Translate this page into:
Lichen scrofulosorum and phlyctenular conjunctivitis
2 Department of Dermatology, Lady Hardinge Medical College and Associated Hospitals, University of Delhi, New Delhi, India
3 Department of Pathology, Lady Hardinge Medical College and Associated Hospitals, University of Delhi, New Delhi, India
Corresponding Author:
Siddharth Madan
Department of Ophthalmology, Lady Hardinge Medical College and Associated Hospitals, University of Delhi, New Delhi
India
drsiddharthmadan@gmail.com
| How to cite this article: Madan S, Beri S, Sethi M, Garg T, Nangia A. Lichen scrofulosorum and phlyctenular conjunctivitis. Natl Med J India 2021;34:58-59 |
Phlyctens of the conjunctiva are mostly asymptomatic.[1] Tuberculosis (TB) is the underlying aetiology in 77% of phlyctenular kerato-conjunctivitis (PKC) cases in India.[2] Phlyctenular conjunctivitis (PC) due to underlying tubercular origin usually responds well to antitubercular treatment (ATT).[3] Lichen scrofulosorum (LS) represents the most common tuberculid in children, yet it remains under-reported and under-diagnosed. It results due to a delayed-type hypersensitivity reaction to Mycobacterium tuberculosis. A 12-year-old boy was referred with redness in the left eye (LE) for 5 days [Figure - 1]a,[Figure - 1]b,[Figure - 1]c. He presented with a 4–5 months history of progressively increasing multiple bilateral well-defined, light brown-coloured pinhead-sized papules over the upper and lower limbs (bilaterally), neck, groin and trunk. Some of these were grouped to form ill-defined plaques with xerosis [Figure - 1]d,[Figure - 1]e. Most lesions had white semi-adherent scaling at their periphery.
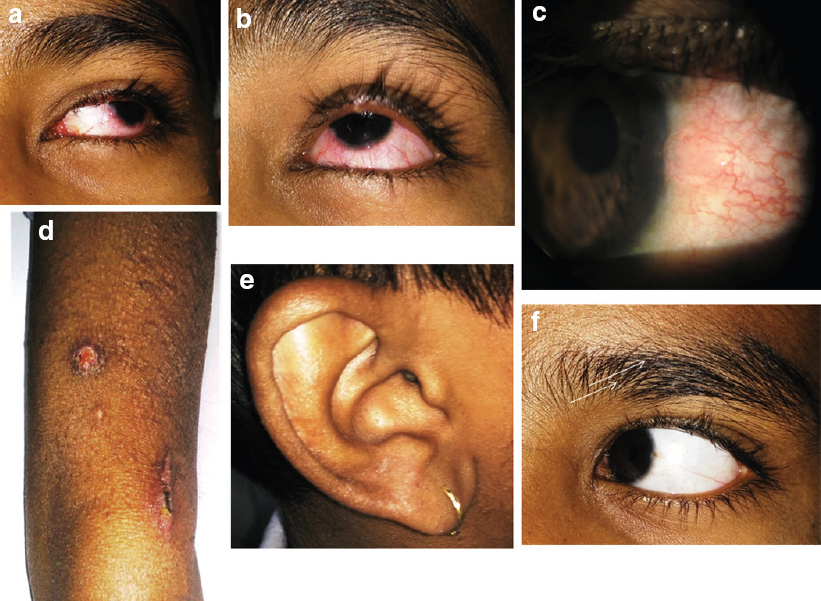 |
| Figure 1 (a-f): Sequential patient photographs. The child presented with redness and congestion in the left eye (a and b) with a pinkish nodule over the temporal limbus suggestive of phlycten (c). Pinhead-sized raised papular lesions over bilateral arms (thin white arrow, (d) along with nodular elevated annular lesions with exudation suggestive of tinea corporis over the arm at places. Ill-defined plaque was observed over the ear (e). Phlycten regressed with treatment (f) |
The child had developed intermittent high-grade fever with characteristic evening rise 2 years ago without any accompanying localizing symptoms. Two months following the onset of fever, his mother noticed these skin lesions. The child also had non-productive cough accompanied with fever of similar nature for 2 months before he presented at the clinic. He had been treated for pulmonary TB with ATT for 11 months when he was 5 years old. The family history had no points relevant to his present condition. At presentation, he had bilateral, multiple, non-matted submandibular lymph nodes (LN), and a 1 cm×1 cm supraclavicular LN on the left side. These lymph nodes were neither clinically significant nor was fine-needle aspiration cytology feasible from them. A biopsy from the skin lesion showed keratotic plugging of the stratified squamous epithelial lining [Figure - 2]a,[Figure - 2]b and epithelioid cell granuloma containing giant cells in the dermis [Figure - 2]b,[Figure - 2]c. There were lymphocytes seen in the superficial dermis and around eccrine glands, which was suggestive of LS. A few fungal hyphae were also seen on a potassium hydroxide mount from skin lesions over the arms and legs, which was suggestive of tinea corporis. Mantoux test was strongly positive with induration of 26 mm×28 mm. His haemoglobin was 12.5 g/dl and the erythrocyte sedimentation rate was 33 mm. He tested negative for human immunodeficiency virus. Chest X-ray suggested left paratracheal lymphadenopathy, but there was no evidence of miliary TB. On computed tomography, none of the left paratracheal LN were over 10 mm. Gastric aspirate for acid-fast bacilli (AFB) along with gene expert was negative. Ultrasound of the abdomen revealed multiple enlarged mesenteric LN with conglomeration, some showing necrosis and the largest LN measured 15 mm. The thickness of the ileo-caecal junction was 6 mm. Category 2 ATT was started after consulting a paediatrician. Topical antifungal (terbinafine) ointment was prescribed. The redness in his left eye just next to the temporal limbus was diagnosed as PC [Figure - 1]a and [Figure - 1]c. Topical fluorometholone and tobramycin eye drops were instilled three times a day. After 2 weeks of treatment, the skin lesions had started to heal, and the phlycten had regressed [Figure - 1]f.
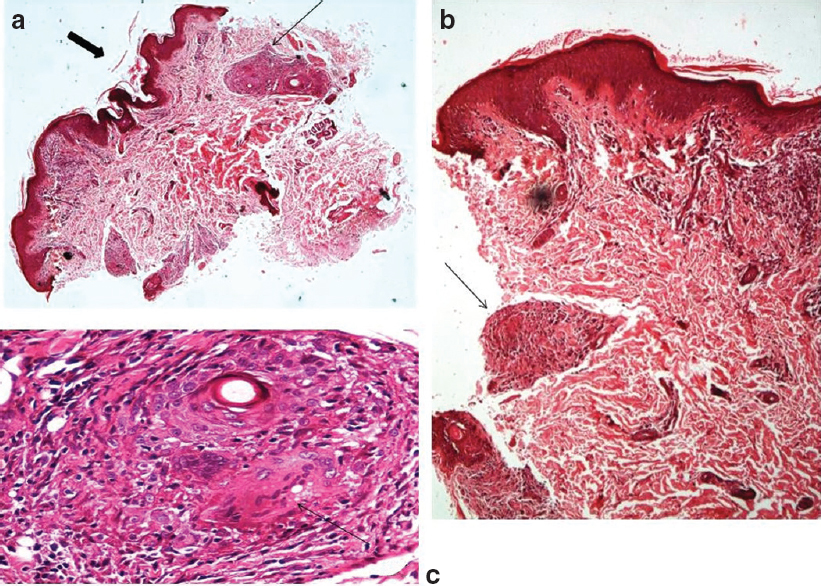 |
| Figure 2 (a-c): Histopathology pictures suggestive of lichen scro-fulosorum. A biopsy from skin lesions demonstrated keratotic plugging of the stratified squamous epithelial lining of the skin (a [bold arrow; H and E, *10], b) along with granuloma in the dermis with giant cells (a-c [thin arrow]; (b: H and E, *40) and lymphocytes in the superficial dermis (c: H and E, *100) |
The annual incidence of TB in children is 0.26 million resulting in 8.9% of cumulative incidence.[4] Cutaneous TB accounts for 0.9% of patients presenting to dermatology clinics.[5] Children contribute to 31.7%–53.9% of skin TB, and clinical presentation resembles that seen in adults.[5] Manifestations of TB are due to direct infection with the bacteria or as a result of immunological response to its antigens, which can present as PKC, interstitial keratitis and retinal vasculitis, and may involve any ocular structure and surrounding adnexae.[6],[7] Children present commonly with PKC; however, it is sparsely reported in the literature.[8] About 1.5% of the 10% cases of extrapulmonary TB cases have dermatological involvement.[9],[10] Although histopathological features are characteristic of LS, polymerase chain reaction and culture for the bacilli are usually negative. Extrapulmonary TB does not show the characteristic clinical symptoms and imaging features, and may commonly be misdiagnosed, and hence, the initiation of treatment may be delayed. Epithelioid cell granulomas with caseous necrosis are the hallmark features of disseminated and extrapulmonary TB; however, AFB is rarely observed in these. This patient possibly had disseminated extrapulmonary TB and his response to ATT was obvious. In all children presenting with cutaneous TB, a comprehensive evaluation should be performed for underlying involvement of the eyes, LN, lungs, gastrointestinal, nervous and musculoskeletal system.[11] Relaunch of the revised national TB control program has provided better control and management of pulmonary and extrapulmonary TB in India, more importantly the escalation of the cost-effective, directly observed treatment, short course.[12]
Conflicts of interest. None declared
| 1. | Duke ES (ed). Conjunctival diseases. In: System of ophthalmology. 1st ed. London:Henry Kempton; 1977:461–75. [Google Scholar] |
| 2. | Rohatgi J, Dhaliwal U. Phlyctenular eye disease: A reappraisal. Jpn J Ophthalmol 2000;44:146–50. [Google Scholar] |
| 3. | Lahiri K, Landge A, Gahlowt P, Bhattar A, Rai R. Phlyctenular conjunctivitis and tuberculosis. Pediatr Infect Dis J 2015;34:675. [Google Scholar] |
| 4. | Bloom BR, Atun R, Cohen T, Dye C, Fraser H, Gomez GB, et al. Tuberculosis. In: Holmes KK, Bertozzi S, Bloom BR, Jha P (eds). Major infectious diseases. 3rd ed. Washington (DC):The International Bank for Reconstruction and Development/ The World Bank; 2017. Available at www.ncbi.nlm.nih.gov/books/NBK525174/ (accessed on 4 Apr 2020). [Google Scholar] |
| 5. | Kumar B, Kumar S. Pediatric cutaneous tuberculosis: Indian scenario. Indian J Paediatr Dermatol 2018;19:202–11. [Google Scholar] |
| 6. | Chuka-Okosa CM. Tuberculosis and the eye. Niger J Clin Pract 2006;9:68–76. [Google Scholar] |
| 7. | Egbagbe EE, Omoti AE. Ocular disorders in adult patients with tuberculosis in a tertiary care hospital in Nigeria. Middle East Afr J Ophthalmol 2008; 15:73–6. [Google Scholar] |
| 8. | Pandhi D, Reddy BS, Chowdhary S, Khurana N. Cutaneous tuberculosis in Indian children: The importance of screening for involvement of internal organs. J Eur Acad Dermatol Venereol 2004;18:546–51. [Google Scholar] |
| 9. | Grosset JH. Present status of chemotherapy for tuberculosis. Rev Infect Dis 1989;11 (Suppl 2):S347–52. [Google Scholar] |
| 10. | Singal A, Aggarwal P, Pandhi D, Rohatgi J. Cutaneous tuberculosis and phlyctenular keratoconjunctivitis: A forgotten association. Indian J Dermatol Venereol Leprol 2006;72:290–2. [Google Scholar] |
| 11. | Rauschkolb JE. Tuberculosis of the skin: A clinical report. Arch Derm Syphilol 1934;29: 398–407. [Google Scholar] |
| 12. | Mandal S, Chadha VK, Laxminarayan R, Arinaminpathy N. Counting the lives saved by DOTS in India: A model-based approach. BMC Med 2017;15:47. [Google Scholar] |
Fulltext Views
1,920
PDF downloads
263




