Translate this page into:
Renal replacement therapy for patients suffering from multiple Asian giant hornet stings: A retrospective study
2 Department of Medical Education, Xi’an Jiaotong University Health Science Center, 3201 Hospital, Hanzhong, 723000, Shaanxi, China
Corresponding Author:
Zheng Liu
Department of Medical Education, Xi’an Jiaotong University Health Science Center, 3201 Hospital, Hanzhong, 723000, Shaanxi
China
boyang1996@gmail.com
| How to cite this article: Zhao M, Zhai Y, Li Y, Liu T, Li X, Liu Z. Renal replacement therapy for patients suffering from multiple Asian giant hornet stings: A retrospective study. Natl Med J India 2020;33:15-18 |
Abstract
Background. From June 2013 to June 2018, patients suffering from Asian giant hornet stings were treated with renal replacement therapy (RRT) in our hospital. We analysed the efficacy of different modalities of RRT in these patients.Methods. A comprehensive clinical history was recorded and a complete physical examination was done for each patient. Three different treatment plans were used in these patients according to the acute physiology and chronic health evaluation (APACHE) II score. These were: (i) haemoperfusion (HP) and intermittent haemodialysis (IHD); (ii) HP and continuous veno-venous haemofiltration (CVVH); and (iii) HP, CVVH and plasma exchange (PE).
Results. The average time of RRT was shorter in HP and CVVH or HP, CVVH and PE groups than in the HP and IHD group, and the patients who received HP and CVVH or HP, CVVH and PE had lower levels of blood urea nitrogen and serum creatinine after RRT for 7 days.
Conclusion. Our study suggests that HP and CVVH or HP, CVVH and PE are effective treatments for patients suffering from Asian giant hornet stings, who require RRT.
Introduction
Asian giant hornet (Vespa mandarinia) is the world's largest wasp and some queens reach more than 50 mm in length. In 2016, we reported a large case series of Asian giant hornet stings in the the southern part of Shaanxi province, China.[1] In that incident, the Asian giant hornet injured 1675 people and killed 42. The reactions to Asian giant hornet stings range from mild local reactions such as pain, oedema and erythema to fatal systemic complications such as acute kidney injury (AKI), acute toxic hepatitis and acute toxic myocarditis. Renal biopsies in such patients with AKI usually show acute interstitial nephritis.[2] In recent years, deaths due to renal failure after AKI have been reported around the world.[3] From June 2013 to June 2018, a total of 885 patients with Asian giant hornet sting were admitted to our hospital. Among these patients, 271 had AKI and 52 of them received renal replacement therapy (RRT). We did a retrospective analysis to evaluate the results of the three different treatment plans used for these patients: (i) haemo-perfusion (HP)+intermittent haemodialysis (IHD); (ii) HP+ continuous veno-venous haemofiltration (CVVH); and (iii) HP+ CVVH+plasma exchange (PE).
Methods
Patients
The patients received appropriate care including removal of the stings and oral methyl prednisolone at the time of admission to our hospital [Figure - 1]a. The diagnosis of AKI, according to Chinese guidelines on the diagnosis and treatment of AKI, included abnormally high levels of blood urea nitrogen (BUN) and serum creatinine (SCr), along with anuria (<100 ml/day) or oliguria (100–400 ml/day) and abnormal urine tests (proteinuria and haematuria). The Chinese guidelines for the diagnosis of AKI refer to KD1GO clinical guideline. AKI can be defined as one of the following: (i) increase in SCr by ≥0.3 mg/dl (≥26.5 μmol/L) within 48 h; (ii) increase in SCr to ≥1.5 times baseline, which is known or presumed to have occurred within the previous 7 days; and (iii) urine volume <0.5 ml/kg/h for 6 hours. All 52 patients had oliguria (urine volume <0.5 ml/kg/hour for 6 hours) and were treated with RRT. The patients received different RRT modalities depending on their acute physiology and chronic health evaluation (APACHE) II score: (i) ≥7: HP+IHD; (ii) ≥7 with one organ damage (liver, kidney or heart) and AKI <12 hours: HP+CVVH; and (iii) ≥7 with AKI ≥12 hours with at least two organs damage: HP+CVVH+PE.
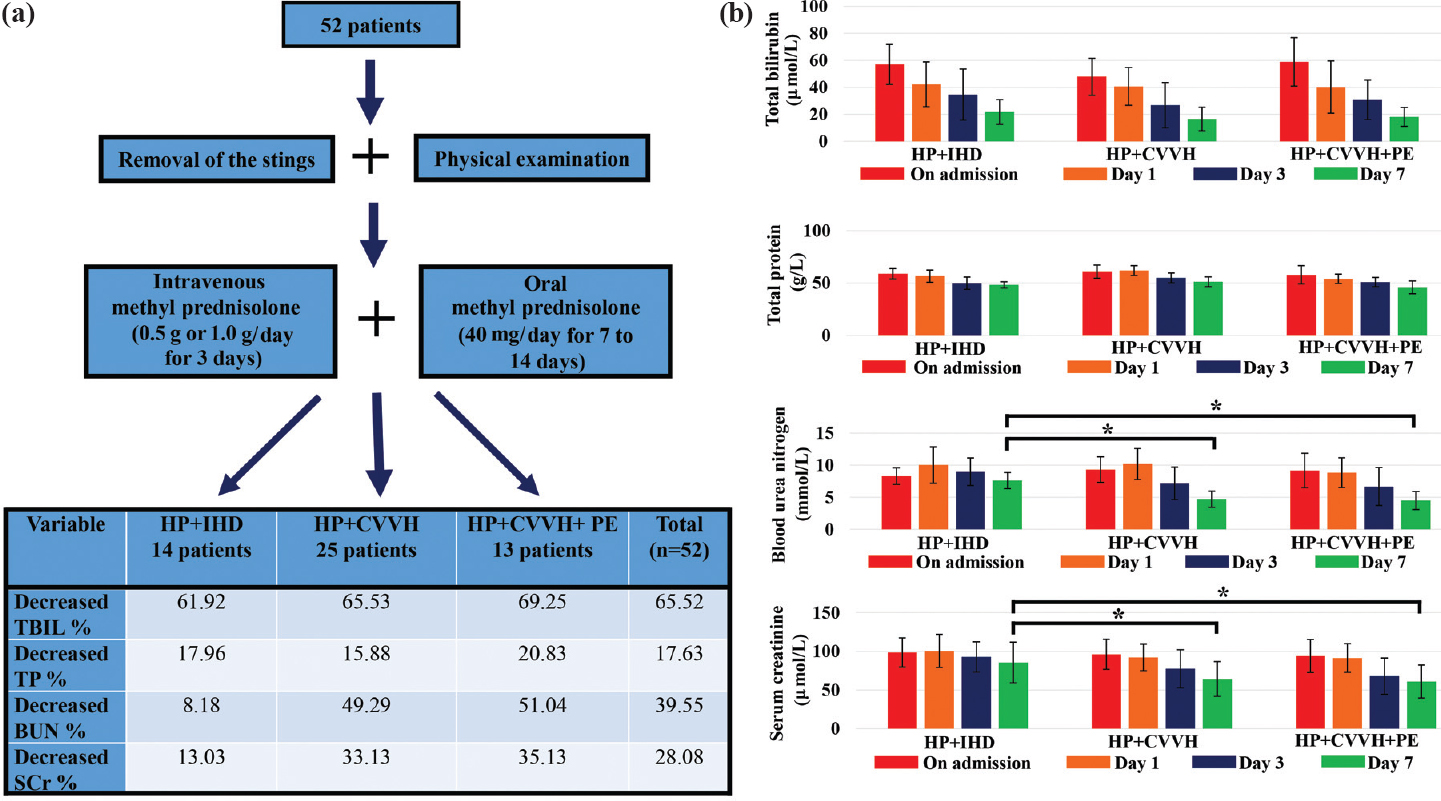 |
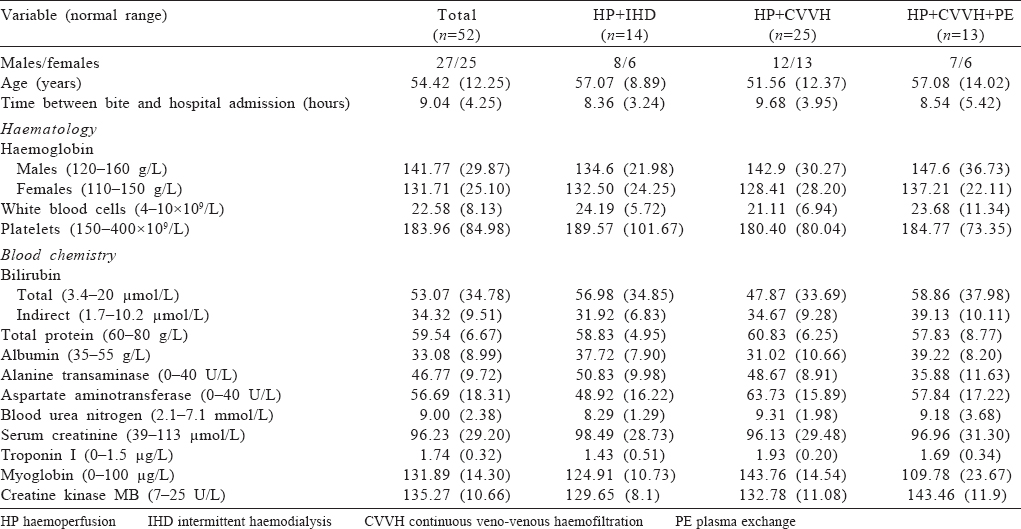
| Figure 1: (a) Workflow diagram of the process in this study. The decrease of total bilirubin (TBIL), total protein (TP), blood urea nitrogen (BUN) and serum creatinine (SCr) presented as the percentage to the concentration of each substrate on admission; (b) The changes in the biochemical measures in the three groups: total bilirubin (μmol/L), total protein (g/L), blood urea nitrogen (mmol/L) and serum creatinine (μmol/L) HP haemoperfusion IHD intermittent haemodialysis CVVH continuous veno-venous haemofiltration PE plasma exchange |
Clinical data collection
Patients’ demographic characteristics such as age, sex and disease history were recorded [Table - 1]. The appropriate investigations such as BUN, serum creatinine, white blood cells (WBC), haemoglobin, platelet count (PLT), total bilirubin (TBIL), indirect bilirubin, total protein (TP), albumin, alanine transaminase, aspartate aminotransferase, troponin I, myoglobin (Mb) and creatine kinase MB, were also recorded. Informed consent was obtained from all patients. The study was approved by the institutional review board of Xi’an Jiaotong University. All procedures performed in this study involving human participants were in accordance with the Helsinki Declaration of 1975, as revised in 2008.
Observation of clinical course and renal outcomes
- HP+IHD group: The treatment was done three times per week for 4 hours per session with a blood flow rate of 200–250 ml/minute and a Kt/V ratio of 1.2–1.4.
- HP+CVVH group: The treatment was done using pre-dilution bicarbonate replacement fluid at a rate of 30–35 ml/kg/hour with a blood flow rate of 150–200 ml/minute.
- HP+CVVH+PE group: These patients received HP+PE once daily on day 1 and day 2 with a 2000–2500 ml exchange volume each time using fresh-frozen plasma.
The RRT was stopped when the urine output was ≥1500 ml/day without fluid overload, and there was a decrease in the serum TBIL, TP, BUN and SCr level to within normal range. The time of RRT, causes of death and changes in important laboratory measures (WBC, PLT, TBIL, TP, BUN and SCr) were recorded. Patients were followed up for 1 month after the RRT.
Statistical analyses
The results are presented as mean (SD) and percentages. The one-way analysis of variance and post hoc Tukey test was used for group comparisons. All analyses were implemented using SPSS 16.0 for Windows. All data were checked for normal distribution before statistical analysis. A p value <0.05 was considered significant.
Results
General characteristics
There was no significant difference in WBC, PLT, TBIL, TP, BUN and SCr in these three groups at admission.
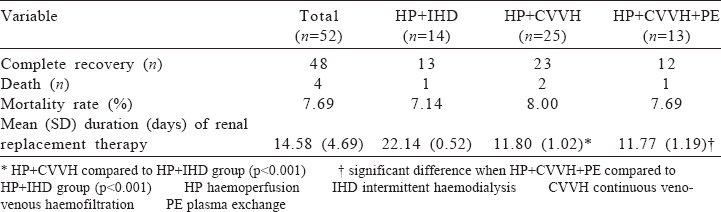
Survival and time of RRT
Of the 52 patients, 4 patients died (mortality rate 7.7%). The cause of death was disseminated intravascular coagulation in 1, acute left heart failure in 1 and laryngeal oedema with acute respiratory distress syndrome in 2. The average treatment time for the HP+CVVH and HP+CVVH+PE groups was 11.80 and 11.77 days, respectively. The HP+IHD group received an average of 22.14 days of dialysis sessions. Compared with the HP+IHD group, the time for RRT was significantly shorter in the HP+CVVH and HP+CVVH+PE groups [Table - 2]. At 1 month after RRT, the kidney function recovered completely in all the survivors (92.3%) as per the Chinese guidelines on diagnosis and treatment of AKI.
Changes in biochemical measures
The decrease of TBIL, TP, BUN and SCr is shown in [Figure - 1]a. As shown in [Figure - 1]b, serum levels of TBIL and BUN decreased steadily through the first week of the treatment. The three groups did not show any difference in TBIL and TP levels on day 7. However, subgroup analysis showed that the HP+IHD group had a higher level of BUN and SCr than the other two groups on day 7.
Discussion
In the southern part of China, Asian giant hornet poisoning takes a heavy death toll annually. As one of the three regional central hospitals in the southern part of Shaanxi province, we established a standard treatment protocol for patients suffering from Asian giant hornet sting. Briefly, the local treatment is removal of the stings left in the skin. Early application of intravenous methyl prednisolone pulse therapy (0.5 g or 1 g/day for 3 days) combined with conventional methyl prednisolone (40 mg/day for 7–14 days) were used in the clinical treatment of patients with severe reactions such as severe allergic reactions, severe haemolysis and rhabdomyolysis [Figure - 1]a. At the same time, RRT was used as early as possible for patients who met the treatment criteria. These treatment plans combined with timely and appropriate supportive management, such as providing efficient and effective nursing care and giving proper clinical services. The other treatment included intravenous fluids, prophylactic antibiotics, oxygen and symptomatic measures.
To the best of our knowledge, there is no standard treatment guideline for Asian giant hornet stings. In an earlier report, HP has proved to be highly effective for the treatment of snake bites in emergency situations.[4] It especially targets small-to medium-sized molecules by removing drugs or poisons from the blood and waste products from the blood.[5],[6] We believed that HP was advantageous in clearing the venom components of the Asian giant hornet and the inflammatory mediators in circulating blood. Therefore, it was used for all of our patients. In our study, patients started with HP+CVVH and HP+CVVH+PE experienced a shorter time of RRT compared with those initiated with HP+IHD. This difference might relate to patients with a poor haemodynamic tolerance to IHD.[7],[8] Compared with IHD, PE provided a more effective clearance of some substances with a large molecular weight.[9] According to previous reports, most components of wasp and bee venoms are large molecules. For example, Mb is the ‘secondary toxin’ produced by rhabdomyolysis following wasp stings and has a molecular mass of 17 800 D.[10] Melittin, one of the main components of bee venom in Apis mellifera is a 2800 D toxic peptide.[11] Antigen 5 and PLA1 are two main components of wasp venom and have larger molecular masses of 23 000 and 43 000 D, respectively.[12] Theoretically, PE could remove these large molecular toxins more effectively than IHD. CVVH is provided as a continuous 24 hours/day therapy. The major advantage of CVVH is providing slow and balanced fluid removal for patients with shock or severe fluid overload.[13],[14] Thus, CVVH is generally better tolerated than IHD since many of the complications of IHD are related to the rapid rate of solute and fluid loss.[15],[16]
Conclusion
Our case series reports the outcomes of patients following multiple Asian giant hornet stings. Most patients had a complete recovery of kidney function. Patients administered HP+CVVH or HP+CVVH+PE had RRT for a shorter time than those administered HP+IHD. The reasons for this observation are unclear. Further studies are required to elucidate the mechanism for the differences between these modified RRTs. In particular, investigating the composition of Asian giant hornet venom can help us understand this mechanism better.
Acknowledgements
This work was supported by the key research and development program of Shaanxi Province (2017ZDXM-SF-067) and Natural Science Foundation of Guangxi Province (2018JJA140045).
Conflicts of interest. None declared
| 1. | Liu Z, Li XD, Guo BH, Li Y, Zhao M, Shen HY, et al. Acute interstitial nephritis, toxic hepatitis and toxic myocarditis following multiple Asian giant hornet stings in Shaanxi province, China. Environ Health Prev Med 2016;21:231–6. [Google Scholar] |
| 2. | Li XD, Liu Z, Zhai Y, Zhao M, Shen HY, Li Y, et al. Acute interstitial nephritis following multiple Asian giant hornet stings. Am J Case Rep 2015;16:371–3. [Google Scholar] |
| 3. | Mulay AV. Renal failure deaths in India: Crying for attention. Natl Med J India 2017;30:148–9. [Google Scholar] |
| 4. | Yildirim C, Bayraktaroðlu Z, Gunay N, Bozkurt S, Köse A, Yilmaz M. The use of therapeutic plasmapheresis in the treatment of poisoned and snake bite victims: An academic emergency department's experiences. J Clin Apher 2006;21:219–23. [Google Scholar] |
| 5. | Si X, Li J, Bi X, Wu L, Wu X. Clinical evaluation of high-volume hemofiltration with hemoperfusion followed by intermittent hemodialysis in the treatment of acute wasp stings complicated by multiple organ dysfunction syndrome. PLoS One 2015;10:e0132708. [Google Scholar] |
| 6. | Shang AD, Lu YQ. A case report of severe paraquat poisoning in an HIV-positive patient: An unexpected outcome and inspiration. Medicine (Baltimore) 2015;94:e587. [Google Scholar] |
| 7. | Schortgen F, Soubrier N, Delclaux C, Thuong M, Girou E, Brun-Buisson C, et al. Hemodynamic tolerance of intermittent hemodialysis in critically ill patients: Usefulness of practice guidelines. Am J Respir Crit Care Med 2000;162:197–202. [Google Scholar] |
| 8. | Chimot L, Gacouin A, Nardi N, Gros A, Mascle S, Marqué S, et al. Can we predict poor hemodynamic tolerance of intermittent hemodialysis with echocardiography in intensive care patients? J Ultrasound Med 2014;33:2145–50. [Google Scholar] |
| 9. | Pons-Estel GJ, Salerni GE, Serrano RM, Gomez-Puerta JA, Plasin MA, Aldasoro E, et al. Therapeutic plasma exchange for the management of refractory systemic autoimmune diseases: Report of 31 cases and review of the literature. Autoimmun Rev 2011;10:679–84. [Google Scholar] |
| 10. | Naka T, Jones D, Baldwin I, Fealy N, Bates S, Goehl H, et al. Myoglobin clearance by super high-flux hemofiltration in a case of severe rhabdomyolysis: A case report. Crit Care 2005;9:R90–5. [Google Scholar] |
| 11. | Terra RM, Guimarães JA, Verli H. Structural and functional behavior of biologically active monomeric melittin. J Mol Graph Model 2007;25:767–72. [Google Scholar] |
| 12. | King TP, Spangfort MD. Structure and biology of stinging insect venom allergens. Int Arch Allergy Immunol 2000;123:99–106. [Google Scholar] |
| 13. | Passos RD, Ramos JG, Gobatto A, Mendonça EJ, Miranda EA, Dutra FR, et al. Lactate clearance is associated with mortality in septic patients with acute kidney injury requiring continuous renal replacement therapy: A cohort study. Medicine (Baltimore) 2016;95:e5112. [Google Scholar] |
| 14. | Putzu A, Fang MX, Boscolo Berto M, Belletti A, Cabrini L, Cassina T, et al. Blood purification with continuous veno-venous hemofiltration in patients with sepsis or ARDS: A systematic review and meta-analysis. Minerva Anestesiol 2017;83:867–77. [Google Scholar] |
| 15. | Palevsky PM. Renal replacement therapy in acute kidney injury. Adv Chronic Kidney Dis 2013;20:76–84. [Google Scholar] |
| 16. | Payette A, Ghannoum M, Madore F, Albert M, Troyanov S, Bouchard J, et al. Carbamazepine poisoning treated by multiple extracorporeal treatments. Clin Nephrol 2015;83:184–8. [Google Scholar] |
Fulltext Views
1,458
PDF downloads
177




