Translate this page into:
Bilateral retrograde pyelography leading to anuria
Corresponding Author:
V S Karthikeyan
Department of Urology, Institute of Nephro Urology, Victoria Hospital Campus, Bengaluru 560002, Karnataka
India
sengkarthik@yahoo.co.in
| How to cite this article: Mallya A, Karthikeyan V S, Manohar C, Keshavamurthy R. Bilateral retrograde pyelography leading to anuria. Natl Med J India 2019;32:20-21 |
Abstract
Retrograde pyelography (RGP) is done to evaluate the collecting system when intravenous contrast studies are contraindicated due to renal insufficiency or prior adverse reactions. We report a patient who developed acute renal shutdown following bilateral RGP in the same sitting done for evaluation of positive malignant cytology of urine. A 65-year-old man on treatment for left stroke and hypertension, with a baseline serum creatinine of 1.9 mg/dl presented with painless haematuria for 2 months. Plain computed tomogram revealed a small papillary growth on the posterior wall of the urinary bladder. Transurethral resection revealed inflammatory atypia. As the patient continued to have haematuria, he was taken up for bilateral ureteric washings for cytology and bilateral RGP. A 5-Fr universal ureteral catheter was used to cannulate the ureters, urine was aspirated for cytology and 6 ml of 76% meglumine diatrizoate (1:2) was injected, and sufficient opacification with no abnormality or pyelosinus/venous or lymphatic reflux was noted. In the immediate postoperative period, he developed anuria and the serum creatinine rose to 3.6 mg/dl on postoperative day 1 and to 7.5 mg/dl on day 5. He needed three sessions of haemodialysis. Ultrasonography showed no hydroureteronephrosis. Urine output improved and his serum creatinine stabilized at the preoperative level of 1.8 mg/dl. The patient is doing well with stable renal function at 12 months. Although RGP is useful, it needs to be done with caution if a bilateral procedure is contemplated. This entity is seldom reported, and routine double-J stenting following unilateral/bilateral RGP also needs evaluation.
Introduction
Retrograde pyelography (RGP) is used as a diagnostic procedure in ureteric obstruction due to suspected upper urinary tract malignancies and in persistent haematuria with normal lower urinary tracts. It is generally a safe procedure to evaluate the collecting system, especially when contrast studies (intravenous urogram or contrast-enhanced computed tomogram [CT]) are contraindicated due to renal insufficiency, prior contrast reaction or if these yield inadequate information. Bilateral RGP is usually indicated for evaluation ofthe upper urinary tracts for malignancies. Anuria and renal failure following bilateral RGP are rare.
The Case
A 65-y ear-old man, with hypertension and a prior cerebrovascular accident, on regular treatment presented with gross haematuria for 6 months. He was a smoker since the age of 35 years. His urine output was 1200 ml/day, urine culture was sterile, serum creatinine was 1.9 mg/dl and urine cytology showed malignant cells. Plain CT of the kidneys and bladder showed a 1.5 cm×1 cm papillary growth in the left lateral wall with normal upper tracts [Figure - 1]. Transurethral resection of the bladder tumour (TURBT) showed inflammatory atypia on histopathology. As he continued to have haematuria, he was taken up for cystoscopy, bilateral ureteric washings for cytology and RGP. A ureteroscopic evaluation was planned in case of any abnormality on RGP. The procedure was done under spinal anaesthesia. At cystoscopy, the TURBT site showed inflamed mucosa, normal ureteric orifices and no bloodstained efflux. A 5-French ureteral catheter was inserted, urine was aspirated from the ureter for cytology and 6 ml of 76% meglumine diatrizoate (1:2 dilution) injected bilaterally. On both sides, sufficient opacification was seen, with no abnormality or pyelosinus/venous or lymphatic backflow [Figure - 2]. The ureters were not stented. A 14-French Foley per urethral catheter was placed at the end of surgery. The patient had an uneventful intraoperative course and was haemodynamically stable throughout the procedure. In the immediate postoperative period, he developed anuria with worsening renal parameters. Despite intravenous fluid boluses of 200 ml of 0.9% normal saline over 1 hour at a gap of 4 hours in addition to intravenous fluids at 50 ml/hour, his urine output did not improve. He had anuria but did not develop fluid overload, and his blood urea was 90 mg/dl and serum creatinine 7.5 mg/dl by postoperative day 5. He required three sessions of haemodialysis and his urine output started improving. His total leucocyte count (8500/cmm) and serum procalcitonin (0.12 ng/ ml) were normal. He was not on any nephrotoxic medications. There was no hydroureteronephrosis on ultrasound [Figure - 3]. The renal parameters improved and reached baseline (serum creatinine 2 mg/dl) and the urine output was around 1200 ml/day by postoperative day 12. His serum creatinine is stable at 1.8 mg/dl at 12 months post procedure.
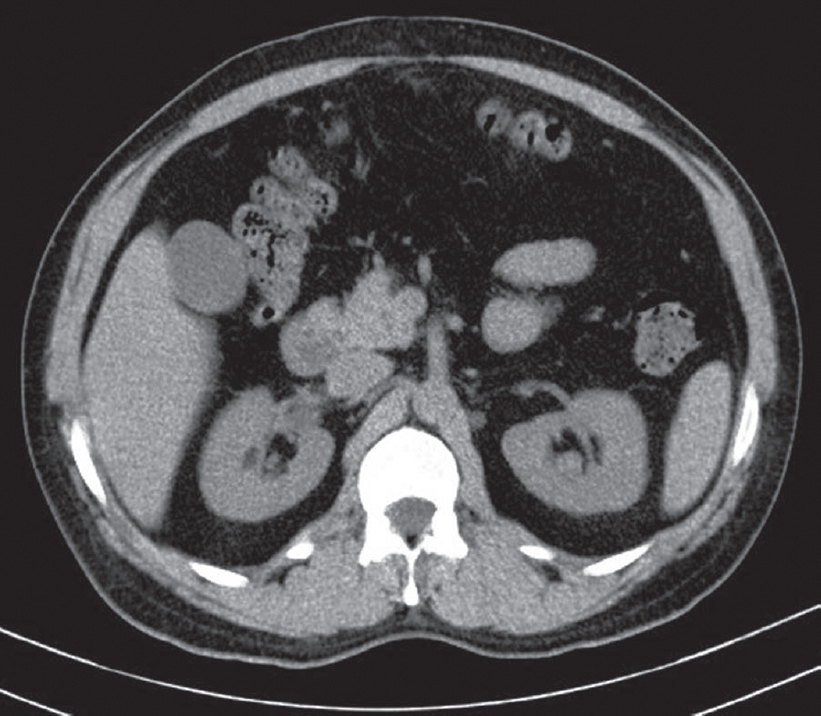 |
| Figure 1: Plain computed tomogram of the kidneys showing no hydronephrosis |
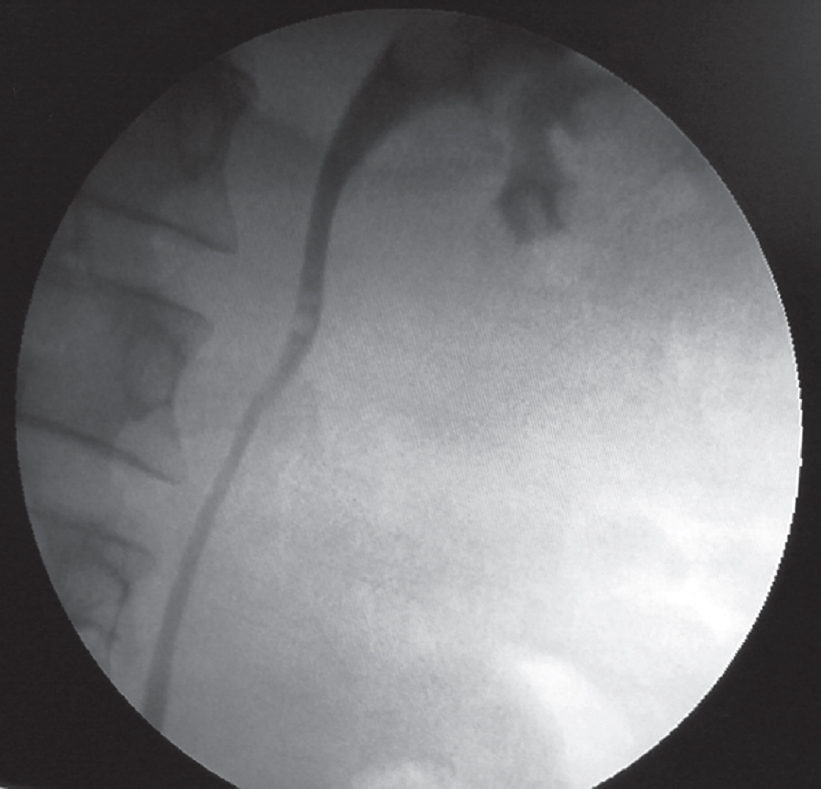 |
| Figure 2: Intraoperative image of left retrograde pyelogram showing non-dilated renal pelvis, calyces and ureter with no pyelovenous/pyelosinus/pyelolymphatic reflux |
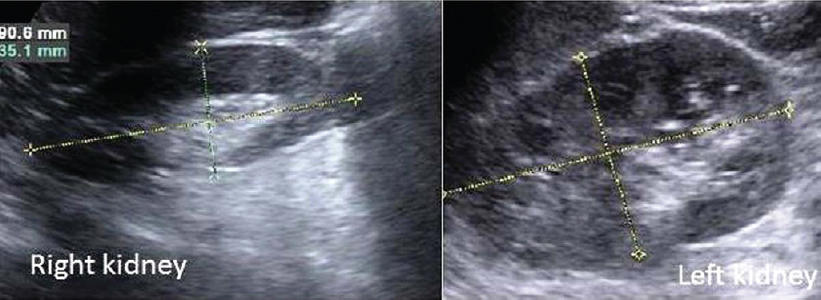 |
| Figure 3: Postoperative ultrasound scan showing bilateral kidneys with no hydroureteronephrosis |
Discussion
RGP is a diagnostic procedure done for patients with ureteric obstruction and is usually followed by stenting and, if not possible, diversion in the form of percutaneous nephrostomy. However, anuria after diagnostic RGP for upper tract evaluation in malignancy is rarely reported, and the role of elective stenting in such cases is not clear from the literature. Chiu et al. and Hurley reported similar occurrences following RGP.[1]·[2] Bilateral RGP on the same day has been debated, but no consensus has emerged.[1],[2] The cause of renal failure in our patient was not clear.
RGP is preferred in renal failure as it does not induce contrast- induced nephropathy in patients predisposed to or already in renal failure. Most instances in previous reports have been due to some form of backflow due to high intrapelvic pressure, obstructed systems or septicaemia. Our patient had no pyelosinus/venous or lymphatic backflow. His workup for infection was negative as well. Hsu et al. reported a patient in whom mucosal oedema due to contrast and trauma caused obstructive uropathy.[3] However, even 5 days after the procedure, our patient did not have hydroureteronephrosis. Although there is a possibility of sclerosis of ureters, his serum creatinine stabilized after the initial three sessions of haemodialysis and he is producing around 1.2 litres of urine every day.
The possibility of sepsis-induced acute kidney injury is less likely in our patient because he did not have tachycardia, hypotension, fever or tachypnoea. His postoperative serum procalcitonin and total leucocyte counts were also normal. We are thus not able to hypothesize why he developed anuria after bilateral RGP and whether bilateral double-J stenting would have prevented this complication. Anuria could have been due to oedema of the upper urinary tracts due to radiographic contrast administration which settles after 5 days, leading to improvement in renal function. Whether stenting is mandatory in patients with borderline renal function, pre-existing comorbid conditions and when bilateral procedures are contemplated is not clear.
Conflicts of interest. None declared
| 1. | Chiu YS, Chiang HW, Huang CY, Tsai TJ. ARF after retrograde pyelography: A case report and literature review. Am J Kidney Dis 2003;42:E13-E16. [Google Scholar] |
| 2. | Hurley RM. Acute renal failure secondary to bilateral retrograde pyelography. Clin Pediatr (Phila) 1979;18:754-6. [Google Scholar] |
| 3. | Hsu C, Tseng H, Chen C. Acute renal failure after bilateral retrograde pyelography— Case of early diversion. Acta Nephrologica 2012;26:97-9. [Google Scholar] |
Fulltext Views
2,581
PDF downloads
2,469




