Translate this page into:
Access to healthcare among the Empowered Action Group (EAG) states of India: Current status and impeding factors
Corresponding Author:
Virendra Kumar
Department of Humanities and Social Sciences, Indian Institute of Technology Roorkee, Roorkee 247667, Uttarakhand
India
kumarvirendraiitr@gmail.com
| How to cite this article: Kumar V, Singh P. Access to healthcare among the Empowered Action Group (EAG) states of India: Current status and impeding factors. Natl Med J India 2016;29:267-273 |
Abstract
Background. Access to healthcare is crucial for meeting the health needs of Indians. We explored factors impeding access to public sources of healthcare among the Empowered Action Group (EAG) states of India. We also examined the extent to which Indians depend on public and private sources of healthcare in the EAG states.Methods. Our study is based on the unit-level records of
9988 ailing persons, who were surveyed among the EAG states in the 71st round of the National Sample Survey (NSS), conducted during January-June 2014 on the theme 'Social consumption: Health'. To analyse the socioeconomic factors, we did logistic regression using STATA version 12.0.
Results. Despite a vast public health infrastructure in the EAG states, around three-fourths of inpatients are dependent on private sources of healthcare in both rural (70%) and urban (78%) areas. Poor quality and long waiting time in accessing healthcare from public health facilities remain big concerns for inpatients of the EAG states.
Conclusion. To make public health services more accessible, there is a need to improve the quality of services, enlarge infrastructure to reduce waiting time, and enhance the physical reach to inpatients in the EAG states of India. Public health services will then be able to compete with those in the private sector.
Introduction
Access to healthcare services is crucial for their optimum utilization and to meet the health needs of Indians. [1],[2],[3], [4] The population should be able to receive health services that are physically and financially accessible, affordable and acceptable for all. [2],[3] Expanding healthcare access is a priority for the Government of India to secure the fundamental human rights of it citizens. [5],[6] However, in the past two decades, the government is struggling to improve healthcare access for its citizens.
India′s healthcare system consists of a mix of public and private health service providers. [6] Regardless of the vast public health infrastructure along with several vertical health programmes, India has the largest private healthcare system in the world [4],[7],[8] with 72% of health expenditure being incurred in the private sector. [9] A dominant private sector and its high out-of-pocket payment mechanism has resulted in unequal access to healthcare and thus, unequal health outcomes among varied socioeconomic population groups. [8] The 12th Five-Year Plan seeks to support initiatives taken in the 11th Five-Year Plan to expand the reach of healthcare towards the long-term objective of setting up a system of universal access to healthcare in India. [6] It means that every individual would have assured access to health services, which should be free for a majority of the population. Though the list of assured services will have to be limited by budgetary constraints, the objective should be to increase the coverage over time. [6]
Studies show that access to healthcare in India is unequal among regions with variations such as caste and class. [4],[7],[10] Powell-Jackson et al. [11] have pointed out that accessibility to healthcare is very low among the weaker sections of society. Kanuganti et al. found accessibility to healthcare to be low in India due to inadequate availability of public transport in rural areas. [3] They also found that access to healthcare depends on travel time, travel cost, convenience and road conditions. Applications of physical accessibility to healthcare in both developed and developing countries have been carried out by Parker and Campbell, [12] Noor et al., [13] Sarkar and Ghosh [14] and Jacobs et al.[15]
We evaluated accessibility to healthcare in the Empowered Action Group (EAG) states of India (Bihar, Chhattisgarh, Jharkhand, Madhya Pradesh, Odisha, Rajasthan, Uttarakhand and Uttar Pradesh) in both public and private sectors by using dataset of the 71st round of the National Sample Survey (NSS). [16] This dataset shows the degree of access to healthcare for individuals in both rural and urban areas. Our interest in the EAG states is primarily because together these states account for about 46% of the Indian population, and 61% of the poor (those living below the poverty line). [17] The health outcomes are the worst in the EAG states, which contribute to the highest disease burden in the country. [18] Therefore, greater access to public health services is desirable if we are to meet the health needs of the population. [6],[11] We also explored the factors impeding access to public sources of healthcare in the EAG states.
Methods
Our study is based on the unit-level records of the 71st round of the National Sample Survey (NSS), which was done during January-June 2014 on the theme of ′Social consumption: Health′. [16] The survey was conducted throughout the country in both rural (consisting of 4577 villages) and urban (3720 urban blocks) areas and provides information on various aspects of healthcare. We used the information related to spells of ailment of household members (including hospitalization), which is available in the eighth block of the NSS 71st round schedule.
We specifically included the level of healthcare from where individuals were seeking medical advice after their ailment. As per the schedule, health subcentre (HSC)/auxiliary nurse midwives (ANM)/accredited social health activist (ASHA)/anganwadi workers (AWW), primary health centres (PHC)/dispensary/community health centres (CHC)/mobile medical units and government hospitals are categorized as public sources of healthcare whereas, private doctors/clinics and private hospitals are classified as private sources of healthcare. [16] HSC, ANM/ASHA and AWW are considered as the lowest level of care. However, the possibility of misclassification of these ′levels of care′ (other than public hospital) by an informant cannot be ruled out due to overlapping of these units in some states. Thus, we have combined these figures.
We analysed five reasons (given in the schedule) associated with not availing public sources of healthcare: required specific services not available, service available but quality not satisfactory, quality satisfactory but facility too far, quality satisfactory but involves long waiting time, financial constraint and others. To analyse the other socioeconomic factors, we used logistic regression using STATA version 12.0 (Stata Corp LP, College Station, TX, USA) and SPSS 20. It aims to explain the odds of the outcome variable in question by a set of factors that vary systematically with socioeconomic status. [19],[20] The parameters of the logistic regression were estimated by modelling the ′public healthcare′ variable (1 if ailing person uses public source of healthcare, 0 private/otherwise) against a set of explanatory variables such as social groups, religious groups, the EAG states, quantiles, sectors and general education level. The estimates of the model have been expressed in terms of odds. Appropriate sampling weights were used to control the complex survey design of the NSS. Sampling weights are given in the NSS dataset (see the NSS reports for the detail of sampling reference).
The ailing persons surveyed among the EAG states in the 71st round were 9988 (5661 in rural and 4327 in urban areas). Among the EAG states, around 40% of the sample was contributed by Uttar Pradesh, followed by Madhya Pradesh (14%), Odisha (13%) and Rajasthan (12%). The remaining three states (Bihar, Jharkhand and Chhattisgarh) shared <10% of the sample households. Except for Bihar, Odisha and Madhya Pradesh, the distribution of sampled persons was similar in rural and urban areas of the EAG states ([Table - 1]).

This study is based on a secondary dataset with no identifiable information on the survey participants. The National Sample Survey Office (NSSO), Government of India, provides this dataset for research purposes (available at www.mospi.gov.in/download-reports?main_cat=NzIy&cat=All&sub_category=All ).
Results
Healthcare accessibility: Public versus private
The results show that the EAG states could ensure access to public sources of healthcare to a limited population (30% rural and 22% urban; [Table - 2]). Among the EAG states, Odisha performed the best in securing access to public health services to a large proportion of inpatients in both rural (71%) and urban areas (47%), followed by Uttarakhand (61% rural and 31% urban) and Rajasthan (44% rural and 39% urban). The inpatients of Chhattisgarh also reported better accessibility (42% rural and 26% urban) to public sector facilities in comparison to Uttar Pradesh (16% rural and 14% urban) and Bihar (16% rural and 18% urban). Similarly, the results reveal that accessibility to public sources of healthcare is better in Madhya Pradesh (27% rural and 29% urban) and Jharkhand (25% rural and 20% urban) in comparison to Uttar Pradesh and Bihar.
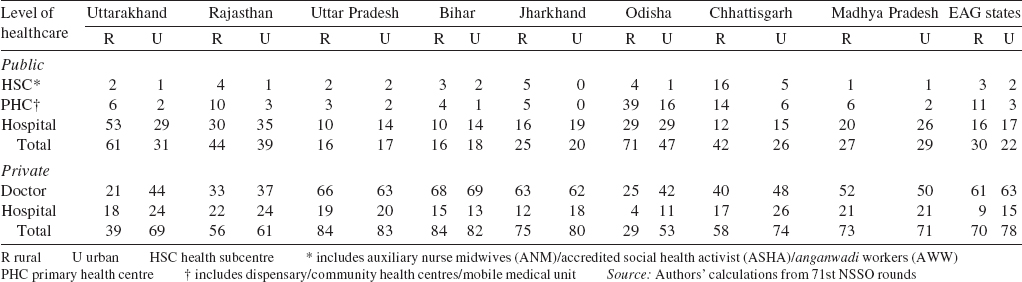
Among the public sources of healthcare, it is public hospitals from where a larger share of the inpatients are seeking medical advice in both rural (16%) and urban (17%) parts of the EAG states, in comparison to other public sources of healthcare such as PHCs and HSCs. Besides, among the EAG states, public hospitals of Rajasthan (30% rural and 35% urban), Odisha (29% rural and 29% urban) and Madhya Pradesh (20% rural and 26% urban) were found to be more accessible than other government sources of healthcare. As an exception, more than half the inpatients (53%) of rural areas of Uttarakhand are dependent especially on public hospitals followed by the PHCs (6%). Thus, public hospitals play a major role in the provisioning of health services in rural areas of Uttarakhand. Further, the inpatients of rural areas of Odisha also reported greater accessibility to public sources of healthcare especially PHCs (39%) and public hospitals (29%).
The results show that around three-fourths of inpatients in the EAG states are dependent on private sources of healthcare in both rural (70%) and urban (78%) areas ([Figure - 1]). Among the EAG states, the inpatients who reside in Uttar Pradesh (84% rural and 83% urban) and Bihar (84% rural and 82% urban) show extreme dependency on private sources of healthcare, followed by Jharkhand (75% rural and 80% urban) and Madhya Pradesh (73% rural and 71% urban). Similarly, around 60% of inpatients in Chhattisgarh and Rajasthan rely on private sector health facilities in both rural and urban areas. In addition, the inpatients of urban areas of Chhattisgarh (74%) and Uttarakhand (69%) predominantly depended on private sources of healthcare. However, inpatients residing in rural areas of Odisha (29%) and Uttarakhand (39%) are seen to be less dependent on private health facilities in comparison to the other EAG states.
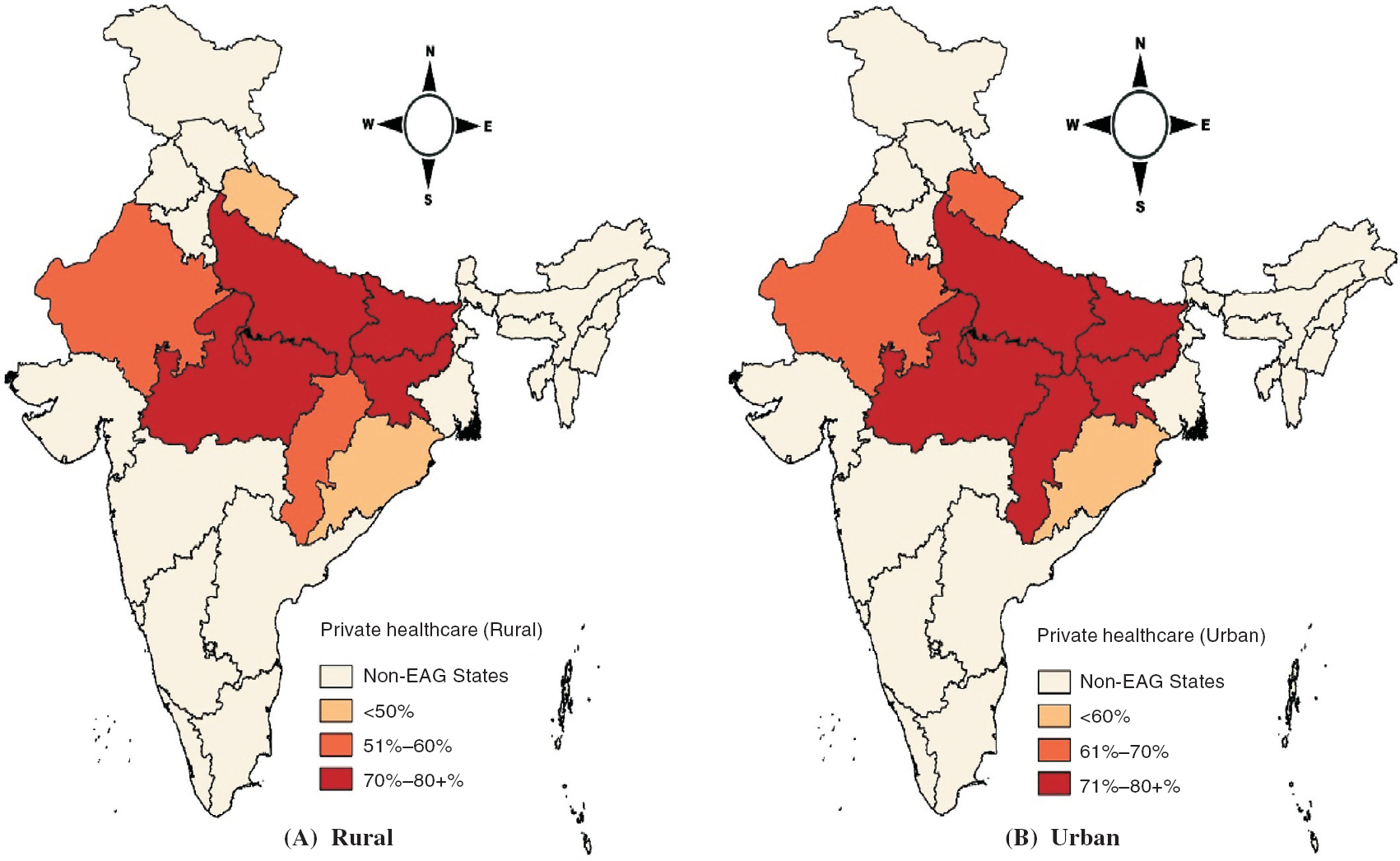 |
| Figure 1. Extent of access of private healthcare facilities in empowered action group (EAG) states |
Factors impeding access to public sources of healthcare
We found that poor quality of services remains the biggest challenge for inpatients of EAG states. Around half the inpatients (51% rural and 48% urban) of the EAG states do not access public sources of healthcare due to poor quality of services available in their areas.
Among the EAG states, Bihar (64% rural and 58% urban), Madhya Pradesh (63% rural and 51% urban) and Odisha (56% rural and 70% urban) contribute the highest proportion of inpatients who were not satisfied with the quality of public health services available in their areas. Poor quality services were also reported by around half the inpatients of Chhattisgarh (49% rural and 55% urban) and Uttar Pradesh (47% rural and 46% urban). However, the public health system of Uttarakhand delivers better quality of health services in comparison to the other EAG states ([Table - 3]).
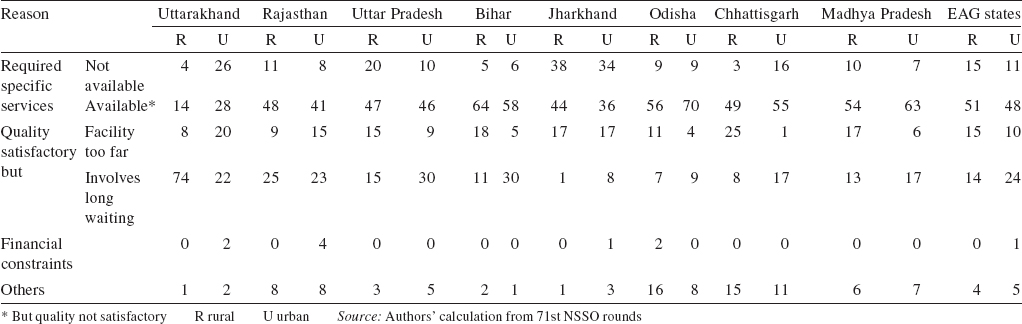
Long waiting time in seeking healthcare from public health facilities is a major public health challenge in the EAG states. A large proportion of inpatients (14% rural and 24% urban) of the EAG states do not access public sources of healthcare as they have to wait for a long time in a queue while seeking these facilities. Surprisingly, due to long waiting in public health facilities 74% of inpatients of rural areas of Uttarakhand do not access these facilities. Similarly, longer waiting time dissuades a large proportion of inpatients of urban areas of Uttar Pradesh (30%) and Bihar (30%) from accessing public health facilities.
Our results show that the EAG states have not been able to make health services available to all. A major proportion of inpatients (15% rural and 11% urban) of the EAG states could not access public sector health facilities because of the absence of required facilities in their area. Among the EAG states, the highest proportion of inpatients (38% rural and 34% urban) in Jharkhand reported non-availability of public health services. In Uttar Pradesh non-availability of public health services was reported by 20% of inpatients of rural and 10% of urban areas. The non-availability of public health services is not seen as a matter of concern in rural areas of Uttarakhand (4%) and Chhattisgarh (3%), but it has been noted as a big challenge in urban areas of both states, as reported by 26% and 16% inpatients, respectively.
We found that 15% of inpatients in rural and 10% in urban areas of the EAG states could not access public sources of healthcare due to remote location of health services. Similarly, remote location of public health facilities led to a large number of inpatients in rural areas of Chhattisgarh (25%), Bihar (18%), Madhya Pradesh (17%) and Jharkhand (17%) not reaching these facilities at the time of their health need. Hence, they accessed nearby private health facilities. Surprisingly, financial constraints were not reported as a major problem in accessing public health services among the EAG states of India.
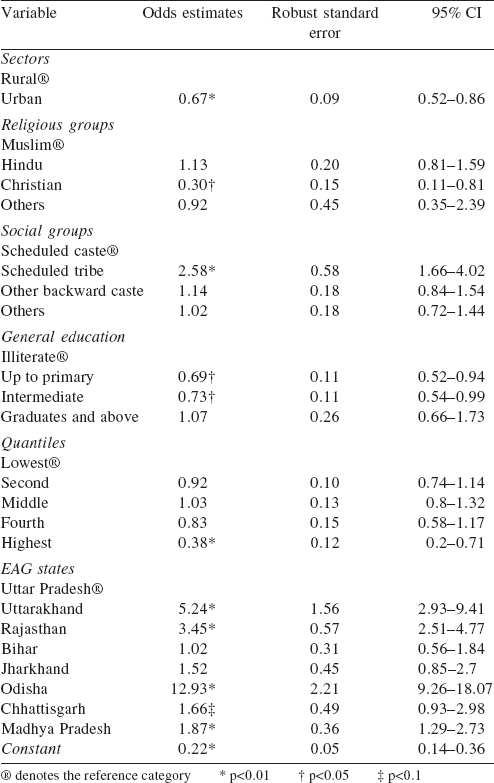
Factors influencing accessibility to healthcare
Accessibility to public and private sources of healthcare in both rural and urban areas of the EAG states primarily depends on the availability of health services ([Table - 4]). However, inpatients residing in urban areas (OR 0.67, p>0.01) have a lower preference for public health services in comparison to inpatients belonging to rural households. Ailing persons with primary (OR 0.69, p>0.05) and intermediate education (OR 0.73, p>0.05) were accessing public sources of healthcare less frequently compared to illiterate persons. Among the socioethnic groups, inpatients belonging to the scheduled tribes (OR 2.34, p<0.01) prefer public sources of healthcare in comparison to those belonging to the scheduled castes. However, there was no significant difference among the other backward castes (OBCs) and others. Ailing persons at the top of the wealth quantile (OR 0.38, p>0.01) had a lower preference for public healthcare in comparison to those in the lower wealth quantile. Among the EAG states, access to public sources of healthcare for persons residing in Odisha (OR 12.93, p<0.01) is 12 times higher, in Uttarakhand 5 times higher (OR 5.24, p<0.01), Rajasthan 3 times (OR 3.45, p<0.01) and Madhya Pradesh 2 times (OR 1.87, p<0.01); and this is statistically significant in comparison to persons residing in Uttar Pradesh.
Historically, after independence, Indian health policy saw the State as the main provider and financier of healthcare for all. [21] The National Rural Health Mission (NRHM) envisages providing high-quality health services especially to citizens of the EAG states at a reasonable cost. [22]
We sought to highlight the extent of access to public and private sources of healthcare, and also examine the factors that play a role in ailing persons in EAG states accessing private sector health facilities more often. The Report of the High Level Expert Group of the Planning Commission on Universal Health Coverage (UHC), [23] and the Steering Committee on Health and Steering Committee on Ayurveda, Yoga and Naturopathy, Unani, Siddha and Homoeopathy (AYUSH) for the 12th Plan have come only in the wake of civil society concerns with universal access to healthcare. [24],[25] However, our results reveal that access to public sources of healthcare is limited in the EAG states. An average 74% of the population of EAG states is currently relying on private sector health facilities.
The states in India selected for this study have been recognized as poor performing states since the 1980s, based on their low health indicators. [18],[26] EAG as the group of most backward and deprived states needs greater access to public sources of healthcare because the cost of treatment at a public health facility is much more affordable than at private health facilities. [6],[16],[18] Among the EAG states, Uttar Pradesh and Bihar have been found to be the worst performing states in terms of access to public sources of healthcare as around 83% of inpatients (in both rural and urban areas) of these states are dependent on private sources of healthcare. Though the situation is similar in Jharkhand, the inpatients of mainly rural areas of Odisha and Uttarakhand have better access to public sources of healthcare. The dependency on private sources of healthcare is also higher in Madhya Pradesh, Rajasthan and Chhattisgarh. [8],[16]
The failure of the public health system to expand commensurate with a growing population and its health requirements opens doors for several private practitioners to expand their so-called medical business in the EAG states. The range of private healthcare providers varies from solo practices and small nursing homes (private hospital) to large corporate hospitals. [16] Among these private practices, it is only private doctors on whom >60% of the overall inpatients of EAG states are dependent for medical advice while ailing. Surprisingly, inpatients of Bihar (68% rural and 69% urban), Uttar Pradesh (66% rural and 63% urban) and Jharkhand (63% rural and 62% urban) are predominantly dependent on solo doctors among the other private sources of healthcare. Similarly, more than half the inpatients of Madhya Pradesh (51% rural and 50% urban) show their reliance on solo doctors (private doctors) for their health needs. The dependency on the solo doctors in Chhattisgarh (40% rural and 48% urban) is similar in Madhya Pradesh. De Costa and Johannson have also suggested that the public sector health facilities are waning in Madhya Pradesh, and thus, people are moving towards the private sector. [8] Further, among the private sources, particularly private hospitals are seen as providing healthcare to a large proportion of inpatients in both rural and urban areas of Rajasthan (22% rural and 24% urban) and Uttarakhand (20% rural and 24% urban). Moreover, accessibility to public health services has improved in Bihar, but it has declined in the other EAG states if we compare results of the present study with those of the National Family Health Survey-3 (NFHS-3). [27]
As per the NFHS-3 (2005-06), at the time of the survey, 92.9% of inpatients of Bihar had reported their dependency on private sources of healthcare, though we found that it had reduced to 83% in 2015. Despite a greater emphasis given to improve accessibility to public sources of healthcare in previous years, the results show that the dependency of inpatients on private sources of healthcare has been enhanced in Chhattisgarh (if we compare the results with NFHS-3) from 63.1% to 66%, Jharkhand from 74.8% to 77.5%, Madhya Pradesh from 61.9% to 72% in the year 2015. The dependency for health needs on the private sector has almost doubled in Odisha (from 22.9% to 41%) and Rajasthan (from 29.6% to 58.5%) in the past decade. However, there has been almost no change in Uttarakhand (54.2% to 54%) and Uttar Pradesh (84.2% to 83.5%) in the past 10 years. Such an extreme dependency on private source of healthcare has been criticized by previous studies on grounds such as lack of political commitment in recognizing health as an essential component of human development reflected by consistently low investment, [9] badly formulated policies, and poor implementation of programmes, resulting in inadequate access to public sector healthcare. [7],[28],[29],[30] The lower accessibility to public health facilities forces a large number of people to go for high out-of-pocket spending in the private sector. [31]
The private health sector in India today is very diverse. World-class care is accessible to a very limited population who can afford to pay for it, while a larger unqualified sector provides services to poorer people in rural areas and urban slums. [32],[33] The existing healthcare system with a dominant private sector and its high out-of-pocket mechanism leads to a catastrophic level of spending for healthcare in several households which drags them further into poverty. [34],[35] However, private health facilities lead to a highly unequal access to healthcare, and thus unequal health outcomes among varied socioeconomic population groups. [7],[8] Baru has also explained that due to rising commercialization of health services, India has an unregulated private sector of healthcare which has made some unprecedented strides at the cost of the public sector. [30]
We also studied factors causing people to go for high out-of-pocket expenditure in the private sector, and why they do not access cheaper public healthcare services available in their area.
Concerns about the quality of healthcare have existed for almost as long as healthcare itself, but recently there has been a renewed vigour at making quality as the service provisioning principle. [36] As quality healthcare services are closely intertwined with health outcomes, [37] providing quality healthcare has become the leading healthcare agenda, both internationally and within India. To maintain the quality of healthcare services, there are a set of Indian Public Health Standards (IPHS) formed by the Ministry of Health and Family Welfare, with the aim to deliver high-quality health services in India. [38] Despite a greater emphasis on improving the quality of health services particularly in the EAG states under the NRHM, our study reveals that poor quality of healthcare remains the biggest drawback in public sector health facilities in the EAG states. Bihar, Madhya Pradesh and Odisha were found to deliver the worst quality of healthcare in the EAG states. [26] Uttarakhand, Chhattisgarh and Uttar Pradesh also deliver poor quality health services but comparatively better than the other EAG states. [26] Owing to poor quality of health services, users of public hospitals are less satisfied than those of private hospitals as the latter get quality treatment. [26] Hence, improvement in the quality of healthcare services is needed to increase the accessibility to public sources of healthcare.
Quality in healthcare is associated with the adequacy of features of health service provisioning as well as provision of preventive and promotive services. [37] Studies have shown that public health systems of the EAG states are marked by insufficient healthcare infrastructure (low doctor-population ratio, doctor-nurse ratio, population-bed ratio, population per health/subcentre ratio), undersupply of medicines, inadequate basic laboratory services, emergency services and improper referral services. [18],[26],[39] Muralidharan and Nandraj have pointed out that the reasons behind poor quality include lack of monitoring by statutory bodies, outdated and inadequate legislation and inability of the government to enforce the regulatory laws. [40] These factors are a major constraint in delivering quality healthcare services in the EAG states.
An average 13% of ailing persons of the EAG states reported that they did not have any choice in accessing healthcare because the services they needed were not available at public sources of healthcare in their area. Among the EAG states, the inpatients of Jharkhand (38% rural and 34% urban) were the biggest sufferers as the government failed to supply the required public healthcare services in their area. [41] Bihar is the worst in terms of quality of healthcare and long waiting time in public health services. Poor quality and long waiting time to access public sources of healthcare were a major drawback of the healthcare system of the EAG states. [11],[26],[42] However, non-availability of public health services was not noticed as a major problem in this state compared to the other EAG states. Similarly, the non-availability of health services was not a major barrier in Odisha. There is a vast difference in availability of health services between rural and urban areas of Uttarakhand and Chhattisgarh. Surprisingly, the non-availability of health services was reported around 7 times more in urban areas (26%) of Uttarakhand than its rural parts (4%). Also, it was around 6 times more in urban parts (16%) of Chhattisgarh than its rural areas (3%). Conversely, the non-availability of health services was reported only twice as often in rural areas (20%) of Uttar Pradesh than its urban parts (10%). In such a situation of non-availibility of public health services, people are left with no option other than availing private sources of healthcare for their health needs. Jacobs et al. [15] and Ramani and Mavalankar [43] have also pointed out that non-availability of public healthcare services remain an important public health challenge in India.
The role of geographical accessibility in the overall dynamics of healthcare access has been well articulated by researchers. [44],[45],[46] Our study reveals that a larger proportion of inpatients (15% rural and 10% urban) of the EAG states could not access public health services because of the remote location of services in their area. Due to the odd location of health services, there is a significant difference in access to healthcare between rural and urban areas. [46] Among the EAG states, the inpatients of Chhattisgarh, Bihar and Madhya Pradesh suffer more as public sources of healthcare are out of their reach. Studies have also shown that remote and adverse topography of health services constrain access to healthcare and result in poor health outcomes. [46],[47],[48] Also, access to remotely located health services depends on the available means of transportation and increases the indirect cost to inpatients. [15] Similarly, geographical accessibility also emerged as one of the barriers in access to public sources of healthcare in the EAG states.
The Ministry of Health and Family Welfare has acknowledged that a bureaucratic and overburdened public health sector was increasingly unable to care for a steadily growing population. [49] A study by Kumar and Mishra revealed that there is an enormous shortfall in health infrastructure in the EAG states, [26] and thus health centres have to cover a vast additional population. Due to imbalances in the provider-population ratio, inpatients (14% rural and 24% urban) reported that they have to wait for a long time to seek healthcare from public sector health facilities. The fear of standing for a long time in a queue makes patients less interested in public sources of healthcare. [11],[15],[39] It has previously been shown that as the level of education increases, the utilization of government health services decreases. [50] This study also shows that inpatients belonging to the lowest wealth quantile are more dependent on public sources of healthcare. Most of the patients of the lowest wealth quantile are daily labourers, and thus may lose their day wage. So, they bypass the public sources of healthcare at the time of health needs.
Conclusion
The meagre accessibility to public sources of healthcare in the EAG states shows that the government′s initiatives to enhance accessibility to health services have not yielded the desired results; hence, this should be a matter of concern for policy-makers. The government needs to take necessary steps to make the public sector more accessible than the private sector if we are to achieve universal access to healthcare. There is a need to improve the quality of public sector health services and also strengthen infrastructure to reduce waiting time and enhance the physical reach of inpatients when they are in need. The state needs to take an initiative with good governance and forge feasible partnership with the dominant private sector to ensure equitable access to healthcare for all.
| 1. | WHO. Report on the International Conference on Primary Health Care, Alma-Ata, USSR, 6-12 September 1978. Geneva:WHO; 1978. [Google Scholar] |
| 2. | Gulliford M, Figueroa-Munoz J, Morgan M, Hughes D, Gibson B, Beech R, et al. What 'does access to health care' mean? J Health Serv Res Policy 2002; 7: 186-8. J Health Serv Res Policy 2002; 7: 186-8.'>[Google Scholar] |
| 3. | Kanuganti S, Sarkar AK, Singh AP, Arkatkar SS. Quantification of accessibility to health facilities in rural areas. Case Stud Transp Policy 2015; 3: 311-20. [Google Scholar] |
| 4. | Acharya SS. Universal health care: Pathways from access to utilization among vulnerable populations. Indian J Public Health 2013; 57: 242. [Google Scholar] |
| 5. | Park JE. Textbook of preventive and social medicine (A treatise on community health). 21st ed. Jabalpur:Banarsidas Bhanot; 2011. [Google Scholar] |
| 6. | Planning Commission. Twelfth five-year plan (2012-17): Social Sectors, Vol. III, Planning Commission, Government of India (1-46). New Delhi:Sage Publications; 2013. [Google Scholar] |
| 7. | Baru R, Acharya A, Acharya S, Kumar AS, Nagaraj K. Inequities in access to health services in India: Caste, class and region. Econ Polit Wkly 2010; 45: 49-58. [Google Scholar] |
| 8. | De Costa A, Johannson E. By 'default or design'? The expansion of the private health care sector in Madhya Pradesh, India. Health Policy 2011; 103: 283-9. Health Policy 2011; 103: 283-9.'>[Google Scholar] |
| 9. | WHO. National Health Accounts, Country Information. Available at www.who.int/nha/country/ind/en/ (accessed on 24 Feb 2016). [Google Scholar] |
| 10. | Balarajan Y, Selvaraj S, Subramanian SV. Healthcare and equity in India. Lancet 2011; 377: 505-15. [Google Scholar] |
| 11. | Powell-Jackson T, Acharya A, Mills A. An assessment of the quality of primary healthcare in India. Econ Polit Wkly 2013; 48: 53-61. [Google Scholar] |
| 12. | Parker EB, Campbell JL. Measuring access to primary medical care: Some examples of the use of geographical information systems. Health Place 1998; 4: 183-93. [Google Scholar] |
| 13. | Noor AM, Gikandi PW, Hay SI, Muga RO, Snow RW. Creating spatially defined databases for equitable health service planning in low-income countries: The example of Kenya. Acta Tropica 2004; 91: 239-51. [Google Scholar] |
| 14. | Sarkar AK, Ghosh D. Integrated Rural Accessibility Planning (IRAP), an application in three panchayats in Rajasthan, India. Prog Develop Stud 2008; 8: 241-59. [Google Scholar] |
| 15. | Jacobs B, Ir P, Bigdeli M, Annear PL, Van Damme W. Addressing access barriers to health services: An analytical framework for selecting appropriate interventions in low-income Asian countries. Health Policy Plan 2012; 27: 288-300. [Google Scholar] |
| 16. | Kumar A, Furtado KM, Jain N, Nandraj S. NSSO 71st Round: Same data, multiple interpretations. Eco Polit Wkly 2015; 50: 46-7. Available at www.epw.in/journal/2015/46-47/discussion/nsso-71st-round.html (accessed on 24 Feb 2016). [Google Scholar] |
| 17. | Census of India 2011. Office of the Registrar General Census Commissioner, Indian Census Bureau. Ministry of Home Affairs, Government of India. [Google Scholar] |
| 18. | Ministry of Health and Family Welfare. Family welfare statistics in India 2011. Statistics Division. New Delhi:MoHFW, Government of India: 2011. Available at http://mohfw.nic.in/WriteReadData/l892s/3503492088FW%20Statistics%202011%20Revised%2031%2010%2011.pdf (accessed on 24 Feb 2016). [Google Scholar] |
| 19. | Oaxaca R. Male-female wage differentials in urban labor markets. Int Eco Rev 1973; 14: 693-709. [Google Scholar] |
| 20. | O'Donnell O, Doorslaer E van, Wagstaff A, Lidelow M. Analyzing health equity using household survey data. A guide to techniques and their implementation. Washington, DC:The World Bank; 2008. Analyzing health equity using household survey data. A guide to techniques and their implementation. Washington, DC:The World Bank; 2008.'>[Google Scholar] |
| 21. | Bhore J, Amesur R, Banerjee A. Report of the health survey and development committee. New Delhi:Government of India; 1946. [Google Scholar] |
| 22. | National Rural Health Mission. Mission document 2005-2012. Ministry of Health and Family Welfare, Government of India. Available at http://upnrhm.gov.in/site-files/Mission-Document.pdf (accessed on 20 Jul 2015). [Google Scholar] |
| 23. | Government of India. High level expert group report on universal health coverage for India. New Delhi:Planning Commission; 2011. Available at http://planningcommission.nic.in/reports/genrep/rep_uhc0812.pdf (accessed on 22 Feb 2016). [Google Scholar] |
| 24. | Government of India. Report of the Steering Committee on Health for the 12th Five-Year Plan: Incorporating Report of the Working Groups and deliberations in Steering Committee Meetings. Health Division, Planning Commission, 2012. Available at http://planningcommission.nic.in/aboutus/committee/strgrp12/str_health0203.pdf (accessed on 20 Feb 2016). [Google Scholar] |
| 25. | Government of India. Report of the Steering Committee on AYUSH for the 12th Five Year Plan (2012-17). Planning Commission, 2012. Available at http://planningcommission.nic.in/aboutus/committee/wrkgrp12/health/WG_7_ayush.pdf (accessed on 23 Feb 2016). [Google Scholar] |
| 26. | Kumar V, Mishra AJ. Quality of health care in primary health care system: A reflection from Indian state. Int J Health Syst Disaster Manage 2015; 3: 136-40. [Google Scholar] |
| 27. | International Institute for Population Sciences (IIPS) and ORC Macro. National Family Health Survey (NFHS-3), India, 2005-06. India. Mumbai:IIPS; 2007. [Google Scholar] |
| 28. | Reddy KS, Patel V, Jha P, Paul VK, Kumar AK, Dandona L; Lancet India Group for Universal Healthcare towards achievement of universal health care in India by 2020: A call to action. Lancet 2011; 377: 760-8. [Google Scholar] |
| 29. | Berman PA. Rethinking health care systems: Private health care provision in India. World Dev 1998; 26: 1463-79. [Google Scholar] |
| 30. | Baru RV. Public sector doctors in the era of commercialisation. In: Sheikh K, George A (eds). Health providers in India: On the frontiers of change. Vol. 1. New Delhi:Routledge; 2010:81-96. [Google Scholar] |
| 31. | Ladusingh L, Pandey A. Health expenditure and impoverishment in India. J Health Manage 2013; 15: 57-74. [Google Scholar] |
| 32. | De Costa A, Diwan V. 'Where is the public health sector?': Public and private sector healthcare provision in Madhya Pradesh, India. Health Policy 2007; 84: 269-76. Health Policy 2007; 84: 269-76. '>[Google Scholar] |
| 33. | De Costa A, Al-Muniri A, Diwan VK, Eriksson B. Where are healthcare providers? Exploring relationships between context and human resources for health Madhya Pradesh province, India. Health Policy 2009; 93: 41-7. [Google Scholar] |
| 34. | Bonu S, Bhushan I, Rani M, Anderson I. Incidence and correlates of 'catastrophic' maternal health care expenditure in India. Health Policy Plan 2009; 24: 445-56. Health Policy Plan 2009; 24: 445-56. '>[Google Scholar] |
| 35. | Mohanty SK, Srivastava A. Out-of-pocket expenditure on institutional delivery in India. Health Policy Plan 2012; 28: 247-62. [Google Scholar] |
| 36. | Lee H, Vlaev I, King D, Mayer E, Darzi A, Dolan P. Subjective well-being and the measurement of quality in healthcare. Soc Sci Med 2013; 99: 27-34. [Google Scholar] |
| 37. | Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Quart 2005; 83: 457-502. [Google Scholar] |
| 38. | Satpathy SK. Indian Public Health Standards (IPHS) for Community Health Centers. Indian J Public Health 2005; 49: 123-6. Available at http://nrhm.gov.in/nhm/nrhm/guidelines/indian-public-health-standards.html (accessed on 24 Feb 2016). [Google Scholar] |
| 39. | Bajpai V. The challenges confronting public hospitals in India, their origins, and possible solutions. Adv Pub Health 2014; 2014: 1-27. [Google Scholar] |
| 40. | Muralidharan VR, Nandraj S. Private health care in India. In: Yazbeck AS, Peters DH (ed). Health policy research in South Asia: Building capacity for reform. Health, nutrition, and population series. Washington, DC:World Bank; 2003:241-2. [Google Scholar] |
| 41. | Ministry of Health and Family Welfare. Rural Health Statistics 2014-15: Statistics Division. New Delhi:MoHFW, Government of India; 2015. [Google Scholar] |
| 42. | Narang R. Determining quality of public healthcare services in rural India. Clin Gov Int J 2011; 16: 35-49. [Google Scholar] |
| 43. | Ramani KV, Mavalankar D. Health system in India: Opportunities and challenges for improvements. J Health Organ Manag 2006; 20: 560-72. [Google Scholar] |
| 44. | Jordan H, Roderick P, Martin D, Barnett S. Distance, rurality and the need for care: Access to health services in South West England. Int J Health Geogr 2004; 3: 21. [Google Scholar] |
| 45. | Cromley RG, Cromley EK. Chloropleth map legend design for visulizing community health disparities. Int J Health Geogr 2009; 8: 52. [Google Scholar] |
| 46. | Peters DH, Garg A, Bloom G, Walker DG, Brieger WR, Rahman MH. Poverty and access to health care in developing countries. Ann N Y Acad Sci 2008; 1136: 161-71. [Google Scholar] |
| 47. | Perry B, Gesler W. Physical access to primary heath in Andean Bolivia. Soc Sci Med 2000; 50: 1177-188. [Google Scholar] |
| 48. | Rahman SU, Smith DK. Use of location-allocation models in health service development planning in developing nations. Eur J Oper Res 2000; 123: 437-52. [Google Scholar] |
| 49. | Ministry of Health and Family Welfare. Report of the National Commission on Macroeconomics and Health. New Delhi:MoHFW, Government of India; 2005. Available at www.who.int/macrohealth/action/Report%20of%20the%20National%20Commission.pdf (accessed on 24 Feb 2016). [Google Scholar] |
| 50. | Chaudhuri A. Socio-economic inequity in healthcare utilization and expenditures in richer states in India. Indian J Med Res 2012; 136: 368-9. [Google Scholar] |
Fulltext Views
8,995
PDF downloads
4,120




