Translate this page into:
Early clinical exposure through a vertical integration programme in physiology
2 Department of Paediatric Nephrology, St John’s Medical College, John Nagar, Bengaluru 560034, Karnataka, India
3 Department of Gastroenterology, St John’s Medical College, John Nagar, Bengaluru 560034, Karnataka, India
4 Department of Neurology, St John’s Medical College, John Nagar, Bengaluru 560034, Karnataka, India
5 Department of Anaesthesiology and Critical care, St John’s Medical College, John Nagar, Bengaluru 560034, Karnataka, India
6 Department of Internal Medicine, St John’s Medical College, John Nagar, Bengaluru 560034, Karnataka, India
7 Division of Epidemiology and Biostatistics, St John’s Medical College, John Nagar, Bengaluru 560034, Karnataka, India
Corresponding Author:
D Savitha
Department of Physiology, St John’s Medical College, John Nagar, Bengaluru 560034, Karnataka
India
haisavitha@yahoo.com
| How to cite this article: Savitha D, Iyengar A, Devarbhavi H, Mathew T, K, Rao S, Thomas T, Kurpad AV. Early clinical exposure through a vertical integration programme in physiology. Natl Med J India 2018;31:296-300 |
Abstract
Background. Early clinical exposure is likely to be beneficial during the preclinical year. This pilot programme aimed to define a learning framework of introducing first year medical students to early clinical exposure through a vertical integration programme in the physiology course. The intent was to enhance the understanding of theoretical concepts and practical applications of physiology. Student and faculty perceptions were evaluated.Methods. First year MBBS students (n = 60) had bedside clinics conducted by 5 clinical departments, where the clinical context and applied physiological concepts were emphasized. Clinical sessions were synchronized with pedagogic highlights on related physiological concepts. The student’s perceptions were recorded through a semi-structured questionnaire, while qualitative feedback was obtained from the faculty.
Results. All students ( 100%) reported that the programme was relevant and did not interfere with their physiology course. Most (91%) appreciated the synchronization of classroom knowledge with clinical exposures, and thought that integrated teaching helped in better understanding of practical applications of physiology (94%) with adequate discussions during the sessions (91 %). Fifty-nine (98%) students preferred integrated teaching over the isolated traditional classroom teaching. The clinicians involved also felt that the early clinical exposure was relevant. The students achieved a mean (SD) score of 13 (2.98) of 25 in the quiz consisting of multiple-choice questions that attempted to test their learning through early clinical exposures.
Conclusion. This pilot exercise showed the utility of early clinical exposure integrated into the physiology course. It will be worthwhile to replicate this exercise at other institutions and among a larger student strength.
Introduction
Vertical integration in medical curriculum is defined as the integration of basic knowledge and skills of human biology within the clinical context.[1] The curricula of several medical schools include patient contact early in the first year, concurrent with basic science instructions[2] to ease the transition from classroom learning to clinical education.[3] The ‘Regulations on graduate medical education’ by the Medical Council of India (MCI)[4] and the latest MCI guidelines[5] for the undergraduate curriculum have emphasized the need of both vertical and horizontal integration for better student comprehension. Although efforts to implement this have been tried in India in the past,[6]-[7] the process of integration needs to be implemented more extensively.
Even though early clinical exposure is thought to be beneficial, its practical application still remains a challenge in the Indian scenario, given the current large class strength of 150–200 students. Equally, the implementation of vertical integration should not be lost or diluted due to apprehensions of numbers of students or class strength. As a first step to introduce vertical integration in physiology, we planned a pilot exercise at St John’s Medical College, which has a class strength of 60 students. The objectives of the exercise were first, to initiate a vertical clinical integration programme which would be well integrated into the physiology course; and second, to capture the student’s perceptions regarding the role of early clinical exposure in enhancing the understanding of the theoretical concepts and better appreciation of the practical applications of physiology.
Methods
All first year medical (MBBS) students (n>=60; 30 females)—aged 18-20 years (n>=53); 21-36 years (n>=7)—of the 2015 batch were enrolled in the exercise. The study was approved by the institutional ethics committee. The students were given a detailed explanation of the integration programme, and their informed consent was obtained.
The first challenge was to frame the practical applications of the physiological concepts. Topics of physiology course that were amenable to demonstration in the form of bedside clinics or investigative procedures were identified. Next, cases or procedures which would re-emphasize and give a broader perspective of the physiological concepts were selected, with the additional aim that students would be exposed to commonly encountered scenarios in clinical practice. After framing the proposed vertical integration, volunteer faculty of clinical departments were enrolled as resource persons. The final challenge was time management. The clinical exposures were planned such that they neither hindered the routine physiology classes nor interfered with the schedules of the clinicians, and were concurrent with the related topics taught in the theory class. The integration sessions were conducted during existing tutorial sessions, with each session lasting for an hour, in which students were taken to the hospital wards in batches of 15.
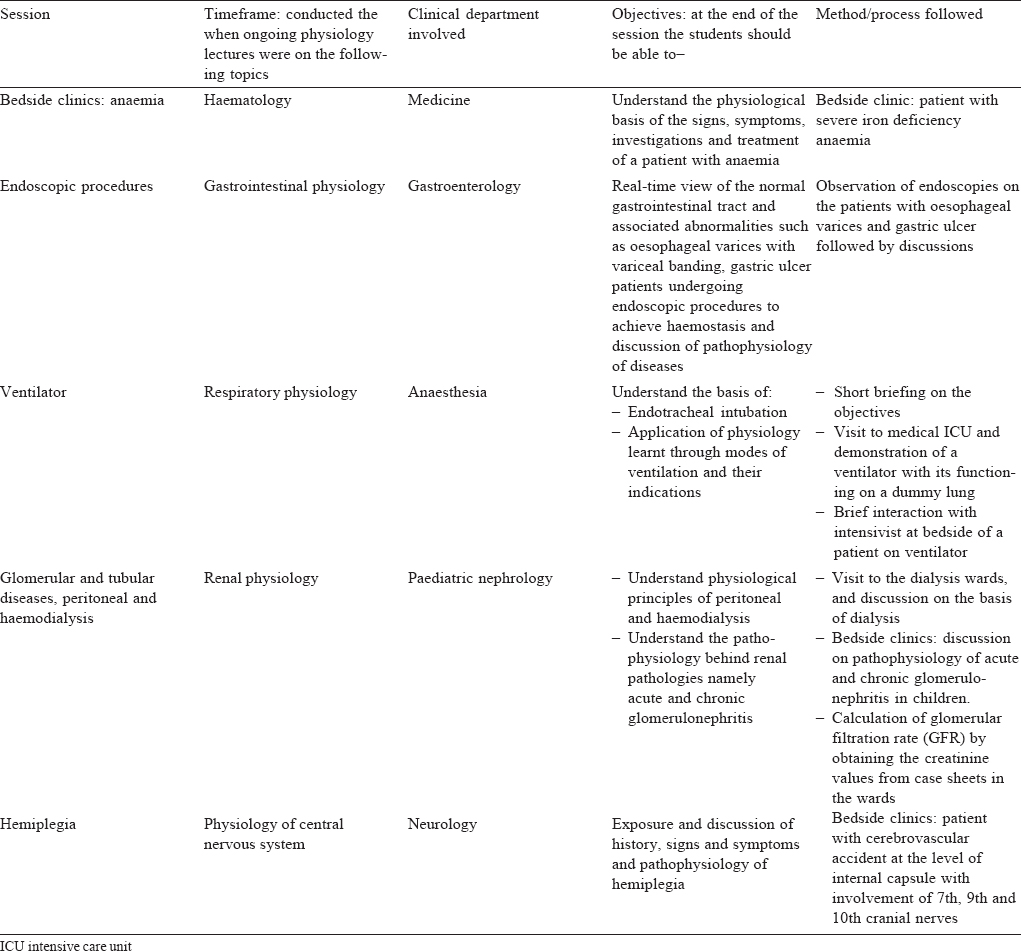
[Table - 1] gives the details of the clinical exposures, timeframes and the objectives of the sessions. For example, following the curriculum lecture on anaemia, bedside clinics on severely anaemic patients were conducted by volunteer faculty from the Depatment of Medicine, where students were exposed to the visible signs and symptoms, along with discussions of pathophysiology. During lectures on gastrointestinal tract, volunteer faculty from the Department of Gastroenterology exposed students to ongoing endoscopic procedures with appropriate applied physiology discussions. Parallel to the teaching of ventilator mechanics in respiratory physiology, students saw the application of ventilators in the intensive care unit (ICU) with volunteer faculty from the Department of Anaesthesia. Similar exercises were conducted when teaching the renal and central nervous system.
At the end of the academic year, student feedback and evaluation were conducted on an online education and interactive platform available in the institution (TYRO). The feedback was collected using a semi-structured questionnaire consisting of 5-point Likert scale and open-ended questions and was checked for construct validity. Five multiple-choice questions related to each of the clinical sessions prepared by the clinical resource persons were collated and a total of 25 questions were administered to the students. Qualitative feedback was taken from each clinician involved.
Results
The overall response rate from the students for the feedback form was 95% (57/60; 29 females). The median agreement scores for most items on the ‘completely disagree’ to ‘completely agree’ Likert scale were 4 or 5, representing agreement [Table - 2]. In isolation, the adequacy of time had 25% of students scoring less than 3. For all other items, the 25th percentile value (quartile 1) was 4, representing agreement. Apart from one student, all (98%) agreed that the topics covered during the clinical exposure were relevant during the physiology course, while 1 student was not sure. While all students felt that the sessions did not interfere with the physiology course, 6 felt that the time was inadequate. Except for 4 students (6%), the rest felt that integrated teaching helped in appreciation and application of knowledge of physiology. Among them, 98% preferred integrated teaching over traditional teaching.
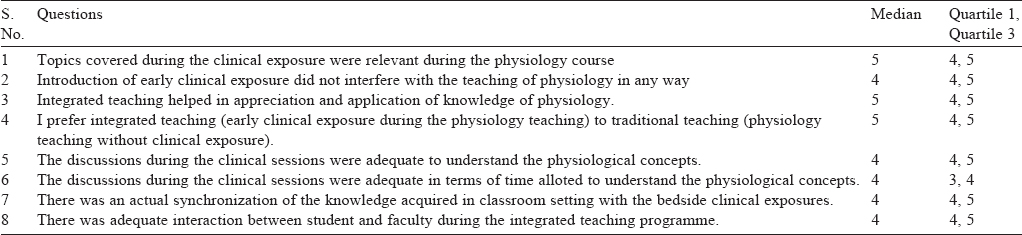
Ninety-one per cent felt the discussions during the clinical sessions were adequate to understand physiological concepts, that there was synchronization of the knowledge acquired in class-room setting with the bedside clinical exposures and there was adequate interaction between student and faculty during the integrated teaching programme. The students described several positive aspects of the programme. Most students appreciated the initiative taken by the department. They felt the programme was ' effectively integrated with the course '. They appreciated the ' opportunity to visit the hospital, interact with patients and connect their theory knowledge with clinical materials’ They indicated the sessions were ‘uniformly spread throughout theyear’. The students opined that the content and methodology was ‘good’, ‘apt and relevant, ' adequate’ and ' synchronous with the topics covered in the class’ The students expressed the limitations were time constraints and lack of adequate prior information on the clinical scenarios. Experience with children in paediatric nephrology evoked feelings of ‘sadness ', ‘sympathy ' and the realization that ' treating children requires more patience’
The students came up with many suggestions for improvement of the programme such as increasing the number of clinical exposures, providing prior details on the clinical session in the form of case sheets and to conduct tests with multiple-choice questions at the end of each session.
In relation to their learning, the students took a quiz containing 25 multiple-choice questions. This had 5 questions prepared by each of the 5 clinical resource persons. The questions were relevant to the topic covered during their clinical session in the vertical integration programme, and 59 of 60 students attempted the quiz. The mean (SD) score was 13 (2.98) of a maximum of 25 [Figure - 1]. In the feedback form, students reasoned that their performance in the quiz was ‘average’ as it was conducted at the end of the academic year. Even so, they felt that the programme helped them improve their understanding of physiology.
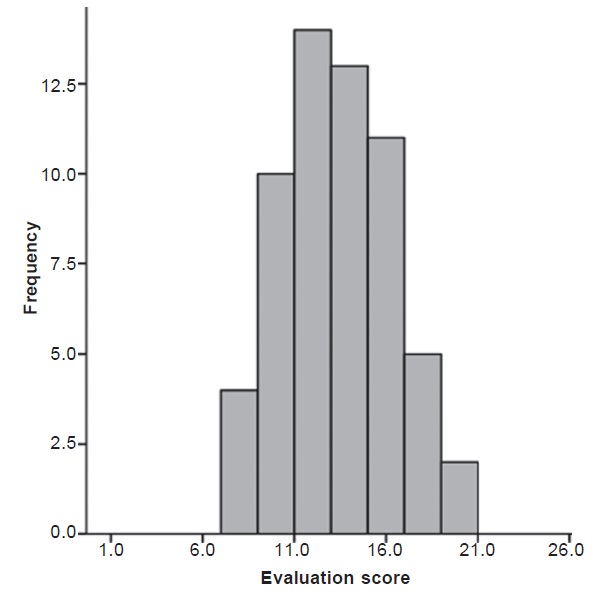 |
| Figure 1: Performance of students in the quiz |
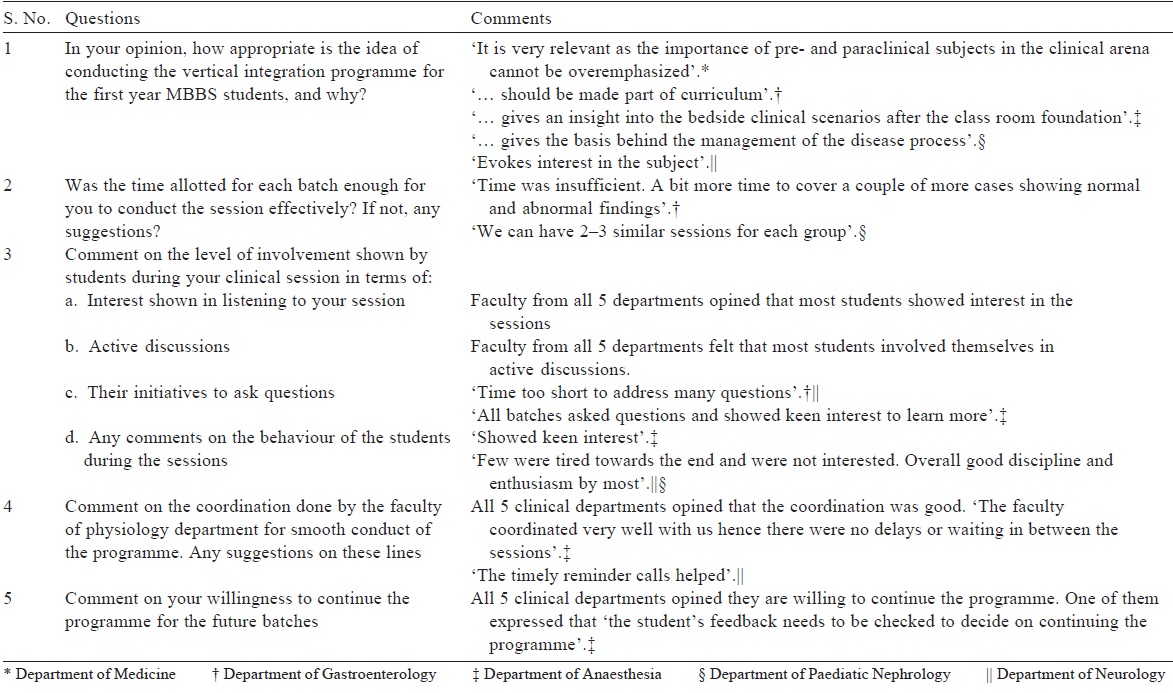
The qualitative feedback from the clinical faculty suggested that the programme was effectively integrated, absolutely essential, appropriate and relevant to the first year MBBS students as it helped them understand the importance of learning physiology [Table - 3].
Discussion
Medical education presently compartmentalizes learning such that the acquisition of knowledge is fragmented in subject silos and in time, as students progress through their medical course.[6] In this context, the introduction of horizontal integration[6],[7] and vertical integration[8] have become areas of major innovations in medical education, both in India and abroad.[9],[10] Efforts have also been made towards the interdisciplinary integration of basic sciences during the clinical years.[11] However, the challenges are many, particularly at the level of practical applications at the organizational level, in terms of additional effort by faculty in the preclinical and clinical departments, time constraints, and the potential lack of interdepartmental cooperation. In addition, and perhaps most critically, the examination system is not integrated, which leads to difficulty in student motivation.[6] Another critical barrier is the sheer number of students that are admitted in medical courses, making hospital exposure a major logistic task.
It is important to note that this study was the evaluation of a pilot programme, which defined a learning framework. The framework then needed to be evaluated, particularly in a medical college where the numbers of students was lower. St John’s Medical College, which was transitioning from 60 students per batch to 150 students per batch in 2016, was ideal, and this exercise was conducted in the last batch of 60 admitted students. Given the results of the pilot programme, in which real learnings were evident, along with student and faculty enthusiasm, the next step is to take these learnings to execute a similar programme for a batch of 150 students. This is logistically difficult. However, using information technology and real-time applications, it is possible to reduce the number of hospital visits, while enhancing student clinical experience within classrooms. Follow-up clinical visits for interested students can also be planned. Therefore, in the next iteration of this programme, several modifications, such as limiting the number of clinical visits depending on the availability of time and volunteer clinical faculty, case-based learning[8] with photos and videos of clinical cases during lectures, and real-time information technology-based sessions would make this feasible.
The results of this pilot project were encouraging with positive responses from the students. Specifically, the students indicated that the programme enhanced their understanding of the theoretical concepts of physiology, while the clinical sessions helped them appreciate the relevance of practical applications and thereby understand the purpose of learning the subject. It is important to stress that the students’ perceptions were that the clinical sessions were well integrated with the physiology course and that the programme did not interfere, but actually enhanced their curricular learning. From an organizational perspective, the programme promoted interdepartmental collaboration. The topics chosen from among the physiology curriculum, and the cases or procedures chosen from the clinical material, seemed optimal and could be continued for future batches. An important outcome would be to know the impact of this vertical integration on the level of comfort and attitudes of these students when they pursue their clinical postings in the next academic year.
While there were positive outcomes, several limitations were also apparent. In terms of generalizability of the programme, the small number (60) of students was advantageous when testing such a pilot programme. However, this model needs further testing and optimization at other medical colleges (both government and private), with larger numbers of students, along with appropriate modifications and the leveraging of new technology and teaching methods. The willingness of the faculty of various clinical departments to participate in such a programme may be subjective across institutions and would largely influence the successful implementation of the programme. The TYRO platform that was used in this programme may not be generalizable to other colleges but could be replaced by an oral or written quiz. A more judicious planning of time-frames, tailored to individual clinical department schedules, was felt to be a definite need, but can be implemented. The feedback on ‘unpreparedness’ by students for clinical sessions could be overcome by providing prior information, particularly through an information technology programme, following all ethical considerations of patient confidentiality. An ongoing assessment, with a greater number of multiple-choice questions, designed for each of the clinical exposures, could be conducted after each session. One threat that may become apparent is that preclinical faculty may see this as an erosion of their own teaching, or of superspecialty volunteer faculty taking over their role. However, integrated teaching poses no threat, when student learning is the primary aim, and challenges every faculty to deliver more.
Conclusion
Our pilot study showed that it was feasible to introduce an early clinical exposure integrated into the physiology course. The feedback, from both students and faculty, suggested that the programme was worth the considerable effort. The integration programme comes with several challenges and requires good interdepartmental coordination with faculty who are committed to ensure continuation of the programme in future years.
Acknowledgements
We would like to thank the faculty of physiology department for their enthusiastic participation and assistance. We also thank Dr Tony D.S. Raj, Dr Divya Rakesh and Dr Radhika Kishore for providing support with the TYRO platform for conducting the feedback and evaluation process.
| 1. | Snyman WD, Kroon J. Vertical and horizontal integration of knowledge and skills— a working model. Eur J Dent Educ 2005;9:26-31. [Google Scholar] |
| 2. | Spencer AL, Brosenitsch T, Levine AS, Kanter SL. Back to the basic sciences: An innovative approach to teaching senior medical students how to best integrate basic science and clinical medicine. Acad Med 2008;83:662-9. [Google Scholar] |
| 3. | Wijnen-Meijer M, Ten Cate O, van der Schaaf M, Burgers C, Borleffs J, Harendza S. Vertically integrated medical education and the readiness for practice of graduates. BMC Med Educ 2015;15:229. [Google Scholar] |
| 4. | Medical Council of India, Regulations on graduate medical education, 2012. Available at iafmonlme.in/data/circular-notifìcations/Revised-GME-2012.pdf(accessed on 7 Nov 2016). [Google Scholar] |
| 5. | Medical Council of India—Vision 2015. Available at www.mcii«dia.org/tools/ announcement/MCI_booklet.pdf (accessed on 7 Nov 2016). [Google Scholar] |
| 6. | Joglekar S, Bhuiyan PS, Kishore S. Integrated teaching—our experience. J Postgrad Med 1994;40:231-2. [Google Scholar] |
| 7. | Kalpana Kumari MK, Mysorekar VV, Raja S. Student’s perception about integrated teaching in an undergraduate medical curriculum. J Clin Diagn Res 2011 ;5:1256-9. [Google Scholar] |
| 8. | Ghosh S, Pandya HV. Implementation of an integrated learning program in neuroscience during the first year of the traditional medical course; perception of the students and faculty. BMC Med Educ 2008;8:44. [Google Scholar] |
| 9. | Schmidt H. Integrating the teaching of basic sciences, clinical sciences, and biopsychosocial issues. Acad Med 2000;73:24-31. [Google Scholar] |
| 10. | Jennifer K, Brueckner, Gould DJ. The health science faculty member’s perceptions on curricular integration: Insight and obstacles. J Int Assoc Med Sci Educ 2006; 16: 31-4. [Google Scholar] |
| 11. | Rudich A, Bashan N. An interdisciplinary course in the basic sciences for senior medical and PhD students. Acad Med 2001;76:1072-5. [Google Scholar] |
Fulltext Views
1,943
PDF downloads
590




