Translate this page into:
Development and use of low-fidelity, low-cost, animal tissue-based simulators for surgical training during the Covid-19 pandemic
Correspondence to VUTHALURU SEENU; varnaseenu@hotmail.com
[To cite: Joshi MK, Bhattacharjee HK, Suhani, Roy A, Seenu V. Development and use of low-fidelity, low-cost, animal tissue-based simulators for surgical training during the Covid-19 pandemic. Natl Med J India 2022;35:239–42.]
Abstract
Background
The Covid-19 pandemic severely affected surgical training as the number of surgeries being done was reduced to a bare minimum. Teaching and training of clinical skills on a simulator are desirable as they may have an even larger role during the Covid-19 pandemic. Commercially available simulators with optimum fidelity are costly and may be difficult to sustain because of their recurring cost. The development of low-cost simulators with optimum fidelity is the need of the hour.
Methods
We developed animal tissue-based simulators for imparting skills training to surgical residents on some basic and advanced general surgical procedures. Porcine tissue and locally available materials were used to prepare these models. The models were pilot-tested. Standard operating procedures were developed for each skill that was shared with the participants well before the ‘hands-on’ exercise. An online pre-test was conducted. The training was then imparted on these models under faculty guidance adhering to Covid-19-appropriate behaviour. This was followed by a post-test and participant feedback. The entire exercise was paperless.
Results
Sixty residents were trained in 10 sessions. Most of the participants were men (44; 73%). The mean pre-test and post-test scores were 40.92 (standard deviation [SD] 6.27) and 42.67, respectively (SD 4.06). Paired sample t-test suggested a significant improvement in the post-test score (p<0.001). The activity and the models were well appreciated by the residents.
Conclusion
The animal tissue-based indigenous models are easy to prepare, cost-effective and provide optimum fidelity for skill training of surgical residents. In addition to skill acquisition, training on such modules may alleviate the stress and anxiety of the residents associated with the loss of surgical training during a time-bound residency period.
INTRODUCTION
The Covid-19 pandemic affected patient care, education and research activities all over the world.1–4 As elective surgeries were largely on-hold, opportunities for skill acquisition of surgical residents were hampered.5–7 The All India Institute of Medical Sciences (AIIMS), New Delhi is a tertiary care teaching hospital where over 6000 major and 40 000 minor surgeries are performed annually, and about 30 general surgical residents are admitted every year to the Department of Surgical Disciplines for training. The initial surgical training of the residents is primarily ‘hands-on’, the residents learn by observing and assisting, thereafter they perform surgery under different levels of supervision, and then independently. Following the Covid-19 outbreak, the number of elective general surgeries plummeted as human and material resources were diverted towards the care of patients with Covid-19. Taking cognizance of this training deficit, we embarked on a simulation-based training for the residents. Procuring good quality, high-fidelity simulators in a short time was difficult because of their prohibitive cost and non-availability during the pandemic. This prompted us to look for alternatives, and we developed some indigenous low-cost simulators. These included low-fidelity, animal tissue-based simulators for incision and drainage (I&D) of superficial abscess, excision of subcutaneous lump, closure of laparotomy wound, use of electrosurgical devices, dissection in correct surgical planes and resection and anastomosis (RA) of the intestine using staplers.
METHODS
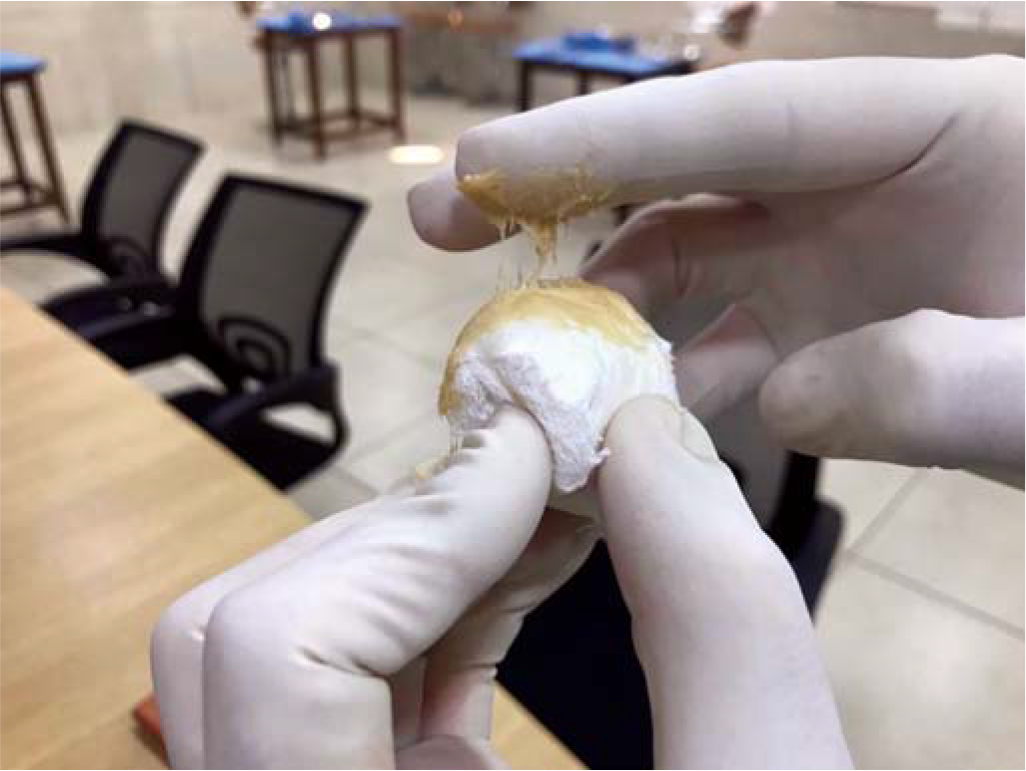
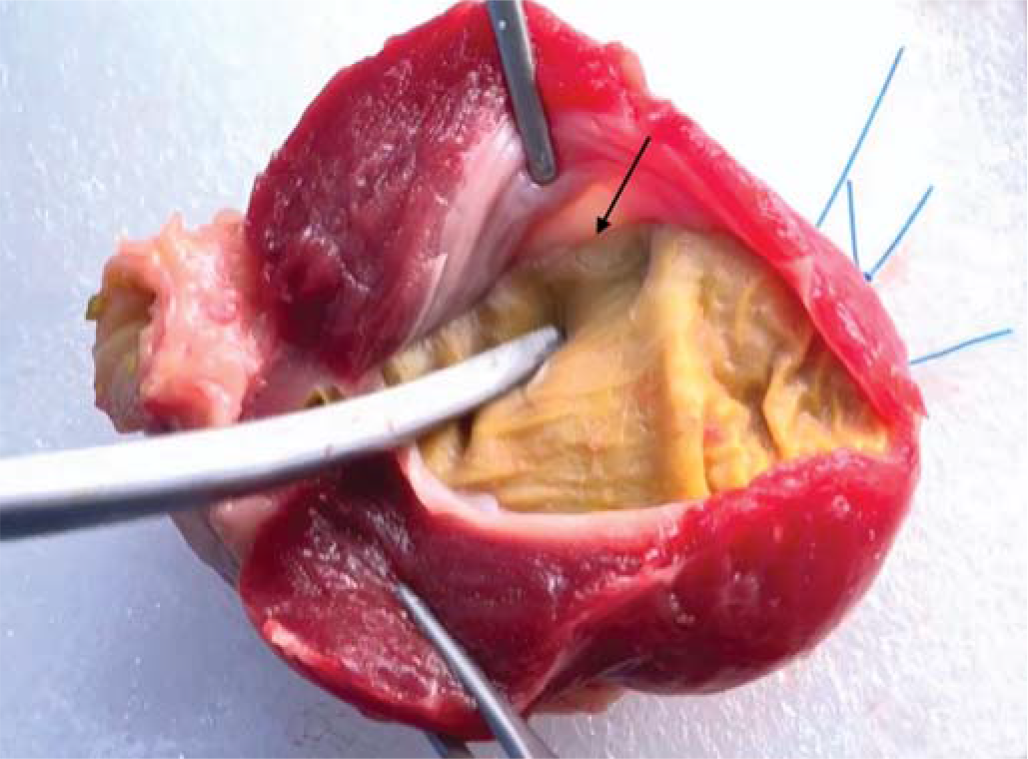
Fresh animal tissues were procured from a designated vendor at an abattoir who supplies animal parts for training and research to our institute. Pork belly (abdominal wall) measuring 15 cm×15 cm was used for simulation for I&D and excision of superficial lump. A cut finger of surgical glove was filled with egg yolk to simulate an abscess (Fig. 1). A 3 cm×3 cm ball of surgical bandage coated with adhesive paste to mimic fibrinous and fibrous adhesions was used to simulate a lump (Fig. 2). These were inserted in the subcutaneous plane of the pork belly using a small incision at one of the margins of the mannequin (Fig. 3). Porcine abdominal wall, stomach and intestine were used for imparting skills on closure of the laparotomy wound, RA using staplers and use of electrosurgical devices, respectively. Chicken gizzard and swine oesophagus were used for teaching dissection in correct surgical planes. The total cost of the models used for training each resident was about ₹750.

- Cut finger of surgical glove filled with egg yolk to simulate abscess
- Ball made of surgical bandage to simulate lump coated with adhesive paste to mimic fibrinous and fibrous adhesions

- Simulated lump and abscess placed in subcutaneous plane of the pork belly (dotted circle); incision at the margin (arrow)
The models were initially tested and validated by four faculty members. Suggestions were incorporated to make the models more realistic. The use of thick paste to simulate fibrinous adhesion for the model of ‘excision of superficial lump’ and use of a cut finger of the glove instead of balloon for the model of ‘I&D’ were found rewarding. Once found appropriate, standard operating procedures (SOPs) for each module were drafted, which were peer-reviewed. The SOP including the videos on the procedures was shared online with the participants 2 days before the planned activity to familiarize them with the models. The workshops were conducted at the wet laboratory of the Skill facility following norms of personal protection and adequate physical distancing. All participants and trainers wore appropriate personal protective equipment (PPE) and the models were sanitized using 70% alcohol.
A pre-test was conducted to assess the baseline knowledge of the participants. The trainer to trainee ratio was 1:2.
The participants were asked to perform I&D and excision of lump as per the SOP. For dissection in correct surgical planes, the lumen of the swine oesophagus was filled with water and clamped at both ends, the participants were then asked to dissect in the plane between the mucosa and the muscles without damaging the mucosa (Fig. 4). The leakage of fluid signified the failure of the procedure. Similarly, the participants were asked to dissect the plane between the outer tough layer and the mucosa of the chicken gizzard (Fig. 5). They were allowed sufficient time to practise on the models till they were confident of their skills. This was followed by post-test and a formal feedback from the participants on a pre-designed questionnaire. The questionnaire comprised 5 closed-ended questions to be responded on Likert scale and 4 open-ended ones (Table I). The whole exercise including the pre-test, post-test and feedback was kept paperless to avoid potential fomite-mediated transmission. The difference between pre-test and post-test scores was analysed using paired sample t-test. After use, the animal tissues were disposed of as per the standard protocol laid down by the institute’s biomedical waste management facility. The parts were transported in impervious yellow bags meant to dispose of infected waste and human tissues, and were incinerated.

- Plane of dissection between mucosa and muscles of porcine oesophagus (arrow)
- Plane of dissection between outer tough layer and mucosa of the chicken gizzard (arrow)
| Questionnaire |
|---|
| The content was related to our needs as general surgery postgraduate residents. |
| The modules were easy to understand and learn from. |
| The operative steps in the modules were explained well. |
| The skills could be learned easily in the wet laboratory after reading the educational material that was provided. |
| Practising all modules on a single day enabled learning at a comfortable pace. |
| What did you like most about the course? |
| What did you like least about the course? |
| What other skills would you like to learn in a similar manner? |
| What suggestions would you like to give to improve the course? |
Please mark an option for each component of the feedback on a scale of 1 (strongly disagree) to 5 (strongly agree); feel free to comment.
RESULTS
Sixty residents working in the department of surgery were trained in 10 sessions. The majority of them (44; 73%) were men. The training on the modules could be achieved as per the plan, including the delivery of the content, hands-on activity, corrections and reinforcement by the mentors for all the participants in time. The mean (SD) pre-test score and post-test scores were 40.92 (6.27) and 42.67 (4.06), respectively. The value of paired sample t-test statistic was 2.59, which was more than the critical threshold value of 1.96, thereby rejecting the null hypothesis and suggesting that the difference between the preand post-test scores was statistically significant (p<0.001). The feedback of the participants was encouraging (Table II). All participants agreed that the modules met the needs of postgraduate residents of surgery. Most of them found the content of the modules informative (91.6%) and that the operative steps were explained well (96.7%). Three participants (5%) reported that there was some difficulty in performing the skills even after going through the supplemented educational material, while 7 (11.7%) had a neutral response. Ten participants (16.7%) expressed some concern over the time provided to practise the skills at a comfortable pace.
| Questionnaire item | Strongly disagree | Disagree, n(%) | Can’t say, n(%) | Agree, n(%) | Strongly agree, n(%) |
|---|---|---|---|---|---|
| The content was related to our needs as general surgery postgraduate residents. | 0 | 0(1.7) | 0(1.7) | 8 (13.3) | 52 (86.7) |
| The modules were easy to understand and learn from. | 0 | 1 (1.7) | 4 (6.7) | 5 (8.3) | 50 (83.3) |
| The operative steps in the modules were explained well. | 0 | 0(1.7) | 2 (3.3) | 10 (16.7) | 48 (80) |
| The skills could be learned easily in the wet laboratory after reading the educational material that was provided. | 0 | 3 (5) | 7 (11.7) | 5 (8.3) | 45 (75) |
| Practising all modules on a single day enabled learning at a comfortable pace. | 0 | 5 (8.3) | 5 (8.3) | 30 (50) | 20 (33.4) |
Regarding the response to the open-ended questions, there were suggestions to increase the duration of the course and inclusion of more surgical skills by some participants. Residents liked the ‘feel’ of the tissues and commented that it matched with that of human tissues. Learning under supervision and personal mentoring were appreciated.
DISCUSSION
The importance of simulation-based training for surgical trainees cannot be overemphasized. It has been considered indispensable by various academic bodies, including the erstwhile Medical Council of India.8 In addition to imparting adequate surgical expertise and improving the competence of the trainee, the perceived advantages of simulation-based skill training include circumvention of ethical and legal concerns, improved skill acquisition and patient safety. The traditional training of residents in surgical specialties has been by observation, assistance, practising under supervision, and then performing independently. With an increasing number of trainees and decreased opportunities for skill acquisition, there have been apprehensions regarding adequate training of residents.9
The Covid-19 pandemic has hampered the training of surgical residents all over the world, and with the material and resource constraints, imparting adequate skill training has been an area of active debate.5–7 The residents’ training was affected as elective surgeries were either suspended or reduced to a minimum, adding to their frustration due to lack of surgical work. Training on simulators may be a way out in this situation that not only allows the trainees to acquire and hone their surgical skills but also helps alleviate the stress and anxiety of loss of surgical training during the time-bound residency period.
The use of high-fidelity simulators may not be practical, especially for resource-limited settings, due to their prohibitive initial and maintenance cost. The use of innovative, low-cost yet effective training modules is therefore the need of the hour.10 Animal tissue-based training modules are considered better than the inanimate basic simulators as the consistency and handling of the tissues matches closely with live human tissues.11 Various authors have developed and used such modules.12,13
Our modules were easy to prepare and mimicked the actual surgical experience rather closely. The initial peer-review process helped us in improving the content and working with animal tissues. Other faculty members also perceived the initiative to be valuable. The sharing of the content before the actual practice on models allowed us to spare less time in discussing the theoretical component and we could spend more time for the ‘hands-on’ activity. The low trainer-to-trainee ratio helped in better supervision. All Covid-appropriate behaviours were strictly followed, including wearing of PPE, adequate physical distancing and sanitization of models using 70% alcohol. In addition, no paper was used in the entire exercise to prevent any fomite-based transmission.
The improvement in the post-test score validated the efficacy of the exercise. Although the models used did not have a superior fidelity, yet they were found effective in achieving the purpose of training as per our experience and the trainees’ feedback. Low-fidelity of such models should not be considered as a deterrent and, at times, it is advantageous.14 Low-fidelity simulators are known to provide high-fidelity simulation.15,16 Fidelity of these models can be improved further by providing a suitable clinical environment with the active involvement of the teacher to engage the learners for better immersion.
Conclusion
The use of indigenously developed low-fidelity, low-cost, animal tissue-based simulation for surgical training during the current pandemic is feasible. It not only serves to impart and improve the necessary surgical skills but also helps in averting boredom of the residents due to relative lack of surgical work.
Conflicts of interest
None declared
References
- Mitigating the risks of surgery during the COVID-19 pandemic. Lancet. 2020;396:2-3.
- [CrossRef] [PubMed] [Google Scholar]
- The untold toll--The pandemic's effects on patients without COVID-19. N Engl J Med. 2020;382:2368-71.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of the COVID-19 pandemic response on other health research. Bull World Health Organ. 2020;98:625-31.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of the COVID-19 pandemic on core surgical training. Scott Med J. 2020;65:133-7.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of coronavirus 2019 (COVID-19) on training and well-being in subspecialty surgery: A national survey of cardiothoracic trainees in the United Kingdom. J Thorac Cardiovasc Surg. 2020;160:980-7.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of COVID-19 on surgical training across the United States: A national survey of general surgery residents. J Surg Educ. 2021;78:431-9.
- [CrossRef] [PubMed] [Google Scholar]
- Competency Based Under Graduate Curriculum. 2019. Available at www.mciindia.org/CMS?information-desk/for-colleges/ug-curriculum (accessed on 14 Apr 2021)
- [Google Scholar]
- Challenges and issues in medical education in India. Acad Med. 2006;81:1076-80.
- [CrossRef] [PubMed] [Google Scholar]
- Cost-efficient medical education: An innovative approach to creating educational products. J Grad Med Educ. 2019;11:713-16.
- [CrossRef] [PubMed] [Google Scholar]
- Development and validation of a novel and cost-effective animal tissue model for training transurethral resection of the prostate. J Surg Educ. 2017;74:898-905.
- [CrossRef] [PubMed] [Google Scholar]
- Development and evaluation of a novel simulation model for transabdominal preperitoneal (TAPP) inguinal hernia repair. Hernia. 2020;24:159-66.
- [CrossRef] [PubMed] [Google Scholar]
- High-fidelity is not superior to low-fidelity simulation but leads to overconfidence in medical students. BMC Med Educ. 2019;19:29.
- [CrossRef] [PubMed] [Google Scholar]
- Low fidelity simulation in a high fidelity world. Postgrad Med J. 2019;95:687-8.
- [CrossRef] [Google Scholar]
- Low fidelity simulations with high impact results. Clin Simul Nurs. 2009;5:s7.
- [CrossRef] [Google Scholar]




