Translate this page into:
Arrhythmia occurring as the sole presenting feature in Covid-19
Correspondence to ANUPAM BHAMBHANI; anupam.bhambhani@yahoo.in
[To cite: Bhambhani A, Pasam P. Arrhythmia occurring as sole presenting feature in Covid-19. Natl Med J India 2022;35:236–8.]
Abstract
Severe acute respiratory syndrome coronavirus 2 (SARSCoV-2) infection is observed to be associated with several cardiac complications. Cardiac arrhythmias are frequently observed in critically ill patients and are usually associated with myocarditis. We report two patients with Covid-19, in whom serious arrhythmias were the sole presenting feature, in the absence of any of the known manifestations of the disease. Further research is required into this yet unknown mechanism of the effect of Covid-19 on the conduction system. Thus, managing patients with acute-onset arrhythmias of unexplained aetiology, even when they present without known clinical features of Covid-19, should be done with care.
INTRODUCTION
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection is observed to be associated with several clinically manifest cardiac complications that are frequently responsible for increased morbidity and mortality in the affected patients.1 These complications are particularly seen in critically ill patients and include myocarditis with or without heart failure, acute coronary syndrome, arrhythmias, cardiogenic shock and systemic as well as venous thromboembolisms. Cardiac rhythm disorders are reported frequently in these patients and include non-specific palpitations,2 life-threatening ventricular arrhythmias,3 atrial fibrillation (AF),4,5 and, although rarely, bradyarrhythmias such as transient complete heart block6 and sinus node dysfunction.7,8 We report two patients with Covid-19, where serious arrhythmias were the sole presenting feature. This report calls for further research into yet unknown mechanisms of cardiac involvement of Covid-19, especially the effects on the conduction system; and alerts the medical fraternity to take precautions towards personal protection while managing patients with acute-onset arrhythmias of unexplained aetiology, even when they present without known clinical features of SARS-CoV-2 infection.
THE CASES
Case 1
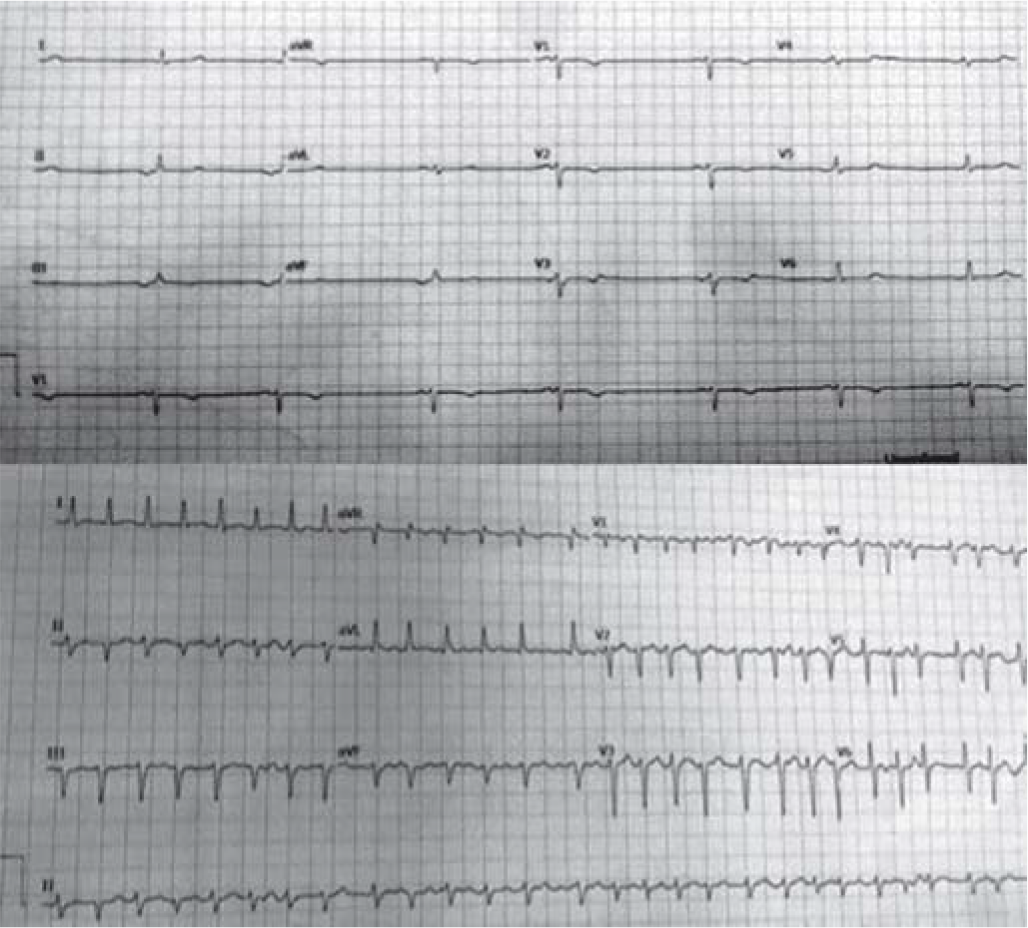
A 36-year-old asymptomatic woman, with no history of any chronic illness or of any addiction, voluntarily got her reverse transcription-polymerase chain reaction (RT-PCR) for SARSCoV-2 done, as her husband was diagnosed with Covid-19 a day before. Her test was found positive for infection, and as per national guidelines prevalent at that time, she was admitted to the hospital. At the time of admission, her heart rate (HR) was 49 per minute, blood pressure (BP) was 110/70 mmHg; the respiratory rate and pulse oximetry saturation at room air were 20 per minute and 99%, respectively; she was afebrile with a temperature of 35.7 °C. In view of bradycardia, electrocardiogram (ECG) was advised, which revealed complete sinus pause (sinus node arrest), with low atrial escape rhythm (Fig. 1, upper panel). The chest X-ray was normal. Other investigations were as mentioned in Table I. After a few hours, the HR further dropped to 42 per minute associated with a drop in systolic BP to 90–95 mmHg and an appearance of mild uneasiness. Injection atropine 1.2 mg intravenous was administered, following which the hypotension and her symptoms disappeared and the HR improved to 60 per minute. She was started on theophylline tablets, in addition to the treatment advised by the infectious disease team. Her remaining hospital stay was uneventful, and she was discharged after cure from Covid-19.
-
Upper panel: Electrocardiogram showing sinus arrest with low atrial escape rhythm in case 1; lower panel: Electrocardiogram showing atrial fibrillation with fast ventricular response in case 2
| Investigation | Case 1 | Case 2 | Reference range |
|---|---|---|---|
| White blood cell count (k/μl) | 3.8 | 9.9 | 4.0–11.0 |
| Red blood cell count (k/μl) | 4.58 | 5.6 | 4.5–5.5 |
| Haemoglobin (g/dl) | 13.1 | 15.5 | 13–17 |
| Haematocrit (%) | 39.9 | 47.7 | 40–50 |
| Platelet count (k/μl) | 227 | 285 | 150–410 |
| Neutrophil (%) | 44.8 | 79.6 | 40–80 |
| Lymphocyte (%) | 43.7 | 12.1 | 20–40 |
| Monocytes (%) | 9.7 | 7.7 | 2–10 |
| Eosinophils (%) | 1.5 | 0.1 | 1–6 |
| Basophils (%) | 0.3 | 0.6 | 0–2 |
| Blood urea (mg/dl) | 14.98 | 59.9 | 16–40 |
| Serum creatinine (mg/dl) | 0.70 | 1.27 | 0.9–1.3 |
| Sodium (mmol/L) | 140 | 127 | 136–145 |
| Potassium (mmol/L) | 3.73 | 3.83 | 3.5–5.1 |
| Creatine phosphokinase MB | – | 3.2 | 0.6–6.3 |
| (ng/ml) | |||
| Troponin I (ng/ml) | – | 0.006 | 0.02–0.04 |
| D-dimer (μg/ml) | 0.2 | 7.9 | 0–0.5 |
| Aspartate transaminase (U/L) | 1 8 | 2 3 | 15–40 |
| Alanine transaminase (U/L) | 1 5 | 2 4 | 10–40 |
| Amylase (U/L) | – | 252 | 24–125 |
| Serum ferritin (ng/ml) | 18.5 | 375.7 | 20–250 |
| Thyroid stimulating hormone | 3.68 | – | 0.35–5.5 |
| (μIU/ml) |
We attributed the sinus arrest in this case to Covid-19 because of many circumstantial evidences which included: (i) its onset and offset correlated with the SARS-CoV-2 infection; (ii) other causes of bradyarrhythmia, namely hypothyroidism, drugs, ischaemia were excluded; (iii) it was unlikely to be an incidental finding related to congenital sinus node disease because it was causing symptomatic hypotension, which the patient would have experienced if the arrhythmia had been there earlier; (iv) since it persisted for hours, it cannot be attributed to the transient increase in vagal tone; and (v) bradyarrhythmias have also been observed in association with Covid-19 in other parts of the world.6–9
Case 2
A 60-year-old man presented to the emergency room with a day’s history of acute-onset palpitation with fast HR, and moderate epigastric pain associated with vomiting. He had never felt similar palpitations in the past. He denied a history of any cardiac ailment and alleged that a routine health check-up done a month before had not revealed any cardiac abnormality. There was no history of recent fever, cough, dyspnoea, loss of smell or taste or of contact with any individual suffering from Covid-19.
The initial examination revealed AF with HR and BP of about 180 per minute and 140/78 mmHg, respectively. He was afebrile and had no tachypnoea. His initial blood parameters are given in Table I. His ECG confirmed AF with fast HR (Fig. 1, lower panel) and the echocardiogram and chest X-ray were normal. Since the history was short and there was no atrial enlargement on echocardiography, the AF was considered paroxysmal with recent-onset and treatment was started with amiodarone and low molecular weight heparin. In view of abdominal pain, opinion from the gastroenterology team was sought; they diagnosed intestinal ischaemia. A contrast-enhanced tomography scan confirmed intestinal gangrene with superior mesenteric artery embolism, for which surgery was advised. As per hospital policy, RT-PCR for SARS-CoV-2 was done before shifting him to the operation room; it was positive. In the meantime, verapamil was added, as his ventricular rate was persistently 160–180 per minute despite the ongoing amiodarone infusion, but the HR continued to be in the same range. His further hospital course was fulminant with the rapid development of acute renal failure and death.
The aetiology of AF, in this case, was likely to be Covid-19 because of multiple reasons including: (i) the history was short, suggesting acute-onset and temporally correlated with the positive RT-PCR; (ii) AF can occur in the presence of cytokine storm seen with Covid-19 and this patient had a fulminant course suggesting the presence of high inflammatory milieu; (iii) the patient’s cardiac assessment was normal a month ago; (iv) echocardiography was normal and did not reveal atrial enlargement, commonly seen with AF of other aetiologies; (v) the AF and the high ventricular rate, in this case, caused symptoms that were severe enough to make him seek emergency help and he would have noticed symptoms earlier also if this arrhythmia had been there before.
DISCUSSION
Although high prevalence of electrophysiological issues has been reported in severely affected patients of Covid-19,1 arrhythmias are less commonly observed in milder form of the disease. The absence of correlation between the severity of pulmonary involvement and occurrence of arrhythmias in SARSCoV-2 infection has been observed earlier,9 but important arrhythmias in complete absence of other known systemic or pulmonary manifestations were not reported in this disease until recently, when another group of authors8 reporting Covid-19-related bradyarrhythmias observed that 4 of their 7 patients did not have common symptoms of SARS-CoV-2 infection, namely cough, fever or dyspnoea. Although 2 of those 4 patients were found to have infiltrative shadows on chest Xray, the other 2, similar to our observations, did not have any of the usual described manifestations of the disease.
The occurrence of arrhythmias in Covid-19 is chiefly attributed to myocarditis; however, in our patients, we did not find any clinical, echocardiographic or biochemical evidence of myocarditis. Another group of researchers, who conducted autopsy studies on cardiac specimens obtained after confirmed Covid-19 deaths, also observed that the pathological findings did not corroborate with the observations expected in typical myocarditis.10,11
Other potential mechanisms suggested in the pathogenesis of arrhythmias in SARS-CoV-2, or in any severe pulmonary infection, include hypoxaemia, acidosis or electrolyte abnormalities, but all of these were absent in our patients. There are some anecdotal reports of bradyarrhythmias related to Covid-19,6–9 in which the investigators have explained the mechanism through severe hypoxia with consequent conduction defects, potentially mediated by endogenous adenosine;9 but neither of the patients described by us had evidence of moderate or severe hypoxia. Although, the possibility of cytokine storm as well as catecholamine release in response to organ stress caused by viral load can be the likely factors in the pathogenesis of AF in the second patient, but not in the one who had isolated sinus node dysfunction. However, if the mechanism(s) involved in sinus node dysfunction are understood, the occurrence of AF can also be explained since the latter can be a consequence of the former.
Our report highlights the need for further investigating the effect of SARS-CoV-2 infection on the conduction system, probably at the molecular level. This is necessary, not only to define the involved mechanisms and to guide preventive and therapeutic strategies but also to decipher the decisions on monitoring of arrhythmia in these patients.
Conflicts of interest
None declared
References
- Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061-9.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J (Engl). 2020;133:1025-31.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2352-71.
- [CrossRef] [PubMed] [Google Scholar]
- Coronavirus disease and new-onset atrial fibrillation: Two cases. Cureus. 2020;12:e8066.
- [CrossRef] [PubMed] [Google Scholar]
- Disrupting the electrical circuit: New onset atrial fibrillation in a patient with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Cureus. 2020;12:e9082.
- [CrossRef] [Google Scholar]
- Transient complete heart block in a patient with critical COVID-19. Eur Heart J. 2020;41:2131.
- [CrossRef] [PubMed] [Google Scholar]
- Sinus node dysfunction in a young patient with COVID-19. JACC Case Rep. 2020;2:1240-4.
- [CrossRef] [PubMed] [Google Scholar]
- Bradyarrhythmias in patients with COVID-19: A case series. Indian Pacing Electrophysiol J. 2020;20:211-12.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiac arrhythmias in COVID-19 infection. Circ Arrhythm Electrophysiol. 2020;13:e008719.
- [CrossRef] [PubMed] [Google Scholar]
- Pulmonary and cardiac pathology in African American patients with COVID-19: An autopsy series from New Orleans. Lancet Respir Med. 2020;8:681-6.
- [CrossRef] [PubMed] [Google Scholar]
- Unexpected features of cardiac pathology in COVID-19 infection. Circulation. 2020;142:1123-5.
- [CrossRef] [PubMed] [Google Scholar]




