Translate this page into:
Caregiver perceptions on intensive care: A qualitative study from southern India
2 Clinical Epidemiology Unit, Christian Medical College, Vellore, Tamil Nadu, India
3 Medical Intensive Care Unit, Christian Medical College, Vellore, Tamil Nadu, India
4 Department of Medicine, Pondicherry Institute of Medical Sciences, Puducherry, India
5 Department of Medicine, Christian Medical College, Vellore, Tamil Nadu, India
Corresponding Author:
Shuba Kumar
Samarth, No. 100 Warren Road, Mylapore, Chennai 600004, Tamil Nadu
India
shuba58@gmail.com
| How to cite this article: Kumar S, Christina J, Jagadish AR, Peter JV, Thomas K, Sudarsanam TD. Caregiver perceptions on intensive care: A qualitative study from southern India. Natl Med J India 2017;30:131-135 |
Abstract
Background. Admission of a patient to an intensive care unit (ICU) can result in tremendous stress to family caregivers not only because of the need to provide physical and emotional support to the sick relative, but also due to the burden of decision-making on behalf of the critically ill person. We enquired about family caregivers' perspectives on intensive care, the challenges they faced with decision-making and their perceptions on the nature of their interactions with healthcare providers.Methods. We used maximum variation sampling and enrolled 20 consenting caregivers for semi-structured interviews. Each interview, based on an interview guide, took 30–40 minutes and was conducted in a private place within the hospital premises. All interviews were recorded, transcribed verbatim and entered into a qualitative software (NVivo) for analysis.
Results. The three emergent themes of analysis were (i) understanding about ICU, (ii) decision-making concerning ongoing treatment; and (iii) relationship with healthcare-providers. Some respondents saw the intensive care as an expensive facility for seriously ill patients while others were not so clear. The family's relationship with the patient and their financial status were seen as important deciding factors in continuing treatment. Decision-making was a complex and emotional issue and doctors were held in awe and seen as the main deciding authority. The importance of doctors being compassionate and communicative was stressed.
Conclusion. Our study highlights the problems faced by family caregivers and of the need to improve their satisfaction through clear and simple communication strategies.
Introduction
All over the world, family caregivers play a major role in supporting family members who are ill.[1],[2] Such support may extend to activities of daily living. When acute illness leads to admission to an intensive care unit (ICU), the patient's dependence for assistance increases several-fold and much of this burden falls on the family caregiver. In addition to having to deal with the healthcare system, communicate with healthcare providers and manage their own personal distress, family caregivers are also called upon to make decisions on behalf of the patient. Such decision-making can be extremely challenging for family caregivers and could seriously impair their own sense of well-being.[3],[4]
Studies from developed countries have documented caregiver experience and challenges associated with caring for a relative admitted in an ICU. A study from the USA[5] described how family caregivers of patients admitted to an ICU tended to be less mindful of their own health, which in turn impacted on their ability to adequately care for the patient. Another study from France[6] underscored the critical need for both physicians and ICU staff to be supportive and to provide caregivers with all the necessary information to understand the patient's condition so that they are better equipped to participate in decision-making. Other quantitative and qualitative studies have reported reduced anxiety, increased satisfaction, improved coping mechanisms and greater caregiver involvement when timely and effective information was provided by healthcare workers in a compassionate and understanding manner.[7],[8],[9],[10]
In India, traditionally families assume a major care-giving role because of the culture of interdependence that is instilled in individuals early in life.[11] Studies have documented how Indian families deal with caring for a chronically ill person, as in looking after the elderly and have reported issues concerning burden and burn-out.[11],[12],[13],[14] However, there is paucity of data on perceptions of Indian families about intensive care. This qualitative component was thus done as part of a larger study that evaluated cost utility of sick medical patients treated in an ICU.[15] More specifically, the qualitative component of the study attempted to understand family caregivers' perceptions of what ICU care meant to them, the challenges they faced with regard to decision-making and their perceptions on the nature of their relationship with healthcare providers in whose care their family members had been entrusted.
Methods
We did a study of caregivers of patients admitted to the medical ICU of a 2500-bed university affiliated, private teaching hospital in southern India. A sub-set of caregivers from the main study[15] were approached and their consent was sought to participate in semi-structured interviews (SSIs). Maximum variation sampling was used in selecting caregivers for the SSIs, which enabled selection of caregivers from different socioeconomic/geographical strata as well as those caring for patients admitted to the ICU for a variety of health problems. The interview guide asked specific questions on their understanding of intensive care, issues concerning caring for their ill relative admitted in the ICU, challenges they faced with regard to decision-making and their experiences with regard to the nature of communication they had with their healthcare providers. The guide ensured that all issues were discussed consistently in every interview.
Procedure
The SSIs were conducted with consenting English-or Tamil-speaking caregivers on any day during the patient's stay in hospital, which was convenient for them. Each interview took 30–40 minutes and was conducted in a private place within the hospital premises. All interviews were recorded after obtaining consent. The interviews were then transcribed verbatim and entered in a qualitative software (NVivo) for further analysis.
Qualitative analysis
We used the framework analytical approach[16] to analyse interview data, which began with the process of data immersion. This involved repeated readings of each interview transcript for gaining familiarity with the data. It also enabled identification of emergent themes that best explained the research questions. The data were carefully sifted, quotes were selected which were then placed under the appropriate thematic content, and interpretations were drawn. Each transcript was coded inductively. A coding framework was then developed after coding five interviews, which guided the coding of the remaining interviews. New codes were added as and when new issues emerged while coding the transcripts. Once all the interviews were coded, segments of text that seemed to relate to a common theme were pieced together and the emergent themes were finalized.
Results
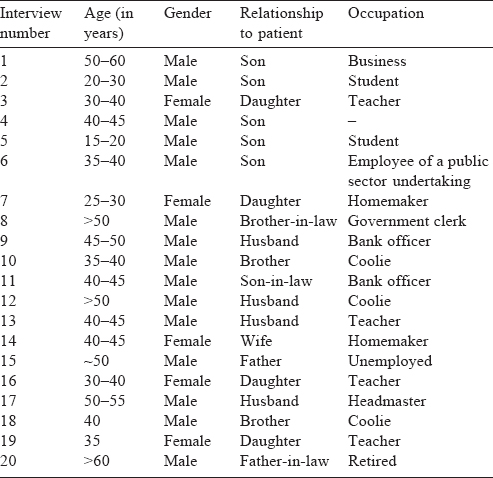
Twenty family caregivers (15 males, 5 females), caring for patients admitted to the ICU for problems ranging from severe infections, chronic lung and heart diseases to suicidal attempts through using organophosphorus pesticides, consented to participate in the interview.
Of the 5 female participants, 2 were homemakers while the remaining 3 were teachers. All the 3 teachers were daughters of respective patients; 1 homemaker caregiver was a wife and the other was a daughter. Two of the male caregivers were students while the rest barring 1, who had retired, were currently employed in odd jobs [Table - 1]. In terms of their relationship to the patient, the most common were son (n=5), husband (n=4) and brother (n=2). Apart from 4 participants who had minimal to no literacy, all others were educated. The emergent themes of analysis were:
— Understanding about the ICU
— Decision-making concerning ICU treatment
— Relationship with healthcare-providers.
Understanding about the ICU
Respondents had varied opinions about the ICU. Most perceived it as a place where emergency treatment was given and believed that it was particularly needed for patients who were extremely ill and struggling for life. Some also said that because the ICU was a sterile place, seriously ill patients were kept there so that they would be protected from infections. Respondents commonly reported that patients with serious heart conditions, poison/accident cases, patients suffering from kidney failure and other complex illnesses required ICU care. However, a few respondents were not clear as to what an ICU was for. Apart from being aware that it was in the hospital, they were not able to say what an ICU meant or what illnesses warranted ICU care. A few saw the ICU as a place where patients in the last stage of their illness were kept, from which survival was difficult. They thus looked upon the ICU with fear.
I don't know what they're doing inside… But, from their side, they are doing their work. Even then, we don't know anything and we're wondering, and we don't know whether they are doing it properly or not. That's how people think. (Male, spouse, number 13)
When the patient is going for ICU treatment, relatives will worry whether the patient will survive or not. This doubt is always there, we don't know whether the doctors are aware about this or not, but the public has this fear. (Female, daughter, number 19)
The ICU was also seen as an expensive care facility. Various specialized equipments that were used in the ICU combined with the medicines that were provided to sick patients contributed to the overall cost. Most respondents were not clear what exactly happened inside the ICU and felt that little information was provided to them by the ICU staff regarding the condition of the patient. The majority opinion was that any individual requiring ICU care must be given it irrespective of his/her age and stage. They believed that families in general wanted their ill relative to recover and would mostly go all out to help that person.
There is no age limit like that; no one is willing to lose their relatives. There are daughters of elderly patients aged over 85 years who are all sitting outside the ICU waiting for their father's improvement. No one will think like this, ‘anyhow he is old, what is the point in [his] living’. (Female, daughter, number 19)
Decision-making
Decision-making about ICU care was an extremely complex and emotional issue for families. The most important thing for them was to see the recovery of their ill relative. Therefore, making sure that the patient had access to good care was crucial. To this end, many reported going all out to raise the money required, even to the extent of going into debt. Having the financial capacity to meet such expenses was thus considered a great help. One participant said:
Emotionally, you're so attached, you just cannot decide. We always have hope and we always pray for miracles to happen. Like, they'll improve. It's the human tendency to think that way. (Female, daughter, number 3)
However, a few were more selective and went on to say that if the patient was elderly, over 80 years of age, the chances of such a person making a full recovery were slim. Therefore, in such cases, keeping the financial status of the family in mind, they may withdraw or decide against placing the individual in the ICU. The financial status of the family was thus a key element in determining the length of ICU care and also its requirement. Families which lacked financial resources were obviously at a disadvantage. The relationship of the family caregiver with the sick person was another factor that was reported by many caregivers to influence the amount of resources the caregiver was willing to spend. In cases where this relationship was a close one, intense fears and concerns about the prognosis and health of their ill relative was a dominant emotion that coloured their every waking thought, thereby contributing to much emotional trauma among family caregivers. However, all respondents emphasized that eventually it was the doctor who was the main deciding authority and that decision was what all families respected and abided by.
It is a professional decision. I don't think it has got anything to do with the patient or patient's relative… Definitely, monetary aspect is there… But the patient or the family member cannot decide whether somebody needs to be in intensive care unit. I think it has to be left to the doctors who are professionals. (Male, spouse, number 11)
I did not want my mother to suffer. That's what I thought. God, you should save my mother… If you give back my mother, God please give her without any pain. Don't give me my mother with pain. That's how I prayed. My friends scolded me and said don't talk like a child. I said I cannot tolerate to see her suffering so much. They poke her here and there and there's no blood. I don't want to see her in pain. (Female, daughter, number 16)
When it came to decision-making and cost of care, some respondents believed that as the chances of survival improved, the cost of care would reduce. They felt that as the patient got better, the amount of resources required to sustain the patient would become less (i.e. less expensive medications, less dependency on expensive medical equipment). Others said that deciding on ICU care or continued stay in an ICU should not be at the cost of the ‘family's future’ particularly if the patient's prognosis was not good. Another opinion was that keeping a patient in ICU beyond 20 days was pointless. This was an unnecessary drain on family resources. Thus, if the patient did not recover within that time, it was best to withdraw the patient from the ICU. A few spoke in terms of percentage survival and said that if a patient was given an 80% survival rate, ICU treatment could be stopped because there was a strong likelihood that such a patient had made it through the worst part of the illness. However, if a patient was reported to be having a 30%–40% chance of survival, then such a patient needed to be placed in an ICU which would hopefully aid in his/her recovery.
My personal opinion is that in ICU, if the medical expense goes very high, then because of that the future of the family should not be spoilt. Suppose I spend ₹20 lakh; even after spending Ψ20 lakh if the patient dies, it is a burden on the future of the family. In that case, we'll call it as ‘unnecessary expense’… the family's future should not be affected. (Male, son, number 1)
Keeping [the patient] for more days in the ICU is really a waste[of resources]. If they are okay within 10 days, no problem. It is very difficult to keep the patient in the ICU for 20 days or one month. The patient may not survive; patients rarely survive. If you keep your patient in the ICU for so many days, the doctors will also keep trying. But really, it's a waste [of resources]. (Female, spouse, number 14)
The huge cost of care was seen as a major challenge, which in turn influenced decision-making for families. A few respondents were able to mention a clear amount that was within their resources, which they felt they would be both willing and able to spend to aid the recovery of the patient. A few others said it was difficult to give a ‘cost for life’ and were hard put to come up with an amount. A few said that ICU costs at this facility were by and large reasonable, considering the resources used and the efforts of the medical team. Others expressed concerns about being criticized by society if they did not aggressively seek the best quality care for their ill relative, which was irrespective of their financial capabilities.
For buying something like a TV or computer, it costs around ₹20 000. They might ask for ₹25 000, then we can bargain and ask them to reduce [the cost]. How can we give a cost for life? (Male, spouse, number 13)
People like me, and I'm saying in general, the middle class really gets affected. There is the prestige issue. Local people will say, ‘see they are in this position [to afford], but not taking care of their father, if the father was given good treatment or ICU treatment or taken to a big hospital he would have been alive. But, his children didn't take care of him.’ So, many are worried about what people will say. (Male, brother-in-law, number 8)
Relationship with care-providers
Most caregivers wanted doctors to talk to them about the patient's condition. Information provided by nurses were also valued but the respondents preferred hearing it from the doctor and felt satisfied only after the doctor had spoken to them and given them the details of the patient's condition. This total faith in the doctor, who was seen by most family members as being next to God, was evident from their narratives. Leaving decision-making to the doctor was the most commonly stated opinion.
My wife had TB spine which was diagnosed following a CT scan. All doctors I saw earlier said she will die. I then came to this hospital and asked Dr S, ‘Sir, people are telling like this. She is a mother of two children. My son is in 2nd standard and my daughter is 2 months old. So, what are the chances?’ He looked at me and said, ‘You pray to God, we will also do our best.’ That was his answer. And I saw God in him. I tell you, on the third day after the surgery he made her walk. (Male, son-in-law, number 11)
My husband was taken to the ICU in the morning, at 6 a.m. They said he had no pulse; he was alive because of artificial respiration. They told us to pray to God, pray to Jesus. I prayed that I get him back. Now also I believe Jesus. My husband was in a serious condition, but Jesus saved him. Without God there is no doctor and without doctors there is no God. Both of them should be there. (Female, spouse, number 14)
No, I didn't ask the doctor anything much about her condition. After all who am I to ask the doctor? I do not feel it right to ask questions; he may not like it. (Male, father, number 15)
Some respondents however did feel that not much information was being given to them. Often they had to repeatedly ask the nurses and other junior doctors before they got any information about the health status of the patient. They spoke of wanting detailed information which they felt was necessary for them to both understand the case and make necessary decisions. At the same time, the patient too needed to be encouraged and reassured, which according to them was best done by the doctor. Often, doctors had very little time to spare with the patient and with family members, which was distressing to them. Conflicting information about the patient's progress in the ICU being given by different ICU staff was another factor reported by some caregivers that contributed to their sense of confusion, even fear. In this context, caregivers stressed the importance of doctors communicating the details of patient's illness in simple terms and being able to honestly answer the questions posed by family members. Quite often the doctors were held in such awe that many hesitated to even ask questions for fear of offending them or for appearing rude. However, a few said that they did not want to be burdened with too many details regarding the patient's condition as this would only distress them more. The doctor was most qualified and knew what to do and they believed in entrusting their family member to the doctor's care and simply following doctor's orders.
Nobody is telling us the condition of the patient [doctors and nurses]… During visiting hours we go and see the patient, we ask them, ‘How is my son?’ They will say ‘as he was in the morning, the same condition he's in now too’. At other times if we ask them, they say ‘please wait we will ask and tell [you]’, but then they never tell [anything]. (Male, parent, number 15)
Only doctors should tell… That is what gives assurance. Even if there are any negative issues, they only should convey them… Whether it's the relatives or friends, who are with them [the patients], should feel that ‘we need to give treatment’, ‘we need to spend [money]’; Doctors should make them think like that. (Male, spouse, number 13)
I feel the ICU staff and doctors should not give too much information to relatives. I have been here for 35 days. I have seen family members crying.other people who are next to them will ask the condition of the patient, and everybody will come to know. So, many times all this information [about the patient's status] is not necessary, it only adds to the stress. (Male, parent, number 15)
Doctors should follow professional ethics and should be qualified enough to consider if the person should go to the intensive care unit. They should have the ability to discuss [the issues]. I cannot understand few technical terms. Some may not understand anything at all. So, doctors should use some language that the patient/caregivers understand… ‘If you keep him in the ICU, this will be the extra cost or extra requirement’, whatever it is. ‘But, this will be the outcome…’ Nobody can predict other than God, nobody can say if they are going to be alive or not? We can say these are the advantages or disadvantages. I think that much should be discussed. (Male, son-in-law, number 11)
Patient's relatives are concerned about the patient. If the doctor speaks in a good tone and spends [some] time with them, they will be happy. If they [doctors] speak rudely, it will add to their [relatives'] tension. (Male, son, number 6)
Discussion
This qualitative study sought to understand family caregivers' perceptions about intensive care, the challenges they faced in terms of decision-making and their relationship with healthcare providers. The use of qualitative research methods with its emphasis on the emic point of view is an excellent way of obtaining such insights as it provides an understanding into the thoughts and feelings of individuals; in this case, family caregivers.
Qualitative research methods have been increasingly used in the ICU setting to examine issues such as communication with families,[17] end-of-life care[18] and patient safety[19] and to gain deeper insights into the experiences, beliefs and actions of ICU clinicians, patients and families. In this qualitative study in an Indian ICU setting, it was evident that family caregivers experienced tremendous stress, not just on account of the pressure of decision-making on behalf of their ill relative and of seeing them suffer, but also on account of having to deal with the uncertainty of length of stay and its impact on their strained financial resources. Added to this were their concerns about possible societal criticisms being levelled against them for not being proactive enough in providing care to their ill relative. Thus, it is obvious that family caregivers carry a huge burden. In the light of this, if healthcare professionals are mindful of what families are experiencing and feeling and be more communicative and empathetic, it would translate to improved caregiver participation, increased satisfaction and strengthen their role in enabling patient recovery.
Decision-making about continuing ICU care was fraught with problems for caregivers. Despite leaving much of the decision-making to the doctor, family caregivers still wanted to understand the condition of their ill relative and to receive regular updates on the patient's progress and this is where they faced problems. Quite often, the information they received was sketchy, or not easily understood or confusing thereby adding to their stress. This was compounded by the fact that many family members were unclear about the prognosis of their ill relative. Issues concerning the spiralling cost of care, and their concerns about their financial capability to meet those demands were a constant stressor reported by many family members. Their attempts to understand the patient's condition were often met with cursory or even conflicting responses sometimes in a language they found hard to comprehend. While many were comfortable receiving the information on the patient's condition from nurses and other junior doctors, the preference was to hear it all from the treating doctor. Mitnick et al.[2] stressed the importance of providing family caregivers with adequate information and access to resources that would enable them to be more effective in their roles as caregivers. They stressed the value of physicians addressing the physical and emotional needs of caregivers, thereby serving to recognize the importance of their roles as caregivers. Medland and Ferrans[20] described how family caregivers preferred receiving information on their ill relative from a single doctor in a personalized manner as this would help avoid contradictions. The need for family caregivers to receive effective and intelligible information clear of any inconsistencies cannot therefore be over-emphasized. Other studies have highlighted the need of family caregivers to be able to visit their ill relative in the ICU, to obtain regular updates on the patient's progress and to be assured that the patient was receiving the best care.[21] Azoulay et al.[6] underscored the need for physicians to determine whether the information imparted to family members had been adequately understood, and stressed that the technical terms that physicians often tended to use interfered with the ability of family members to comprehend what was being conveyed, resulting in lowered satisfaction among family members. They emphasized the need for physicians to be sensitive to cultural differences in family members which could contribute to gaps in them comprehending the information provided.
Another important finding of our study, which is also typical of our culture, was the immense faith that people in general—in this context family members—reposed in the doctor. The doctor was seen as next to God and therefore the one most empowered to make decisions concerning the patient. Family caregivers often felt diffident to ask questions to the doctor. Studies have described that the most common reason for not asking questions to the doctor were because of fears of appearing poorly in their eyes, coupled with the belief that asking questions would annoy the doctor, which in turn may affect quality of care for their ill relative.[22] The authors describe that doctors accentuate these beliefs by behaving as if they were ‘on a higher plane when compared to the patient and thereby more empowered to make these decisions’. The importance of doctors being compassionate and kind and of being forbearing in addressing their concerns was reiterated by most family caregivers. By virtue of their expertise and knowledge in the field, doctors indeed may be the best persons to shoulder the responsibility of advising family caregivers. However, this also imposes on the doctor the critical responsibility of being open and honest with the caregivers, thereby establishing a relationship of trust. Such a relationship can best be achieved through being compassionate and forbearing in addressing their doubts and concerns and by spending adequate time with them. Azoulay et al.[23] highlighted that by spending ‘sufficient’ time with the family, doctors helped caregivers deal with and come to terms with the illness of their relative.
Some limitations merit attention. The interviews were conducted only with the family caregivers. Perspectives of doctors and nurses in the ICU would have provided insights on barriers and problems faced in dealing with patients and family caregivers and challenges in communicating highly technical information in a simple manner. Further, our study did not explore specific health repercussions of ICU admission on the family caregiver. While there is abundant literature on such issues from developed countries, this has remained a relatively less explored field in India and therefore provides scope for further work.
In conclusion, our study attempted to understand family caregivers' perceptions on intensive care and has highlighted the considerable financial, emotional and medical constraints they face. The need to improve family caregiver satisfaction through clear and simple communication strategies and through effective psychological support would go a long way in improving their well-being and in enhancing their caregiver role.
Acknowledgements
The study was funded by internal funds from the institution and by the individual departments.
Conflict of interest. None declared.
| 1. | Evans R, Catapano MA, Brooks D, Goldstein RS, Avendano M. Family caregiver perspectives on caring for ventilator-assisted individuals at home. Can Respir J 2012;19:373–9. [Google Scholar] |
| 2. | Mitnick S, Leffler C, Hood VL, American College of Physicians Ethics, Professionalism and Human Rights Committee. Family caregivers, patients and physicians: Ethical guidance to optimize relationships. J Gen Intern Med 2010;25:255–60. [Google Scholar] |
| 3. | Whitlatch CJ, Judge K, Zarit SH, Femia E. Dyadic intervention for family caregivers and care receivers in early-stage dementia. Gerontologist 2006;46:688–94. [Google Scholar] |
| 4. | Whitlatch CJ, Feinberg LF. Family care and decision making. In: Dementia and social work practice: Research and intervention [Internet]. New York:Springer; 2007:129–7. Available at www.springerpub.com/dementia-and-social-work-practice.html (accessed on 20 Apr 2016). [Google Scholar] |
| 5. | Choi J, Hoffman LA, Schulz R, Ren D, Donahoe MP, Given B, et al. Health risk behaviors in family caregivers during patients' stay in intensive care units: A pilot analysis. Am J Crit Care 2013;22:41–5. [Google Scholar] |
| 6. | Azoulay E, Pochard F, Chevret S, Lemaire F, Mokhtari M, Le Gall JR, et al. Meeting the needs of intensive care unit patient families: A multicenter study. Am J Respir Crit Care Med 2001;163:135–9. [Google Scholar] |
| 7. | Auerbach SM, Kiesler DJ, Wartella J, Rausch S, Ward KR, Ivatury R. Optimism, satisfaction with needs met, interpersonal perceptions of the healthcare team, and emotional distress in patients' family members during critical care hospitalization. Am J Crit Care 2005;14:202–10. [Google Scholar] |
| 8. | Delva D, Vanoost S, Bijttebier P, Lauwers P, Wilmer A. Needs and feelings of anxiety of relatives of patients hospitalized in intensive care units: Implications for social work. Soc Work Health Care 2002;35:21–40. [Google Scholar] |
| 9. | Hardwick C, Lawson N. The information and learning needs of the caregiving family of the adult patient with cancer. Eur J Cancer Care (Engl) 1995;4:118–21. [Google Scholar] |
| 10. | Hickey M. What are the needs of families of critically ill patients? A review of the literature since 1976. Heart Lung J Crit Care 1990;19:401–15. [Google Scholar] |
| 11. | Avasthi A. Preserve and strengthen family to promote mental health. Indian J Psychiatry 2010;52:113–26. [Google Scholar] |
| 12. | Gupta R, Pillai V. Cultural influences on perceptions of caregiver burden among Asian Indians and Pakistanis. Southwest J Aging 2002;17:65–74. [Google Scholar] |
| 13. | Jamuna D, Ramamurti P. Burnout among the caregivers of disabled elderly: Effect of intervention. Psychol Stud 2000;45:150–6. [Google Scholar] |
| 14. | Gupta R, Pillai VK. Elder caregiving in South-Asian families in the United States and India. Soc Work Soc [Internet]. 2012;10 (2). Available at www.socwork.net/sws/ article/view/339 (accessed on 9 Oct 2015). [Google Scholar] |
| 15. | Thomas K, Peter JV, Christina J, Jagadish AR, Rajan A, Lionel P, et al. Cost-utility in medical intensive care patients. Rationalizing ongoing care and timing of discharge from intensive care. Ann Am Thorac Soc 2015;12:1058–65. [Google Scholar] |
| 16. | Ritchie J, Spencer L. Qualitative data analysis for applied policy research. In: Analyzing qualitative data. 1st ed. London:Routledge; 1994:173–94. [Google Scholar] |
| 17. | Curtis JR, Engelberg RA, Wenrich MD, Nielsen EL, Shannon SE, Treece PD, et al. Studying communication about end-of-life care during the ICU family conference: Development of a framework. J Crit Care 2002;17:147–60. [Google Scholar] |
| 18. | Curtis JR, Engelberg RA, Wenrich MD, Shannon SE, Treece PD, Rubenfeld GD. Missed opportunities during family conferences about end-of-life care in the intensive care unit. Am J Respir Crit Care Med 2005;171:844–9. [Google Scholar] |
| 19. | Rocker GM, Cook DJ, Martin DK, Singer PA. Seasonal bed closures in an intensive care unit: A qualitative study. J Crit Care 2003;18:25–30. [Google Scholar] |
| 20. | Medland JJ, Ferrans CE. Effectiveness of a structured communication program for family members of patients in an ICU. Am J Crit Care 1998;7:24–9. [Google Scholar] |
| 21. | Plaszewska- -Zywko L, Gazda D. Emotional reactions and needs of family members of ICU patients. Anaesthesiol Intensive Ther 2012;44:145–9. [Google Scholar] |
| 22. | Kumar S, Mohanraj R, Rose A, Paul MJ, Thomas G. How ‘informed’ is informed consent? Findings from a study in South India. Indian J Med Ethics 2012;9:180–6. [Google Scholar] |
| 23. | Azoulay E, Chevret S, Leleu G, Pochard F, Barboteu M, Adrie C, et al. Half the families of intensive care unit patients experience inadequate communication with physicians. Crit Care Med 2000;28:3044–9. [Google Scholar] |
Fulltext Views
2,364
PDF downloads
1,834




