations and improved health and mental healthcare need to be accompanied by measures such as protection from discrimination, efforts aimed at greater gender and social justice and ethical news reporting. The government needs to recognize the issue of suicides to protect the right to life and right to health of its population. This will help India achieve its Sustainable Development Goals.
Conflicts of interest. None declared
| 1. | Jacob KS. Suicide in India: Part perceptions, partial insights, and inadequate solutions. Natl Med J India 2017;30:155-8. [Google Scholar] |
| 2. | National Crime Records Bureau. Accidental deaths and suicides in India: 2014. New Delhi:Ministry of Home Affairs; 2015. [Google Scholar] |
| 3. | Patel V, Ramasundarahettige C, Vijayakumar L, Thakur JS, Gajalakshmi V, Gururaj G, et al. Suicide mortality in India: A nationally representative survey. Lancet 2012;379:2343-51. [Google Scholar] |
| 4. | Fleischmann A, Arensman E, Berman A, Carli V, De Leo D, Hadlaczky G, et al. Overview evidence on interventions for population suicide with an eye to identifying best-supported strategies for LMICs. Glob Ment Health (Camb) 2016;3:e5. [Google Scholar] |
| 5. | Gunnell D, Knipe D, Chang SS, Pearson M, Konradsen F, Lee WJ, et al. Prevention of suicide with regulations aimed at restricting access to highly hazardous pesticides: A systematic review of the international evidence. Lancet Glob Health 2017;5: e1026-37. [Google Scholar] |
| 6. | Knipe DW, Gunnell D, Eddleston M. Preventing deaths from pesticide self-poisoning- learning from Sri Lanka’s success. Lancet Glob Health 2017;5:e651-2. [Google Scholar] |
| 7. | Pearson M, Zwi AB, Buckley NA, Manuweera G, Fernando R, Dawson AH, et al. Policymaking ‘under the radar’: A case study of pesticide regulation to prevent intentional poisoning in Sri Lanka. Health Policy Plan 2015;30:56-67. [Google Scholar] |
| 8. | Gunnell D, Fernando R, Hewagama M, Priyangika WD, Konradsen F, Eddleston M, et al. The impact of pesticide regulations on suicide in Sri Lanka. Int J Epidemiol 2007;36:1235-42. [Google Scholar] |
| 9. | Knipe DW, Chang SS, Dawson A, Eddleston M, Konradsen F, Metcalfe C, et al. Suicide prevention through means restriction: Impact of the 2008-2011 pesticide restrictions on suicide in Sri Lanka. PLoS One 2017;12:e0172893. [Google Scholar] |
| 10. | Roberts DM, Karunarathna A, Buckley NA, Manuweera G, Sheriff MH, Eddleston M, et al. Influence of pesticide regulation on acute poisoning deaths in Sri Lanka. Bull World Health Organ 2003;81:789-98. [Google Scholar] |
| 11. | Manuweera G, Eddleston M, Egodage S, Buckley NA. Do targeted bans of insecticides to prevent deaths from self-poisoning result in reduced agricultural output? Environ Health Perspect 2008;116:492-5. [Google Scholar] |
Fulltext Views
951
PDF downloads
317




