Translate this page into:
Dry ice in the eye: A rare occupational hazard!
Corresponding Author:
Namrata Sharma
Dr Rajendra Prasad Centre for Ophthalmic Sciences, All India Institute of Medical Sciences, New Delhi 110029
India
namrata.sharma@gmail.com
| How to cite this article: Agarwal R, Urkude J, Shaikh NF, Banerjee M, Sharma N. Dry ice in the eye: A rare occupational hazard!. Natl Med J India 2020;33:281-283 |
Abstract
Superficial corneal foreign bodies (FBs) are a common occupational ocular hazard and can cause visually important astigmatism. A 23-year-old male working in a factory, which produced dry ice (solid carbon dioxide), presented to our emergency unit with symptoms of whitish discolouration of the right cornea for 1 day. Visual acuity in both eyes was 20/20 and slit-lamp examination of the right eye revealed an irregularly shaped whitish superficial FB in the inferior paracentral cornea with surrounding superior nebular opacity. Its gentle removal with a moistened cotton bud revealed an underlying epithelial defect with residual whitish changes. At 1-month of follow-up, the patient had nebulo-macular corneal opacity with stromal thinning at the site of impacted dry ice. We speculate that dry ice causes corneal damage due to its extremely cold temperatures and the formation of carbonic acid.Introduction
Corneal foreign bodies (CFBs) are common causes for a visit to an ophthalmic emergency care set up and occupational injuries contribute to the vast majority of these cases.[1],[2] Various organic and inorganic CFBs related to occupational trauma have been reported in the literature.[1],[2] We report a new mechanism of superficial CFB occurring due to accidental impact of dry ice in the eye.
The Case
A 23-year-old healthy male presented to our emergency unit with a history of whitish discolouration and mild foreign body (FB) sensation of the right eye for the past 2 days. The patient worked in a factory producing dry ice, solid carbon dioxide (CO2), without the use of protective eyewear. Snellen visual acuity was 20/20. The slit-lamp biomicroscopic examination revealed a white-coloured, irregular in shape, superficial CFB in the inferior paracentral area at the level of Bowman’s membrane and superficial stroma with a surrounding rim of nebular corneal opacity in its superior part [Figure - 1]a. The presence of a similar nebular opacity in the superior paracentral area of the cornea was suggestive of an unrecognized previous similar episode [Figure - 1]b. The rest of the examination was uneventful. Anterior segment optical coherence tomography was not done. Microbial keratitis was ruled out by lack of redness, pain, photophobia, surrounding inflammation, anterior chamber reaction and negative corneal scraping specimens. Drug deposits and small corneal keloids which may also present as a white elevated mass on the cornea were ruled out as the former is associated with the use of long-term topical medications, and the latter is longstanding in nature and usually associated with previous corneal lesions. A clinical diagnosis of superficial CFB, dry ice, was made and it was removed on slit lamp with a moistened cotton bud in the same sitting. Residual material found at the base and whitish ring of irreversible changes surrounding the FB in its superior part was left undisturbed. On staining with fluorescein dye immediately following its removal, an epithelial defect corroborating with the size and margins of FB was noticed thereby ruling out other causes of whitish corneal deposits including dust particles, filaments and mucous plaque [Figure - 2]a and [Figure - 2]b. The presence of CO2 in the FB was confirmed by the limewater test (limewater turns milky/cloudy confirming reaction of CO2 with calcium hydroxide present in limewater).
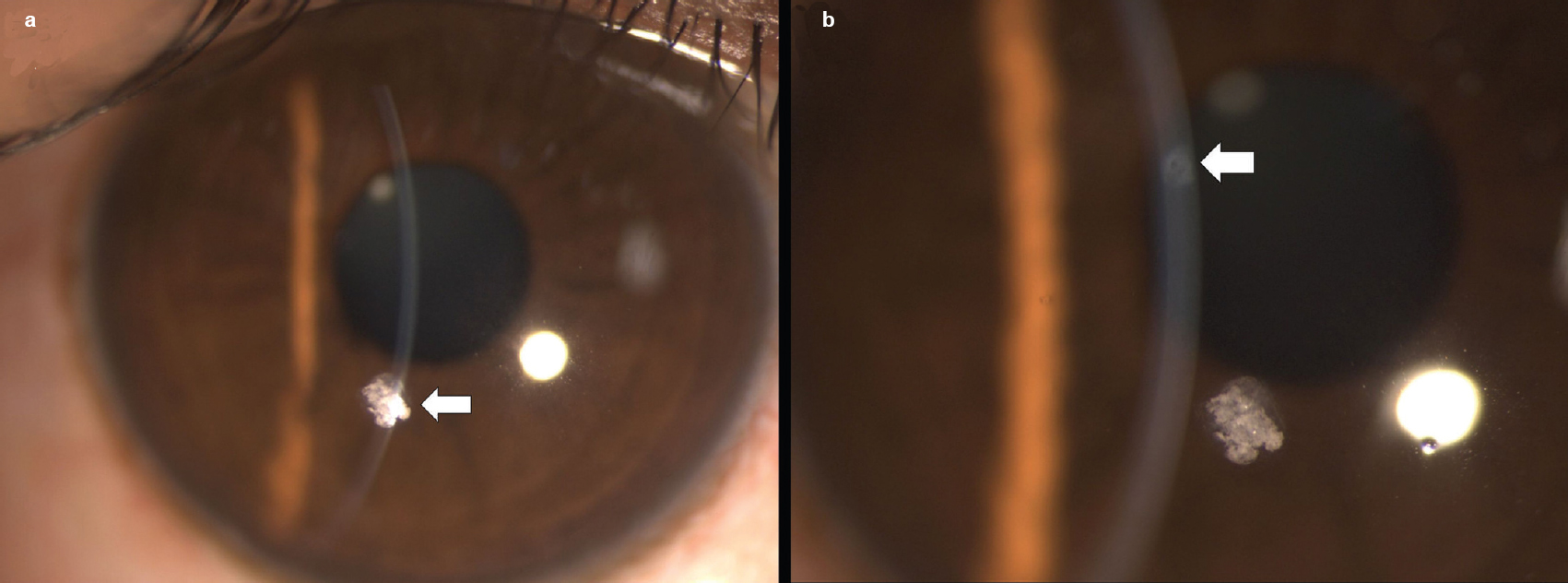 |
| Figure 1: (a) Arrow shows superficial white-coloured corneal foreign body; (b) arrow shows nebulo-macular corneal opacity |
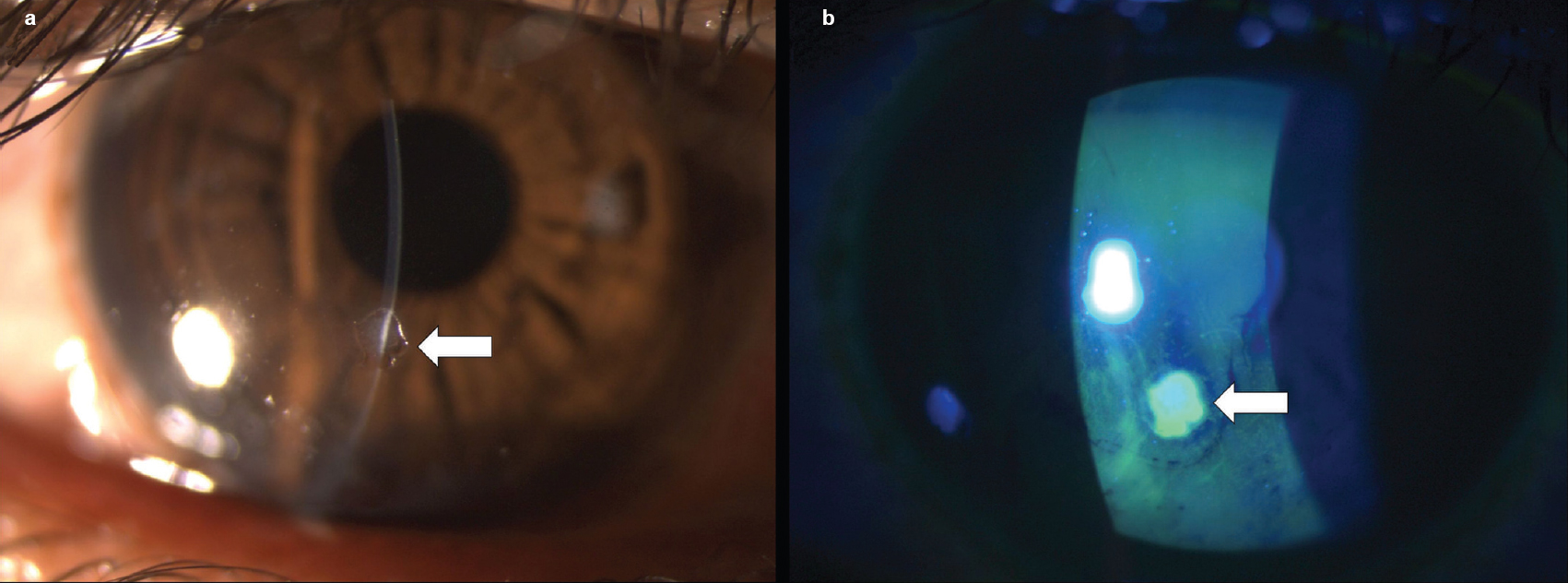 |
| Figure 2: (a) Arrow shows epithelial defect seen immediately after the removal of foreign body; (b) arrow shows epithelial defect corroborating with size and shape of foreign body as seen on cobalt blue light examination after fluorescein staining |
The patient was advised topical prophylactic fourth-generation fluoroquinolone and preservative-free lubricants for a week. At 1-month follow-up, a nebulo-macular corneal opacity associated with stromal thinning at the site of FB not affecting the quality of vision was present [Figure - 3].
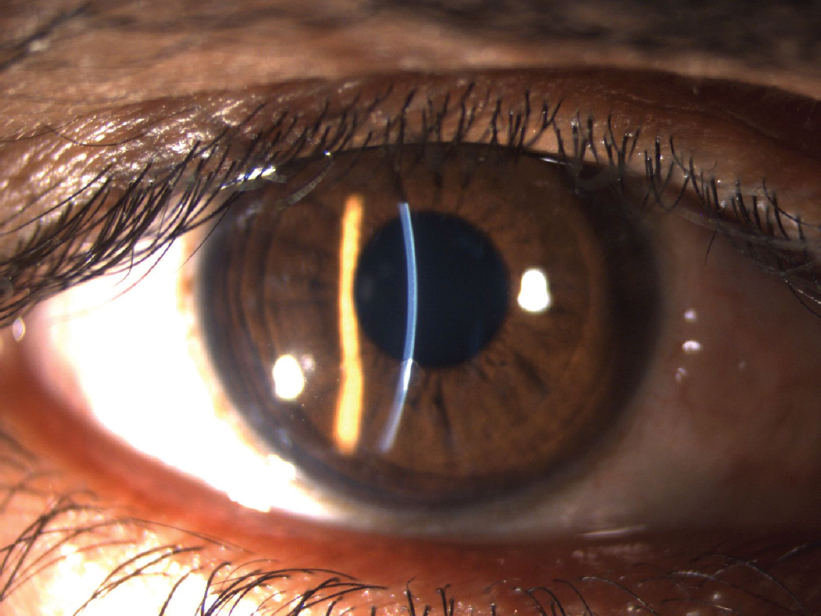 |
| Figure 3: Superficial corneal opacity and stromal thinning seen at the site of foreign body at 1-month follow-up |
Discussion
Superficial corneal FBs are a frequently encountered type of preventable ocular trauma seen in ophthalmic emergency care.[1] Most of these FBs occur in young males and result from occupational trauma with metal-on-metal injury.[2] As most of these cause only minor symptoms and are not associated with ocular morbidity, they are generally ignored.
Dry ice is primarily used as a refrigerant in various industries.[3] The product is stable under normal conditions, but on explosion, it can become dangerous to life and irritative to the eye because of its extremely cold temperature and sublimation into gaseous CO2.[4],[5] Solid CO2 presenting as superficial CFB, to the best of our knowledge, has not been reported.
Solid CO2 probes are used worldwide in cryosurgery for sealing retinal breaks, cataract extraction, multiple adnexal, conjunctival and corneal lesions.[6] The mechanism of cellular destruction by cryotherapy include cellular ischaemia through vascular stasis and tissue necrosis from extracellular ice crystal formation, an effect seen due to supercooling of water.[7] Studies on human donor cornea have speculated susceptibility of endothelial cells and Descemet’s membrane to transcorneal application of cryoprobe related to number of freeze–thaw cycles.[8] The application of such extremely cold temperature on the surface of eye increases the risk of long-term scarring, infection or globe perforation. Although recorded with liquid nitrogen, these effects may be related to extremely cold temperature and not to the nature of the cryogen. Furthermore, gaseous CO2 generated on sublimation of dry ice can chemically react with water to form carbonic acid and may cause acidic trauma to surrounding ocular structures.
In our patient, the dry ice may have settled as a solid structure on the superficial cornea because its accidental impact with cornea was not enough to cause its sublimation into gaseous form. The irreversible changes at and beyond margins of FB as already described may be due to a combination of ischaemic damage from its extremely low temperatures and localized acidic trauma by carbonic acid formed on reaction of gaseous CO2 with water present in tears.
We speculate that the supercooling effect of dry ice may have affected the underlying corneal nerves leading to minimal symptoms in our patient. The FB was removed despite minimal symptoms because our patient was worried about the cosmetic appearance, short-term effects of dry ice were harmful in our patient and the long-term effects were not known. Overzealous attempts at removal of underlying changes were not made to prevent resultant visually important astigmatism.
Conclusion
Our patient highlights the localized hazardous effects of dry ice to the cornea, which necessitates prevention of similar injuries in high-risk workspaces by improving workplace standards, appropriate training of supervisors and conducting awareness programmes on effective eye protection.
Conflicts of interest. None declared
| 1. | Ahmed F, House RJ, Feldman BH. Corneal abrasions and corneal foreign bodies. Prim Care 2015;42:363–75. [Google Scholar] |
| 2. | Nalgirkar AR. Study of ocular foreign bodies in the city population. Indian J Occup Environ Med 2003;7:40–2. [Google Scholar] |
| 3. | Encylopedia Britanica; June 2011. [Google Scholar] |
| 4. | Hsieh CC, Shih CL, Fang CC, Chen WJ, Lee CC. Carbon dioxide asphyxiation caused by special-effect dry ice in an election campaign. Am J Emerg Med 2005;23:567–8. [Google Scholar] |
| 5. | Centers for Disease Control and Prevention (CDC). Acute illness from dry ice exposure during hurricane Ivan – Alabama, 2004. MMWR Morb Mortal Wkly Rep 2004;53:1182–3. [Google Scholar] |
| 6. | Tehrani S, Fraunfelder FW. Cryotherapy in Ophthalmology. Open J Ophthalmol 2013;3:103–17. [Google Scholar] |
| 7. | Fraunfelder FW. Liquid nitrogen cryotherapy for surface eye disease (an AOS thesis). Trans Am Ophthalmol Soc 2008;106:301–24. [Google Scholar] |
| 8. | Oh JY, Lee HJ, Khwarg SI, Wee WR. Corneal cell viability and structure after transcorneal freezing-thawing in the human cornea. Clin Ophthalmol 2010;4:477–80. [Google Scholar] |
Fulltext Views
5,139
PDF downloads
2,034




