Translate this page into:
Covid-19 presenting as isolated severe thrombocytopenia in an HIV-lymphoma survivor
Correspondence to ANANT MOHAN
[To cite: Madan M, Shareef I, Raja A, Dwivedi T, Mittal S, Sahoo B, et al. Covid-19 presenting as isolated severe thrombocytopenia in an HIV-lymphoma survivor. Natl Med J India 2022;35:235–6.]
Abstract
Coronavirus disease has myriad manifestations and can present with predominantly extrapulmonary manifestations. We describe a 50-year-old man, a person living with HIV (PLHA), a non-Hodgkin lymphoma survivor, who presented with isolated severe thrombocytopenia. He was found to have immune-mediated thrombocytopenia, and showed excellent response to intravenous immunoglobulins.
INTRODUCTION
Covid-19 has myriad manifestations and poses diagnostic and management challenges across all specialties of modern medicine. Though thrombocytopenia has been studied as a marker of severity, it can be an isolated presenting manifestation too. We report a patient with human immunodeficiency virus (HIV)–Covid coinfection presenting as isolated severe thrombocytopenia in an HIV–lymphoma survivor.
THE CASE
A 50-year-old man, paramilitary worker, was admitted to our centre, after being detected to be Covid-19-positive. He had no constitutional or respiratory symptoms. He was HIV-positive, on treatment since 2004, and had received zidoviudine, lamivudine and efavirenz regimen (ZLE) initially, which had been modified to lamivudine, tenofovir and efavirenz (TLE) in 2015; he had been on atanazavir/ritonavir, lamivudine and tenofovir (TDF+3TC+ATV/r) since 2018; his last recorded CD4 count was 320 in December 2019. He had a past history of Hodgkin lymphoma in 2011, had received chemotherapy, and had been in remission since.
His clinical examination was normal—there was no pallor, cyanosis, lymphadenopathy or hepatosplenomegaly. There were few conjunctival petechiae; an ecchymotic patch (approximately 3 cm×2 cm) was seen on the anterior aspect of the right elbow. Initial investigations were unremarkable, except for thrombocytopenia of 5000/cmm. The patient received 4 units of platelet transfusion which improved the platelet count to 17 000/cmm on day 2; however, it again declined to 7000/cmm the next day. Peripheral smear did not reveal any parasitic infection; and was normal except for decreased platelets. Dengue serology was negative. Prothrombin time, D-dimer (290 ng/ml) and fibrinogen (320 mg/dl) were normal. As he was on tenofovir and lamivudine for the past 2 years, none of the drugs could be incriminated as a cause of thrombocytopenia. CT chest and abdomen, done to rule out disseminated infective aetiology or recurrence of lymphoma, was normal. Bone marrow aspiration and biopsy revealed a normal bone marrow without any evidence of infiltration or myelofibrosis (Fig. 1a). In view of severe thrombocytopenia and bleeding manifestations, and presumptive diagnosis of immune-related thrombocytopenia, intravenous immunoglobulin (IVIG) was administered—1 g/kg of IVIG over 2 days. After 3 days of IVIG, repeat haemogram showed a steadily rising platelet count, which reached 60 000/cmm on day 11 (Fig. 1b). The patient was discharged after day 18 with a negative Covid-19 report.
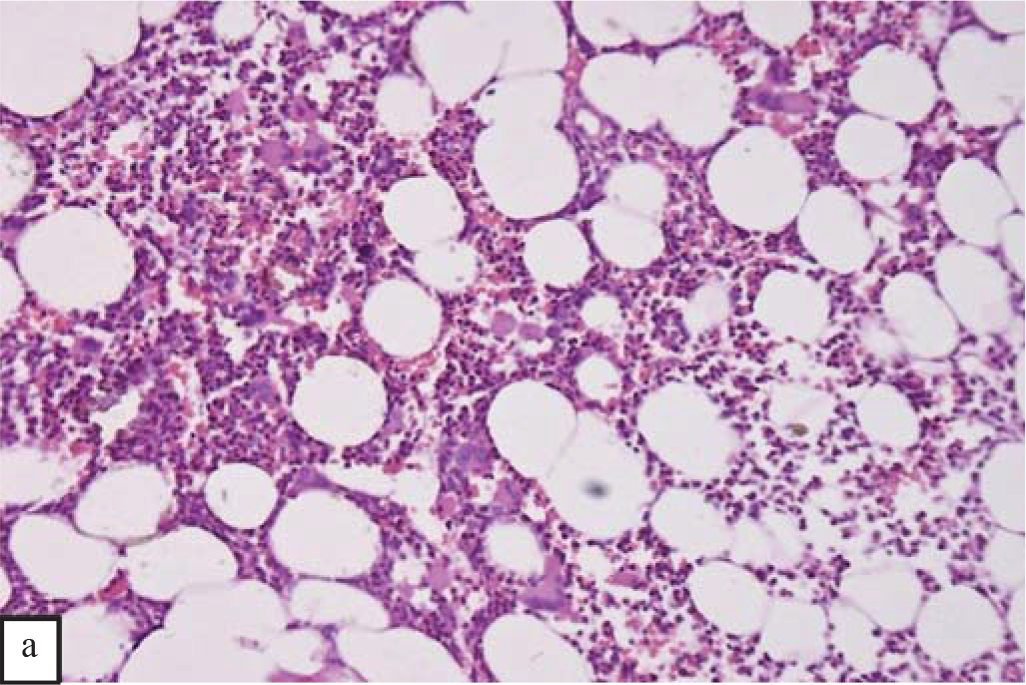
- Photomicrograph of trephine bone marrow biopsy (haematoxylin and eosin stain, 100× magnification) shows haematopoietic cells of all three lineage. No atypical cell was seen
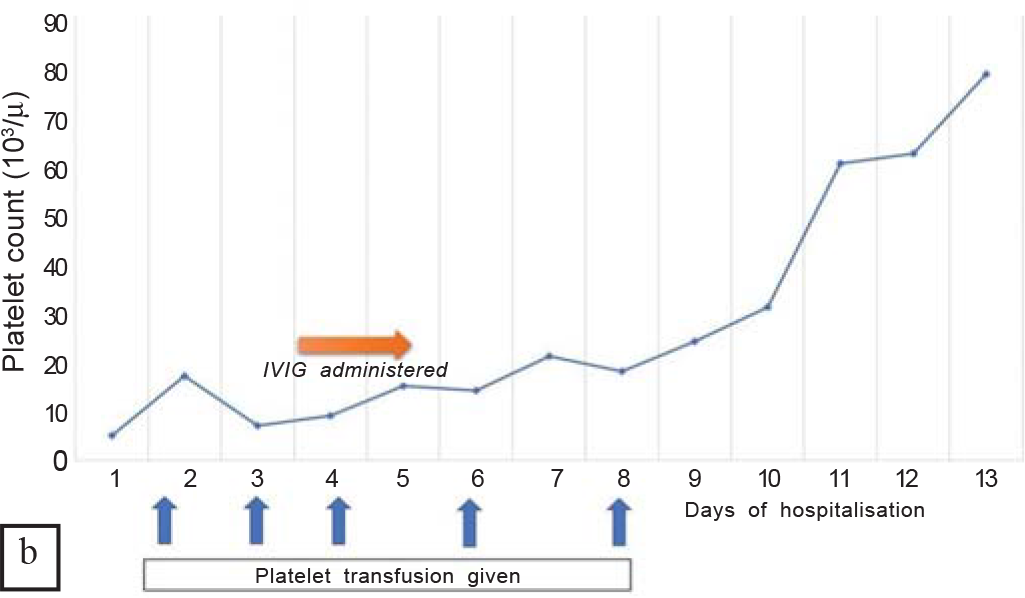
- Graph showing evolution of platelet counts along with interventions such as platelet transfusion and intravenous immunoglobulin (IVIG) therapy
DISCUSSION
We report asymptomatic Covid-19 in an HIV–lymphoma survivor, presenting with severe thrombocytopenia, which is not a common occurrence.1 HIV can be associated with thrombocytopenia due to the primary disease itself, immunological cause (HIV-associated), disseminated infection with bone marrow involvement, drug-related (e.g. zidovudine) or lymphoproliferative disorders. HIV-related immune thrombocytopenia can be a presenting complaint or complication during the course of the disease, though its prevalence has reduced with the advent of highly active antiretroviral therapy (HAART).2 The prevalence of thrombocytopenia in Covid-19 has been reported to range from 7% to 47%, and has been associated with the risk of severe disease and a high risk of mortality.3 The mechanisms of thrombocytopenia in Covid-19 can be due to direct infection of the marrow causing inhibition of platelet synthesis, as a part of the cytokine storm, or generation of platelet-rich micro-thrombi leading to platelet consumption.4 Coinfections such as malaria and dengue, as well as disseminated tubercular or fungal infections may cause thrombocytopenia in immuno-compromised Covid-19 patients. Immune thrombocytopenia precipitated due to Covid-19 has been reported in case reports and case series, with varied presentations and severity and good response to IVIG,5,6 which via their immunomodulatory effect, have been shown to be effective in the treatment of idiopathic as well as HIV-associated immune thrombocytopenia.5,6 Also, IVIG therapy has shown promising though variable results in patients with severe and critical Covid-19 pneumonia, in ongoing trials.7 In view of the above, we preferred IVIG to high-dose corticosteroids in this patient. As the pandemic goes on, we are likely to encounter more patients with HIV– Covid-19 coinfections. Therefore, physicians should be vigilant regarding atypical and extrapulmonary presentations of Covid-19 in this population.
References
- Immune thrombocytopenic purpura in a patient with Covid-19. N Engl J Med. 2020;382:e43.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical features, treatment, and outcome of HIV-associated immune thrombocytopenia in the HAART era. Adv Hematol. 2012;2012:910954.
- [CrossRef] [PubMed] [Google Scholar]
- Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: A meta-analysis. Clin Chim Acta. 2020;506:145-8.
- [CrossRef] [PubMed] [Google Scholar]
- Mechanism of thrombocytopenia in COVID-19 patients. Ann Hematol. 2020;99:1205-8.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19-associated immune thrombocytopenia. Br J Haematol. 2020;190:e61-e64.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19 presenting with immune thrombocytopenia: A case report and review of the literature. J Med Virol. 2021;93:43-5.
- [CrossRef] [PubMed] [Google Scholar]
- High-dose intravenous immunoglobulins in the treatment of severe acute viral pneumonia: The known mechanisms and clinical effects. Front Immunol. 2020;11:1660.
- [CrossRef] [PubMed] [Google Scholar]




