Translate this page into:
Dermatological diseases in the elderly: An observational study at a tertiary care hospital in northern India
Corresponding Author:
Sarita Sanke
Department of Dermatology and Sexually Transmitted Diseases, Lady Hardinge Medical College and Associated hospitals, Shaheed Bhagat Singh Marg, New Delhi
India
sankesarita@gmail.com
| How to cite this article: Mendiratta V, Sanke S, Chander R. Dermatological diseases in the elderly: An observational study at a tertiary care hospital in northern India. Natl Med J India 2019;32:58-59 |
Dermatological diseases in the elderly: An observational study at a tertiary care hospital in northern IndiaDermatological disorders are a common cause of morbidity in the elderly. With an ever increasing population of the elderly it is important to understand the main dermatological problems related to ageing. We did a cross-sectional observational study, approved by our institutional ethics committee, of all patients of either gender, aged 60 years and above, attending the geriatric outpatient department at our tertiary care hospital, between 2014 and 2016. After obtaining consent, a detailed history was followed by examination of the skin, mucosae and nails. Any associated systemic disease was also noted. Data were entered in an Excel sheet and were analysed using descriptive statistics. SPSS software version 18 was used. The data were expressed in frequencies and percentages.
A total of 530 patients aged 60 years and above were analysed. Of these, 320 (60%) were men and 210 (40%) were women. The minimum age was 60 years and the maximum was 90 years. Derma- tological manifestations related to ageing were predominantly senile pruritus, skin tags, freckles, lentigines, cherry angioma, seborrheic keratoses, dermatoses papulosa nigra, wrinkling, senile comedones, senile purpura, xerosis, keratoderma, callosity, sebaceous gland hyperplasia, epidermoid cyst and Favre-Racouchot syndrome and were observed as overlapping dermatoses in 290 (54.7%) patients [Figure - 1]. These were the primary complaints in a few, while others were not bothered by these. Senile pruritus was reported by 140 (26.4%) patients.
 |
| Figure 1: Seborrheic keratoses (red arrow), freckles (blue arrow) and solar elastoses (yellow arrow) in an elderly woman |
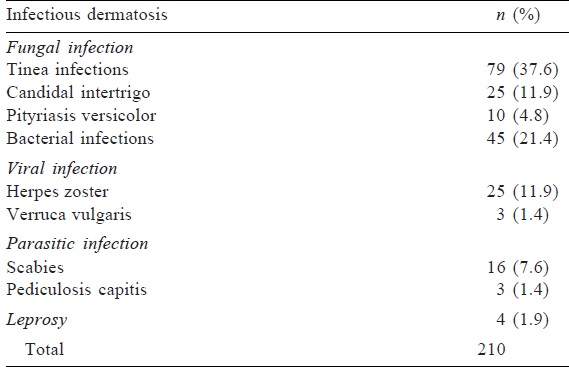
Cutaneous infections constituted the most common dermatological disease in our patients and were present in 210 (39.6%) patients [Table - 1].
Inflammatory dermatoses were observed in 92 (17.3%) patients, of which psoriasis, lichen planus, pigmented purpuric dermatoses and seborrheic dermatitis were common and accounted for 31 (33.7%), 22 (23.9%), 12 (13%) and 15 (16.3%) patients, respectively. The other less common conditions included atopic dermatitis, parapsoriasis, chronic superficial scaly dermatitis and amyloidosis. Thirty- two (6%) patients presented with autoimmune disorders, which included urticaria (40%), discoid lupus erythematosus (34%) and lichen sclerosis et atrophicans (25%), while 1 woman presented with paraneoplastic dermatomyositis.
Eczematous conditions were diagnosed in 65 (12.3%) patients. The commonest presentation was asteatotic eczema in 3 8% patients, followed by nummular eczema (24%), hand eczema ( 14%), pompholyx (4%), lichen simplex chronicus (12%) and lichen simplex chronicus hypertrophies (8%).
Allergic contact dermatitis mostly due to hair dye and mustard oil were diagnosed in 24 (4.5%) patients, and photoallergic contact dermatitis and air-borne contact dermatitis were seen in 8 (1.5%) and 4 (0.75%) patients, respectively. Neuropathic dermatoses which included post-herpetic neuralgia, diabetic and trophic ulcers were observed in 18 (3.4%) patients. In the immunobullous group, 4 had bullous pemphigoid, 2 had pemphigus vulgaris, while 1 had linear IgA disease. Three patients presented with fixed drug eruption, 6 with lichenoid drug eruption (either to antihypertensive or antidiabetic drugs they were on), while 1 with antitubercular therapy-induced erythroderma. Disorders of pigmentation were also observed and included melasma (20), idiopathic guttate hypomelanosis (135), vitiligo (8), toxic melanosis (4) and post-inflammatory hypo-/hyper- pigmentation (40). Malignant conditions such as basal cell carcinoma were seen in only 2 patients, and squamous cell carcinoma in 1 patient.
Ageing is a complex process that has been defined as the accumulation of molecular damage over time. Two types of skin ageing exist: intrinsic ageing, which includes changes due to normal maturity, and extrinsic ageing, which is due to extrinsic factors such as ultraviolet exposure.
Men outnumbered women in our study with a men:women ratio of 1.5:1; similar to other studies.[1]·[2] The oldest patient was aged 90 years. Majority of our patients (57.4%) suffered from age-related changes. Skin tags were seen in 30.1% (160). The frequency of senile comedones in various studies ranged from 11.5% to 95.6%.[3],[4] In our study, it was observed in 22.6% ( 120). Twenty-six per cent of patients (140) complained of pruritus, whereas other studies reported an incidence from 9% to as high as 74.6%.[5],[6],[7],[8]
Cutaneous infections and infestations (39.6%) were common in our series. Fungal infection was the commonest followed by bacterial infections, which was similar to other studies.[2]·[9] The high frequency of infections in our study could be attributed to high temperatures in Delhi, leading to excessive sweating and overcrowding promoting cross-infection in the family.
Pigmentary dermatoses constituted the third most common group of dermatoses in the the elderly. Idiopathic guttate hypomelanosis is a common, benign pigmentary disorder related to ageing which mimics vitiligo that compels the patient to seek consultation. It was seen in 25.4% in our study, which is similar to other studies.[3],[10] However, Raveendra reported a higher frequency of 33% in his study.[2] The incidence of psoriasis in our study was 5.8%, while in various other studies, it ranged from 1% to 11%.[3],[11],[12],[13] Nearly 12% of patients presented with eczematous disorders, the commonest being asteatotic eczema. This incidence is slightly low as compared to other studies where it ranged from 11.9% to 58%.[2],[7],[9] Immunological disorders were seen in 8% of our patients. The incidence in other studies ranged from 0.5% to 4.1%.[1],[14],[15] The incidence of allergic dermatitis in our patients was 6.8%. This was mostly seen in the group using hair dye and mustard oil. Other studies reported an incidence ranging from as low as 1.5% to as high as 58.7%.[5],[16],[17] This variation may be on account of regional, cultural, environmental and occupational differences.
In various studies, the incidence of bullous disorders ranges from 0.5% to 4.4%, while in our study, it was 1.3% with bullous pemphigoid being the commonest presentation.[1],[2],[7],[10] Trophic ulcer was seen in 8 (4%) cases in a study done by Raveendra.[2] A large number of geriatric patients are on a number of drugs for their comorbid conditions and hence are at higher risk for developing drug-induced dermatoses. The incidence of drug-induced dermatoses in our study was 1.8%.
Diabetes was the most common comorbid condition with an incidence of 49%. Its incidence in several other studies ranged from 9% to 32.5%.[3],[11],[18] However, Nair and Vora reported the most common comorbid condition to be hypertension in 70.9% of their patients.[18]
Associated comorbid conditions such as hypertension and diabetes predispose the elderly to several dermatological diseases and we suggest that multispecialty, one-stop clinics are required for the elderly to minimize inconvenience and for expediting the management of multiple problems including those related to the skin.
Conflicts of interest. None declared
| 1. | Yalçin B, Tamer E, Toy GG, Oztaş P, Hayran M, Alli N, et al. The prevalence of skin diseases in the elderly: Analysis of 4099 geriatric patients. Int J Dermatol 2006;45:672-6. [Google Scholar] |
| 2. | Raveendra L. A clinical study of geriatric dermatoses. Our Dermatol Online 2014;5:235-39. [Google Scholar] |
| 3. | Patange VS, Fernandez RJ. A study of geriatric dermatoses. Indian J Dermatol Venereol Leprol 1995;61:206-8. [Google Scholar] |
| 4. | Beauregard S, Gilchrest BA. A survey of skin problems and skin care regimens in the elderly. Arch Dermatol 1987;123:1638-43. [Google Scholar] |
| 5. | Jindal R, Jain A, Roy S, Rawat SD, Bhardwaj N. Skin disorders among geriatric population at a tertiary care center in Uttarakhand. J Clin Diagn Res 2016;10: WC06-8. [Google Scholar] |
| 6. | Darjani A, Mohtasham-Amiri Z, Mohammad Amini K, Golchai J, Sadre-Eshkevari S, Alizade N, et al. Skin disorders among elder patients in a referral center in Northern Iran (2011). Dermatol Res Pract 2013;2013:193205. [Google Scholar] |
| 7. | Liao YH, Chen KH, Tseng MP, Sun CC. Pattern of skin diseases in a geriatric patient group in Taiwan: A 7-year survey from the outpatient clinic of a university medical center. Dermatology 2001;203:308-13. [Google Scholar] |
| 8. | George RR, Joy B, Balakrishnan AN. Clinico-epidemiological study geriatric dermatosesin a tertiary care hospital in Kerala. Int J Recent Trends Sci Technol 2016;18:498-502. [Google Scholar] |
| 9. | Souissi A, Zeglaoui F, El Fekih N, Fazaa B, Zouari B, Kamoun MR, et al. Skin diseases in the elderly: A multicentre Tunisian study. Ann Dermatol Venereol 2006; 133:231-4. [Google Scholar] |
| 10. | Durai PC, Thappa DM, Kumari R, Malathi M.Aging in elderly: Chronological versus photoaging. Indian J Dermatol 2012;57:343-52. [Google Scholar] |
| 11. | 1Sahoo A, Singh PC, Pattnaik S, Panigrahi RK. Geriatric dermatoses in Southern Orissa. Indian J Dermatol 2000;45:66-8. [Google Scholar] |
| 12. | Tindall JP, Smith JG Jr. Skin lesions of the aged and their association with internal changes. JAMA 1963;186:1039-42. [Google Scholar] |
| 13. | Weismann K, Krakauer R, Wanscher B. Prevalence of skin diseases in old age. Acta Derm Venereol 1980;60:352-3. [Google Scholar] |
| 14. | Grover S, Narasimhalu CR. A clinical study of skin changes in geriatric population. Indian J Dermatol Venereol Leprol 2009;75:305-6. [Google Scholar] |
| 15. | Sheethal MP, Shashikumar BM. A cross-sectional study on the dermatological conditions among the elderly population in Mandya city. Int J Med Sci Public Health 2015;4:467-70. [Google Scholar] |
| 16. | Bilgili SG, Karadag AS, Ozkol HU, Calka O, Akdeniz N. The prevalence of skin diseases among the geriatric patients in Eastern Turkey. J Pak Med Assoc 2012;62: 535-9. [Google Scholar] |
| 17. | Cvitanoviæ H, Knezeviæ E, Kuljanac I, Janciæ E. Skin disease in a geriatric patients group in outpatient dermatologic clinic Karlovac, Croatia. Coll Antropol 2010;34 Suppl 2:247-51. [Google Scholar] |
| 18. | Nair PA, Vora R. Association of systemic diseases with cutaneous dermatosis in elderly population: Preliminary observation at a rural tertiary care centre. J Family Med Prim Care 2015;4:74-8. [Google Scholar] |
Fulltext Views
2,568
PDF downloads
1,739




