Translate this page into:
Clinical profile of patients and sensitivity of troponin I in patients with and without acute coronary syndrome: An observational study
Correspondence to SHRUTHI M. KULKARNI; shruthi.mk@stjohns.in
[To cite: Kulkarni SM, Roongta R, Sankar S. Clinical profile of patients and sensitivity of troponin I in patients with and without acute coronary syndrome: An observational study. Natl Med J India 2023;36:305–9. DOI: 10.25259/NMJI_801_2021]
Abstract
Background
Various clinical conditions can cause troponin elevation in the absence of myocardial ischaemia. Elevated troponin represents the likely occurrence of myocardial necrosis and does not itself provide any indication of the aetiology. Identifying the cause for troponin elevation and its sensitivity and specificity in predicting acute coronary syndrome (ACS) and cardiac mortality is an important step in determining the optimal management for these patients.
Methods
We retrospectively collected data of inpatients who had troponin I (TnI) testing as part of their clinical assessment, either in the emergency department, medical wards, coronary care unit (CCU) or intensive care unit (ICU) with their final diagnosis. TnI was used as the index test of sensitivity to diagnose ACS and either echocardiography or coronary angiogram in those available as the reference gold standard. They were classified into two groups of normal and elevated TnI, and further divided into those with ACS and no ACS. Data on clinical parameters and aetiology of elevated TnI in patients without ACS were analysed.
Results
Of the 254 patients studied, 114 patients (45%) had normal TnI and 140 (55%) had elevated TnI. Seventy-eight patients had ACS, 66 (84.6%) of whom had elevated TnI and 12 (15.38%) had normal TnI. Seventy-four (52.85%) of 140 patients with elevated TnI had alternate causes of TnI elevation; the most common being sepsis, acute kidney injury (AKI) and heart failure without ACS. All-cause mortality was significantly higher in patients with elevated TnI with or without ACS. There was no cardiac mortality among patients with ACS with normal TnI. Sensitivity and specificity of TnI for predicting ACS was 84.6% (95% CI 74.7%–91.8%) and 58% (95% CI 50.3%–65.3%), respectively.
Conclusion
A variety of conditions apart from myocardial infarction can lead to elevated TnI. Hence, caution should be exercised while diagnosing a patient with ACS based on TnI value in the absence of other supporting evidence given its low specificity. Elevated TnI portends a worse prognosis regardless of the aetiology and has a role in predicting all-cause and cardiac mortality.
INTRODUCTION
Ischaemic heart disease remains a leading cause of death. Analysis of serum cardiac markers have become crucial for early diagnosis of acute coronary syndrome (ACS)1 as electrocardiograph (ECG) can be non-diagnostic in 50%–60% of patients with MI coming to the emergency department and less than 80% have classical symptoms of chest pain. The most reliable of the cardiac marker assays, troponin assays, can be detected quickly and repeated serially with a half-life of 2 hours. These assays have become more sensitive, with the ability to quantify troponin levels even in the normal population, making the interpretation of this test difficult. Cardiac troponin (Tn) elevation reflects acute or chronic myocardial damage but is not exclusive for ACS, thereby causing difficulty in its interpretation.2–4
There are various causes of Tn elevation in the absence of myocardial infarction, broadly due to oxygen demand mismatch (tachyarrythmias/bradyarrythmias, hypertensive crisis), direct myocardial damage (cardiac infiltrative disorders, chemotherapy) and systemic processes (sepsis, burns), etc.3–6 It is important to exercise caution when interpreting elevated Tn values for diagnosing ACS in the absence of other features such as chest pain and ECG changes. Elevations in cardiac Tn, regardless of aetiology, portend a worse prognosis, even in those without heart failure (HF), obstructive coronary artery disease, or significant kidney dysfunction.7 The clinical significance of elevated troponins in non-cardiac conditions is not completely known. Also, it is unclear if these clinical conditions need to be managed differently when they lead to an increase in Tn levels.8
Identifying the cause for Tn elevation and its sensitivity and specificity in predicting ACS and cardiac mortality is an important first step in determining the optimal management for these patients. Hence, we proposed a hypothesis that among patients presenting with symptoms suggestive of ACS, TnI, as an index test has high sensitivity and specificity to diagnose ACS (target condition) and the study aimed to determine the sensitivity and specificity of TnI among medical inpatients diagnosed with ACS and to look for an alternative diagnosis in those with elevated TnI and no ACS.
METHODS
We conducted a retrospective study of adult inpatients who had TnI testing as part of their clinical assessment. The decision to test for TnI was at the discretion of the treating physician, for suspected ACS1 and did not influence the inclusion of patients. We collected data from medical records and included adult inpatients who had TnI testing, either at admission or later, either at the emergency department (ED), or admitted in medical and cardiology wards, intensive care unit (ICU) or cardiac care unit (CCU). Patients were identified from the TnI test registers maintained in the respective departments of clinical biochemistry laboratory, CCU and ICU. In those patients who were diagnosed to have ACS, available data on echocardio-graphy/cardiac CT scan and the gold standard, coronary angiogram (CAG) were collected. Various departments were selected to have a heterogeneous population to minimize selection bias. Pregnant women were excluded. The diagnosis of ACS was made by the presence of two of the following: Symptoms of ischaemia and/or ischaemic changes on ECG and/or evidence of ischaemia on imaging, and elevated TnI.1 The absence of these features, alongside the clinical picture of an alternative diagnosis, confirmed conditions other than ACS.
Measurement of TnI
TnI, with its high sensitivity and specificity is the recommended cardiac biomarker to measure myocardial injury, according to the American Heart Association (AHA)/American College of Cardiology (ACC).1 We had two different assays to measure cardiac TnI in our hospital, AQT90 FLEX immunoassay analyser used by the emergency department and CCU in their respective departments and the chemiluminescent immunoassay (CLIA), used by the hospital biochemistry laboratory. Patients admitted to the emergency department or directly to the CCU underwent the FLEX immunoassay. Patients admitted to medical wards/ICU underwent the CLIA method of TnI testing. TnI was considered elevated if it was above the upper limit of the value prespecified by the manufacturer for that assay, 0.01 mg/L and 0.034 mg/L for FLEX immunoassay and CLIA, respectively. When the first TnI result was indeterminate or normal, a serial test at an interval of 6 hours along with ECG was done and the serial rise or fall was considered positive or negative, respectively. As we used two different commercial assays, TnI test result was considered as a qualitative parameter of whether normal or elevated for analysing our study results. Commercially available assays are not standardized and have documented differences across methods.9 The reasons being the lack of commutable reference and difference in the antibody immuno-reactivity as well as in the antigen used as calibrators.10
Based on the clinical diagnosis and the TnI result, we categorized patients into four groups: (i) elevated TnI with ACS (TEAP); (ii) elevated TnI without ACS (TEAA); (iii) normal TnI with ACS (TNAP); and (iv) normal TnI without ACS (TNAA). Patients were followed up till discharge and their demographic data, comorbid conditions, investigations, final diagnosis and outcome were recorded to assess the aetiology of elevated TnI with or without ACS.
Based on the study by Wong et al.11 raised cardiac TnI levels in patients without ACS with 5% significance and 20% precision, we needed 200 patients for the study.
Statistical analysis
Descriptive data were represented as percentage and frequencies. Chi-square and Fisher exact tests were used for comparing categorical variables. Student t-test was used for comparing group means. Sensitivity and specificity of TnI, positive and negative predictive values for all cause and cardiac mortality were calculated based on true and false-positives, and true and false-negatives. A value of p<0.05 was considered statistically significant. Data were analysed using SPSS version 20 for Windows.
RESULTS
A total of 254 patients were included for analysis, 114 patients (45%) had normal TnI and 140 (55%) had elevated TnI. Twelve (10.5%) patients with normal TnI and 66 (47%) patients with elevated TnI had ACS. Of the 78 patients who had ACS, 66 (84.6%) had elevated TnI and 12 (15.38%) had normal TnI (Fig. 1).
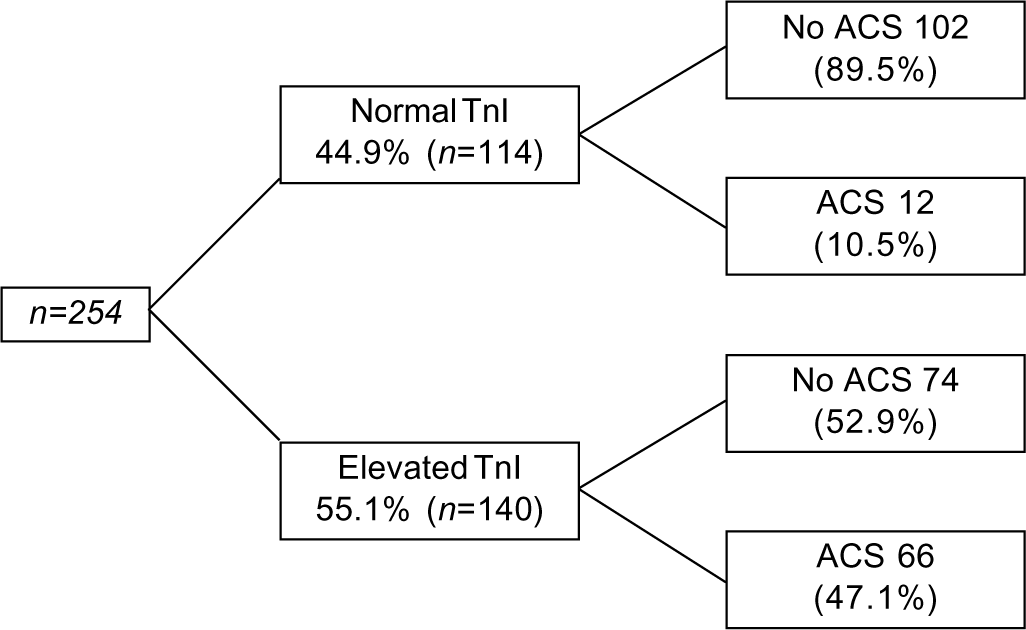
- Distribution of patients TnI troponin I ACS acute coronary syndrome
The mean (SD) age of all patients was 56.67 (16.87) years. The mean (SD) age of patients with ACS irrespective of TnI was 62.9 (12.0) years and those without ACS was 54 (18) years (p<0.001). Of the 254 patients, 156 (61.4%) were men and 98 (38.6%) were women. The baseline characteristics of patients across the four groups showed significant differences. Age, history of chest pain and smoking, and ICU admission were higher in patients with ACS with or without elevated TnI. Comorbid conditions were higher in patients with elevated TnI, with or without ACS. Of the 254 patients, 106 (41.73%) had diabetes and mean (SD) duration of diabetes was 11.7 (8.6) years. One hundred and twenty-four patients (48.8%) had hypertension and the mean (SD) duration of hypertension was 10 (8.3) years, 58 (22.8%) were known to have ischaemic heart disease, of which 27 (10.6%) had undergone coronary revascularization (Table I).
| Variable | TEAP (n=66) | TEAA (n=74) | TNAP (n=12) | TNAA (n=102) | p value |
|---|---|---|---|---|---|
| Mean (SD) age (years) | 63.5 (12.6) | 54.7 (19.4) | 59.8 (8) | 53.3 (17) | <0.001 |
| Gender (men) | 4 6 | 34 | 8 | 68 | 0.01 |
| Chest pain | 45 | 10 | 10 | 26 | <0.001 |
| Breathlessness | 26 | 36 | 2 | 32 | 0.05 |
| Smoking | 31 | 13 | 6 | 19 | <0.001 |
| Type 2 diabetes mellitus | 33 | 29 | 8 | 36 | 0.07 |
| Hypertension | 35 | 30 | 6 | 53 | 0.40 |
| Previous ischaemic heart disease | 19 | 18 | 5 | 16 | 0.06 |
| Abnormal electrocardiogram | 64 | 30 | 1 1 | 53 | <0.001 |
| Heart failure (known case) | 31 | 21 | 3 | 14 | <0.001 |
| ST elevated myocardial infarction | 22 | 0 | 5 | 1 | <0.01 |
| Regional wall motion abnormalities | 53 | 10 | 1 0 | 12 | <0.001 |
| Mean (SD) ejection fraction | 43 (12.5) | 55 (13.9) | 50 (12.6) | 61 (9.74) | <0.001 |
| Sepsis | 6 | 21 | 0 | 9 | <0.001 |
| Hypotension | 10 | 22 | 0 | 4 | <0.001 |
| Myocarditis | 0 | 13 | 0 | 4 | <0.001 |
| Acute kidney injury | 12 | 21 | 2 | 12 | 0.05 |
| Cardiomyopathy | 1 | 6 | 1 | 2 | 0.1 |
| ICU admission | 54 | 37 | 8 | 26 | <0.001 |
TEAP elevated TnI with acute coronary syndrome (ACS) TEAA elevated TnI without ACS TNAP normal TnI with ACS TNAA normal TnI without ACS ICU intensive care unit
Presenting complaints, ECG and echocardiogram findings
Of the 254 patients, 91 (35.8%) presented with chest pain. Of these 91 patients, 55 (60.4%) patients had elevated TnI and 55 (60.4%) patients had ACS. Forty-five (49.5%) patients had a combination of ACS, elevated TnI and chest pain. Of the 140 patients with elevated TnI, 55 (39.3%) had complaints of chest pain and 62 (44.3%) presented with breathlessness (p=0.01). Of the 78 patients with ACS, 55 (70.5%) presented with chest pain (p<0.001) and 28 (35.9%) presented with breathlessness.
Of the 254 patients, ECG was normal in 96 (37.8%) and abnormal in 158 (62.2%) patients. Among the 158 patients with abnormal ECGs, 75 (47.5%) had ACS and 94 (59.5%) had elevated TnI. ST elevation was more frequent in patients with elevated TnI (78.5% v. 21.4%, p<0.005) than those with normal TnI and in patients with ACS (96.4% v. 3.6%, p<0.001) than in those without ACS.
ST depression was more frequent in patients with elevated TnI (72.2% v. 27.8%, p<0.05) than in those with normal TnI and in patients with ACS (75% v. 25%, p<0.001) than in those without ACS. Twenty-seven (96.4%) patients with ST elevation had ACS and 27 (75%) with ST depression had ACS. Presence of bundle branch blocks were significantly higher in patients with elevated TnI (p<0.005) and with ACS (p<0.001). Of the 140 patients with elevated TnI, 63 (45%) had regional wall motion abnormality (RWMA) on echocardiography (p<0.001). TnI was normal in 22 (25.9%) of 85 patients with RWMA. Mean ejection fraction (EF) was lower in patients with elevated TnI (49.5%) than in those with normal TnI (59.6%). Mean EF was lower in patients with ACS (44.5%) than those without ACS (58.2%).
Of the 78 patients with ACS, 28 (36%) had ST elevation myocardial infarction (STEMI), 47 had non-STEMI (60%) and 3 (4%) patients had unstable angina.
Alternative diagnosis of elevated TnI (Table II)
Sepsis, HF and acute kidney injury (AKI) were the commonest causes of elevated TnI in the absence of ACS and they were present in combination in 38 patients.
| Alternative diagnosis | Elevated TnI (n=140) n(%) | Normal TnI (n=114) n(%) | p value |
|---|---|---|---|
| Heart failure (newly diagnosed) | 52 (37) | 17 (15) | <0.001 |
| Sepsis | 27 (19) | 9 (8) | 0.11 |
| Myocarditis | 13 (9.2) | 4 (3.5) | 0.08 |
| Arrythmias | 5 (3.5) | 3 (2.6) | 0.73 |
| Accelerated hypertension | 9 (6.4) | 3 (2.6) | 0.23 |
| COPD/asthma exacerbation | 4 (2.8) | 6 (5) | 0.35 |
| Acute kidney injury | 33 (23.5) | 14 (12) | 0.02 |
| Chronic kidney disease | 13 (9.2) | 11 (9.6) | 1.00 |
| Malignancy | 5 (3.5) | 3 (2.6) | 0.73 |
COPD chronic obstructive pulmonary disease
Of the 69 patients with HF, 34 (49.3%) had ACS. Thirty-one of 78 patients with ACS had HF at presentation. For 4 patients no discernible cause for elevated TnI was found. Significant TnI elevation was observed in patients with HF, sepsis, hypotension and AKI (p<0.05).
In patients with a diagnosis of ACS, mean age, history of chest pain, smoking and diabetes, ST elevation and depression on ECG and RWMA on echocardiogram, were found to be significant than those without ACS, regardless of TnI levels (Table III).
| n (%) | n (%) | ||
|---|---|---|---|
| Variable | ACS (n=78) | No ACS (n=176) | p value |
| Mean (SD) age (years) | 63 (12) | 54 (18) | <0.001 |
| Women | 24 (30.7) | 74 (69.3) | 0.09 |
| Chest pain | 55 (70.5) | 36 (20.5) | <0.001 |
| Breathlessness | 28 (40) | 68 (38.6) | 0.77 |
| Smoking | 37 (47.4) | 32 (18.2) | <0.001 |
| Alcohol | 14 (18) | 14 (8) | 0.03 |
| Type 2 diabetes mellitus | 41 (52.5) | 65 (37.5) | 0.03 |
| Hypertension | 41 (52.6) | 83 (47) | 0.49 |
| Dyslipidaemia | 9 (11.5) | 9 (5) | 0.10 |
| Previous ischaemic heart disease | 24 (30.7) | 34 (19.3) | 0.05 |
| Heart failure | 4 (5) | 7 (4) | 0.74 |
| COPD/asthma | 5 (6.4) | 13 (7.4) | 1.09 |
| Normal electrocardiogram | 3 (3.8) | 93 (52.8) | <0.001 |
| ST elevation | 27 (34.6) | 9 (5) | <0.001 |
| ST depression | 27 (34.6) | 9 (5) | <0.001 |
| Left bundle branch block | 19 (24.3) | 15 (8.5) | 0.001 |
| Regional wall motion abnormalities | 63 (80.7) | 22 (12.5) | <0.001 |
| Previous CRT | 11 (14) | 16 (1) | 0.27 |
COPD chronic obstructive pulmonary disease CRT cardiac resynchronization therapy
Of the 78 patients diagnosed with ACS, 35 patients underwent coronary angiogram (CAG; 4 had non-obstructive coronary artery disease, 12 had single vessel disease, 8 had double vessel disease and 11 had triple vessel disease). Among these, 21 patients underwent coronary revascularization therapy (either angioplasty or stenting). Four patients required cardiopulmonary resuscitation at admission, prior to CAG.
Statistically significant (p<0.001) TnI elevation was seen in patients requiring ICU care (n=125). The mean (SD) duration of hospital stay in patients with ACS was 8.24 (5.9) days than those without ACS, 6.84 (4.73) days (p=0.05). Twenty-five (9.8%) patients of 254 died during hospital stay, of which 24 (96%) had elevated TnI (p<0.005). Twelve (4.7%) patients died of cardiac causes.
Sensitivity and specificity of TnI for predicting ACS was 84.6% (95% CI 74.7%–91.8%) and 58% (95% CI 50.3%–65.3%), respectively. The PPV and NPV of TnI to predict ACS was 47.1% (95% CI 42.26%–52.08%) and 89.5% (95% CI 83.27%–93.56%), respectively.
Elevated TnI had 100% specificity in predicting cardiac mortality and good negative predictive value for predicting both cardiac and all-cause mortality (Table IV).
| Troponin I | All-cause mortality | Cardiac mortality |
|---|---|---|
| Sensitivity (%) | 96 (88.3–99.2) | 100 (96–100) |
| Specificity (%) | 49.34 (38.4–56.2) | 47 (37.1–52.6) |
| Positive predictive value | 17.14 | 8.57 |
| Negative predictive value | 99.12 | 100 |
DISCUSSION
Our study details the clinical profile and causes of elevated TnI and outcomes of 254 inpatients from a tertiary care teaching hospital. Of the 254 patients, more than half (140, 55%) had an elevated TnI level. And among these 140 patients with elevated TnI levels, half (74, 53%) had diagnoses other than ACS, a higher number in comparison with an audit done by Wong et al.11 Male predominance in the ACS group was noted in this study as also seen in the other studies.3,11,12 No significant difference was noted between the gender distribution of patients with normal and elevated troponin. We had 47% of patients with elevated TnI having ACS, lower compared to the study by Wong et al. (62.3%).11 We speculate that this difference in the finding between our study and other similar studies could be due to a more sensitive assay used by us leading to detection of minor elevations of troponin even in non-ACS patients with an alternative diagnosis for TnI elevation. There were no significant differences with the medical history and comorbid conditions in the two groups (normal v. elevated TnI).
In our study, patients with ACS and elevated TnI had a significant association with diabetes (53.2%) and history of smoking (70.5%) compared to the study by Khan et al.,3 probably due to lower numbers in their study. Among patients with elevated TnI, we found that more patients with ACS had pre-existing hypertension (53.8%), ischaemic heart disease (51.4%) and chest pain (81.8%) and presence of ST elevation on ECG at presentation than without ACS, similar findings were seen in another study (54%, 45% and 72%, respectively).3 Patients without ACS were less likely than those with ACS to present with ECG changes and chest pain as a major symptom (p<0.001), as noted in a similar study.13
A large number of conditions have been identified for elevation of TnI, other than ACS. Among the 140 patients (55%) with elevated TnI in the absence of ACS, sepsis, AKI and HF were the commonest causes in our study. Significantly higher number of patients and with similar non-ACS aetiologies of elevated TnI were seen in other studies.14,15 The less common causes of elevated TnI in the absence of ACS were myocarditis, cardiac arrest from non-ACS causes, chronic kidney disease, accelerated hypertension and cardiotoxic drugs. We had one patient with pulmonary thromboembolism and 4 patients in whom no diagnosis could be made.
The mean duration of hospital stay in patients with elevated TnI with or without ACS was significantly higher than in those with normal TnI (8.45 [5.9], 5.81 [3.5] days). In-hospital all-cause mortality and cardiac mortality were significantly higher in patients with elevated TnI and ACS (23% and 13.6%) than elevated TnI without ACS (12% and 4%), respectively. This is in contrast to other studies in which non-ACS patients with elevated Tn had significantly higher mortality.11,14 This could be due to the larger sample sizes in these studies.
The sensitivity and specificity of TnI for the diagnosis of ACS was 84.6% and 58%, respectively in our study. These numbers are low compared to other studies as they had excluded non-ACS conditions.15,16 The result may be confounded by the presence of non-ACS aetiologies in patients with ACS in this study. Elevated TnI is an independent predictor of prognosis in patients with ACS.17,18 It is also associated with higher mortality in patients with non-ACS aetiologies.19–22 We found the sensitivity and negative predictive value (NPV) of TnI in predicting all-cause and cardiac mortality to be (96% and 100%) and (99.12% and 100%), respectively.
A few limitations of the study are small sample size, qualitative assessment of TnI, which limit the assessment of possible incremental mortality with increase in TnI and the limited data on coronary angiogram.
In conclusion, TnI can be elevated in several conditions apart from ACS. The assessment of whether TnI elevation is a result of a coronary event or not has become a major challenge and has greater implication to both the hospital and the patient. Caution should be exercised while diagnosing a patient with elevated TnI as having ACS without other supporting evidence and in the setting of an alternative diagnosis. Specificity of TnI can be improved by better test-ordering protocols based on the pre-test probability of the suspected condition. However, TnI has a good negative predictive value in diagnosing ACS and has a role in predicting mortality in patients with and without ACS. Elevated TnI portends a worse prognosis regardless of the aetiology, compelling for a detailed evaluation of both ACS and non-ACS causes. As elevation of TnI indicates myocardial injury even in those with non-ACS cause of its elevation, whether they require longer follow-up and early cardiac evaluation later in life has to be studied.
Conflicts of interest
None declared
References
- 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. In: Circulation. Vol 130. 2014. p. :e344-e426. Erratum in: Circulation 2014;130:e433-4
- [CrossRef] [Google Scholar]
- Troponin elevation in coronary vs. non-coy disease. Eur Heart J. 2011;32:404-11.
- [CrossRef] [PubMed] [Google Scholar]
- Elevation of serum cardiac troponin I in noncardiac and cardiac diseases other than acute coronary syndromes. Am J Emerg Med. 1999;17:225-9.
- [CrossRef] [PubMed] [Google Scholar]
- Elevation of cardiac troponin I indicates more than myocardial infarction. Clin Invest Med. 2003;26:133-47.
- [Google Scholar]
- Common causes of troponin elevations in the absence of acute myocardial infarction. Incidence and clinical significance. Chest. 2004;125:1877-84.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiac biomarkers of acute coronary syndrome: From history to high-sensitivity cardiac troponin. Intern Emerg Med. 2017;12:147-55.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiac troponin elevation in patients without a specific diagnosis. J Am Coll Cardiol. 2019;73:1-9.
- [CrossRef] [PubMed] [Google Scholar]
- A review of cardiac and non-cardiac causes of troponin elevation and clinical relevance. Part II. Non cardiac causes. J Cardiol Curr Res. 2018;11:9-16.
- [CrossRef] [Google Scholar]
- Harmonization of contemporary-sensitive troponin I immunoassays: Calibration may only be a part of the problem. Riv Ital Med Lab. 2014;10:108-14.
- [CrossRef] [Google Scholar]
- Counterpoint: Standardization of cardiac troponin I assays will not occur in my lifetime. Clin Chem. 2012;58:169-71.
- [CrossRef] [PubMed] [Google Scholar]
- Raised cardiac troponin T levels in patients without acute coronary syndrome. Postgrad Med J. 2007;83:200-5.
- [CrossRef] [PubMed] [Google Scholar]
- Acute coronary syndrome vs nonspecific troponin elevation: Clinical predictors and survival analysis. Arch Intern Med. 2007;167:276-81.
- [CrossRef] [PubMed] [Google Scholar]
- The meaning of elevated troponin I levels: Not always acute coronary syndromes. Am J Emerg Med. 2016;34:145-8.
- [CrossRef] [PubMed] [Google Scholar]
- The etiology and prognostic significance of cardiac troponin I elevation in unselected emergency department patients. J Emerg Med. 2010;38:1-5.
- [CrossRef] [PubMed] [Google Scholar]
- High-sensitivity cardiac troponin T compared with standard troponin T testing on emergency department admission: how much does it add in everyday clinical practice? J Am Heart Assoc. 2013;2:e000204.
- [CrossRef] [PubMed] [Google Scholar]
- High-sensitivity versus conventional troponin in the emergency department for the diagnosis of acute myocardial infarction. Crit Care. 2011;15:R147.
- [CrossRef] [PubMed] [Google Scholar]
- The prognostic valve of troponin in patients with non-ST elevation acute coronary syndromes: a meta-analysis. J Am Coll Cardiol. 2001;38:478-85.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiac-specific troponin I levels to predict the risk of mortality in patients with acute coronary syndromes. N Engl J Med. 1996;335:1342-9.
- [CrossRef] [PubMed] [Google Scholar]
- Prognostic use of cardiac troponin T and troponin I in patients with heart failure. Can J Cardiol. 2003;19:383-6.
- [Google Scholar]
- Prevalence of increased cardiac troponin I levels in patients with and without acute pulmonary embolism and relation of increased cardiac troponin I levels with in-hospital mortality in patients with acute pulmonary embolism. Am J Cardiol. 2004;93:263-4.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiac troponin I in patients with severe exacerbatiom of chronic obstructive pulmonary disease. Intensive Care Med. 2003;29:584-9.
- [CrossRef] [PubMed] [Google Scholar]
- Troponin I and T level in renal failure patients without acute coronary syndrome: A systematic review of the literature. Can J Cardiol. 2004;20:1212-18.
- [Google Scholar]




