Translate this page into:
Economic and social impact of out-of-pocket expenditure on households of patients attending public hospitals
2 Department of Gastroenterology and Human Nutrition Unit, All India Institute of Medical Sciences, Ansari Nagar, New Delhi 110029, India
Corresponding Author:
Anoop Saraya
Department of Gastroenterology and Human Nutrition Unit, All India Institute of Medical Sciences, Ansari Nagar, New Delhi 110029
India
ansaraya@yahoo.com
| How to cite this article: Bajpai V, Singh N, Sardana H, Kumari S, Vettiyil B, Saraya A. Economic and social impact of out-of-pocket expenditure on households of patients attending public hospitals. Natl Med J India 2017;30:15-20 |
Abstract
Background. We aimed to generate evidence on the social and economic impact of out-of-pocket expenses incurred by households on illness.
Methods. We did a hospital-based cross-sectional study including a convenience sample of 374 inpatients and outpatients.
Results. The median illness expenditure was the same (₹62 500) for inpatients and outpatients. Of all respondents, 51.3% among the rural and 65.5% among the urban patients were employed before illness, but after illness only 24.4% among the rural and 23.4% among the urban patients remained in employment. The proportion of rural households of different socioeconomic categories that experienced decrease in expenditure on food, education and health, and those who had to sell land or cattle, and the education of whose children suffered was statistically significant. The proportion of indebted families in different socioeconomic classes was also statistically significant among both rural and urban patients. The lowest socioeconomic strata depended mostly upon the financial support of their friends to tide over the financial crisis of an illness.
Conclusion. Our study shows that out-of-pocket expenses on healthcare are a burden not only for the poor but also the middle classes.
Introduction
The impoverishing effect of out-of-pocket expenditure on healthcare on households is well known.[1],[2],[3] However, the health policy framework in India has not been able to address the difficulties of patients and their families. Among other measures, encouraging the growth of markets in healthcare and levying of user charges in public health facilities are two policy measures that have added to the burden of out-of-pocket expenditure of households on healthcare. Most studies on out-of-pocket expenditure on healthcare from India are population-based surveys. We based our study on interviews of patients attending tertiary and secondary care public hospitals.
Methods
We conducted this study among outpatients and inpatients of the Department of Gastroenterology and Human Nutrition Unit, inpatients of the Department of Cardiology, All India Institute of Medical Sciences (AIIMS), New Delhi and the outpatients and inpatients of the Comprehensive Rural Health Services Project (CRHSP) hospital, Ballabgarh, Haryana of AIIMS between September–October 2005 and January 2006.
Verbal consent was obtained from each respondent before filling the proforma. The interviewer explained all the pertinent information related to the study, allowed the respondents to ask questions and verified that they understood what was explained to them. We enrolled a convenience sample of 374 respondents; all patients recruited in the study had an illness for less than a year.
We used a predesigned and pretested semi-structured interview schedule with both closed-ended and open-ended questions containing information on various study variables. Pretesting of the interview schedule was done by administering it to 20 participants. The data collected from pretesting are not included in the results presented. We administered the questionnaire to patients and/or any adult family member close to them.
The questions included those on possession of and knowledge regarding below poverty line (BPL) cards, changes in household dietary intake in the wake of illness, per capita income of the household, illness expenditure, changes in the employment status due to illness, indebtedness, source of loan, status of savings, sale of movable and immovable property, changes in household expenditure on food, education and health and changes in the employment status of the spouse and children in the wake of illness. The change in household expenditure on food, education and health on account of illness in the family was elicited in terms of ‘increased’, ‘decreased’ or ‘remained same’, rather than as actual expenditure in rupees. The overall expenditure incurred on the treatment of illness till the time of recruitment into the study was included. For the total expenditure incurred on illness we did ask for approximate expenditure on different components of out-of-pocket expenditure to corroborate the total out-of-pocket expenditure on illness reported. However, we did not use this in our final analysis as the information was only approximate and our priority was to generate data on the social and economic impact of out-of-pocket expenditure rather than analyse the expenditure per se.
Socioeconomic status
The per capita income of the patients’ families and their socioeconomic status was defined as per the Kuppuswamy's[4] socioeconomic status scale revision for the year 2003.[1]
Statistics
Categorical variables were summarized as frequency (%). Quantitative variables were checked for normal distribution. Variables following normal distribution were summarized as mean (SD). Variables following non-normal distribution were summarized as median (range). The chi-square/Fisher exact test was used to determine statistical association of the categorical variables. The Student t-test/Wilcoxon Rank sum test was used to compare average values between the two groups. A p value <0.05 was considered statistically significant. All statistical analyses were done using STATA 9.0 (Statacorp, Texas, USA).
Results
The median expenditure on illness among all the respondents was similar in outpatients and inpatients, as well as for urban and rural patients [Table - 1]. There was little difference in the expenditure on illness by different socioeconomic classes in rural and urban areas, for example the median expenditure for all classes in urban areas was ₹50 000 (p>0.05].
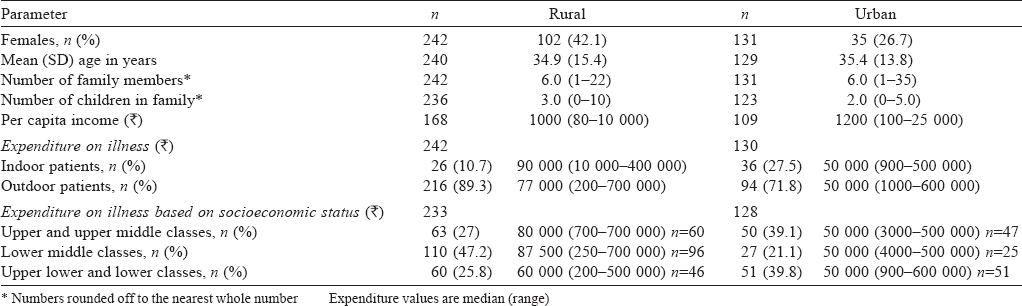
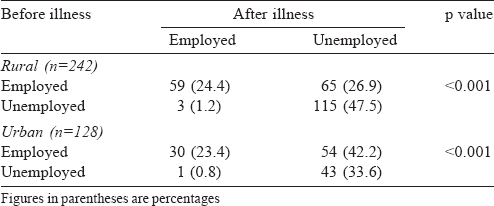
Among rural respondents, 51.3% were employed before their illness but only 24.4% were employed after the illness. The corresponding figures for urban respondents were 65.6% and 23.4%. Both changes were statistically significant. Similarly, there was a significant decrease in the mean number of earning members per family after the illness [Table - 2].
The economic and the social impact of illness on rural as well as urban families in terms of decrease in expenditure on food, education and health, as well as the need to sell land or cattle and the impact on the education of children was statistically significant [Table - 3]. Similarly, the proportion of urban households of different socioeconomic categories, which experienced decrease in savings and expenditure on food and health, as well as households where the spouse started working were significant [Table - 3].
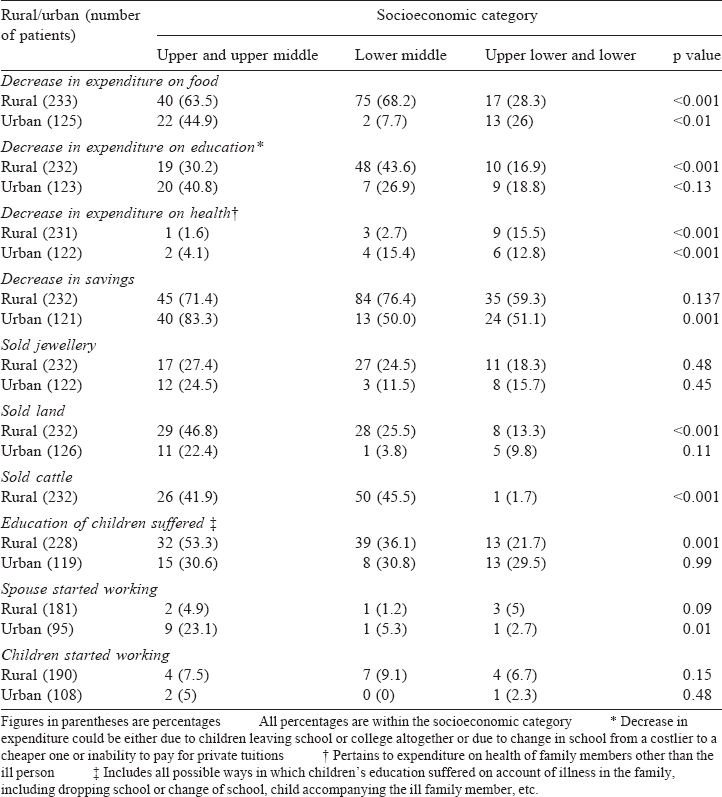
A considerable proportion of the upper and upper middle classes were also affected socioeconomically—63.5% of rural and 44.9% of urban families decreased their expenditure on food. Among the lowest socioeconomic classes, 28.3% of rural and 26% of urban families faced similar difficulties. Similarly, the proportion of families from the upper socioeconomic classes that had to sell land to meet treatment-related expenses was much higher than the proportion of other socioeconomic classes.
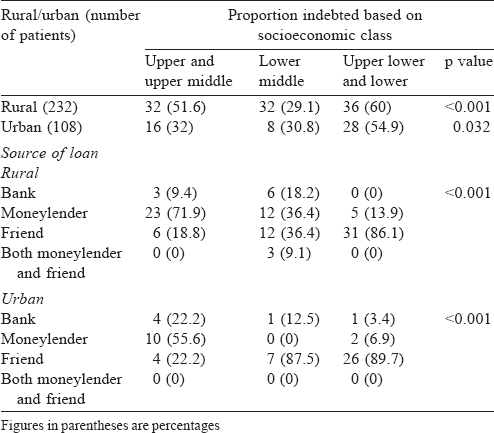
The distribution of proportion of indebted families in different socioeconomic classes was statistically significant among both rural and urban patients [Table - 4]. Bank loans were accessed more often by the upper socioeconomic classes and moneylenders were the most common source of loan for the upper and middle classes. The lower socioeconomic classes depended upon financial support of their friends to tide over the financial crisis.
Discussion
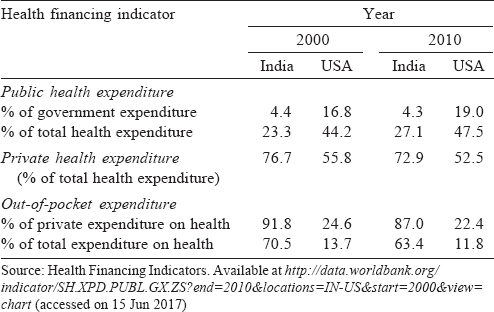
The Constitution enshrines India as a ‘sovereign socialist secular democratic republic’,[5] so it is important to highlight the political context of high out-of-pocket costs on healthcare in India. On the other hand, the USA is a beacon of entrepreneurial capitalism. A comparison of the health financing indicators of India and the USA brings out the paradox [Table - 5].[6] For each indicator, the USA seems to be more ‘socialist’ in the delivery of healthcare compared to India.
While our results show similar expenditure among outpatients and inpatients, this is due to a large number of patients with chronic illnesses being included in our study. As many of the inpatients had been on long follow-up and had been treated earlier as outpatients, it was not possible to categorize illness episodes as outpatient and inpatient. This is a limitation of our study and an aspect that needs to be addressed in the methodology in future studies.
High out-of-pocket expenses on illness of a patient can not only impoverish the family, but can make the economic recovery challenging. This has been variously described as a ‘poverty ratchet’[7] or ‘medical poverty trap’.[8] WHO estimates put nearly a 100 million people around the world who are poor due to healthcare costs, while another 150 million suffer due to catastrophic expenditure on health.[9] Many studies from India have shown that people have been pushed into poverty on account of out-of-pocket expenses on healthcare.[2],[10],[11]
A household confronted with an illness is obliged to meet varied expenses—the cost of treatment and transport, opportunity costs for the sufferer and caregivers and the cost of caring, besides other routine household expenses. The process of meeting these costs can impact household consumption expenditure and the standard of living. Households may simultaneously adopt coping strategies such as borrowing money at high interests, cutting back on food consumption, sale of assets, etc., which potentially push them into a cascading cycle of poverty. Gertler and Gruber[12] provided evidence of health shocks leading to decreased supply of family labour and thereby reduced family incomes. Russell[13] has shown that for a family surviving on a daily income barely enough to meet minimum dietary requirements, even a minor illness may well prove to be the proverbial ‘last straw’. Evidence shows that the consequences of health shocks are not borne equally by members of the household, with women and children being worse off.[14] Social class[15],[16],[17] and caste[15],[18] are important determinants of how successfully a household can weather a health crisis.
We have used the lessons drawn from the above studies to map our conceptual understanding of the pathways to economic and social impact of out-of-pocket expenditure on healthcare [Figure - 1].
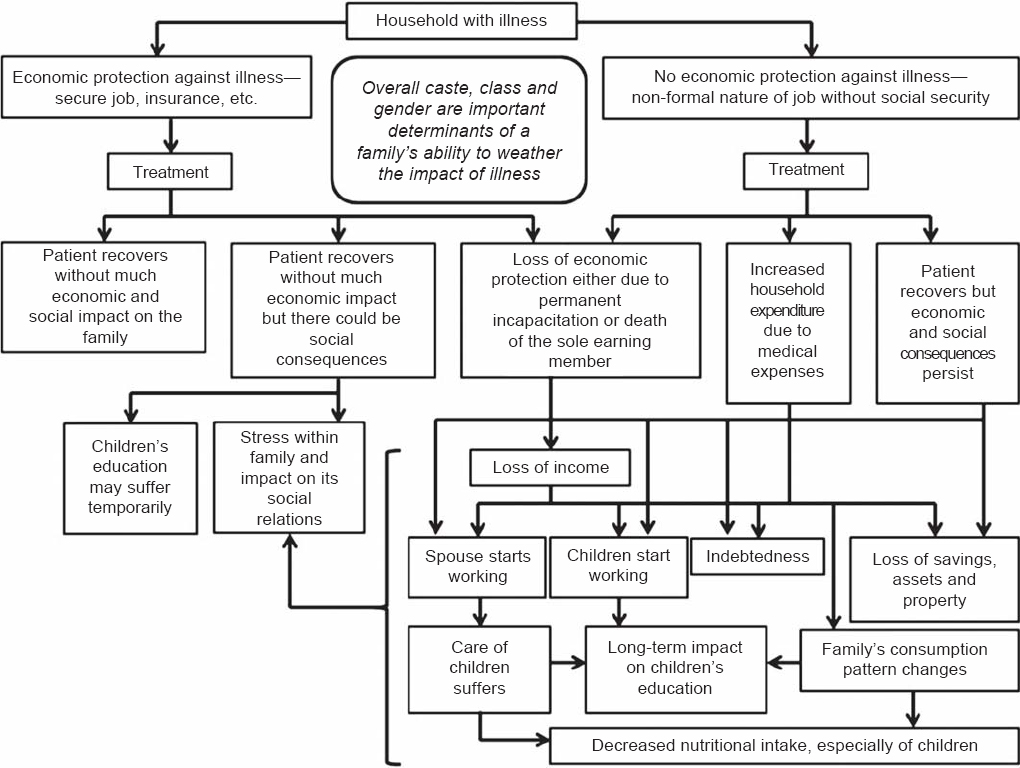 |
| Figure 1: Conceptual framework of economic and social impact of out-of-pocket expenditure on health Note: Any depiction of such a conceptual framework can only be a simplification of the real-life conditions. We have taken here two extreme scenarios—one where there is full economic protection afforded by a secure job or insurance cover, and the other scenario where there is little economic protection for the family braving illness. In reality, however, there could be many scenarios that lie between these two situations. |
Socioeconomic class and cost of treatment
The results of our study can be understood only in the ‘context’ of related developments in society with respect to healthcare. This ‘context’ is defined by the National Sample Survey Organization (NSSO) data.
We found that people from lower socioeconomic background were a minority in our sample while one would expect them to comprise a majority of patients at public health hospitals. As we used a convenience sample it is possible that this was by chance, but it could also suggest that treatment even in public hospitals is gradually getting out of reach for some of the poorest sections of society.
There has been a rise in the cost of treatment in both public and private hospitals, after adjusting for a general rise in prices [Table - 6]. Moreover, the rise has been marginally higher in public hospitals as compared to private hospitals. In successive NSSO rounds there has been an increase in the number of untreated ailments due to financial reasons [Table - 7].[19] Hence, the perception that treatment in public hospitals is subsidized is gradually withering away. This, in our opinion, is a consequence of a policy that has promoted, directly or indirectly, large-scale commercialization of services of public hospitals and user charges for different services have become the norm rather than an exception.
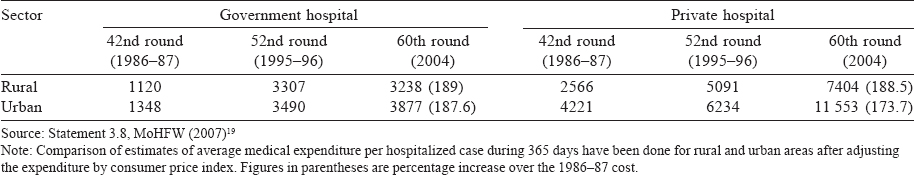
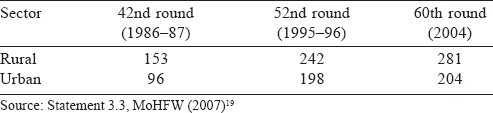
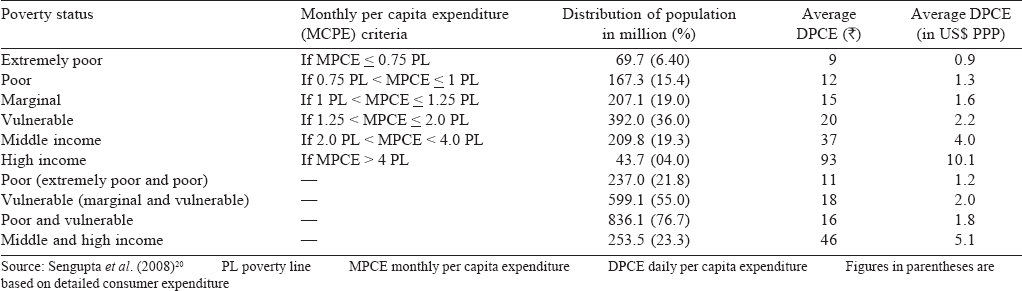
While for a lower socioeconomic class access to any form of healthcare is difficult, even the middle and upper sections of the society are finding healthcare to be expensive and at times beyond their means. However, user charges in public hospitals are exempted only to those who have a below poverty line (BPL) card. The problems of public policy on this issue is further illustrated by how the middle and high income groups are defined based on the national consumer expenditure surveys [Table - 8].[20] In 2004–05, a daily per capita expenditure (DPCE) of ₹93 was categorized as ‘high income’. The average cost of hospitalized care in a government hospital in rural areas in 2004 was ₹3238 [Table - 6]. If we presume an average stay of 7 days for each hospitalization, ₹3238 would amount to an expenditure of ₹462.6 per day per hospitalization. For a person with a DPCE of ₹93 this would be an enormous additional burden.
Among the reasons for rising costs of treatment is that consumables such as medicines are often not available and need to be purchased.[1],[21] Due to long waiting times for diagnostic investigations, patients often need to or prefer to get these done at private diagnostic centres. There is also a tendency to over-investigate patients and practise ‘defensive’ medicine.
We believe that our data on total treatment expenditure reported by patients was reasonably accurate as in all instances the duration of illness was less than a year and hence allowed for a relatively accurate recall of the expenses. Also, patients with chronic illnesses generally have fixed monthly expenditures and this too is helpful in recalling reasonably accurate expenses for treatment.
Loss of employment due to illness
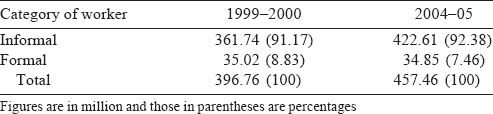
There was a significant decline in the employment status of both urban and rural patients. As we did not gather information on the sector (organized or unorganized) and nature of employment (formal or informal), we can only surmise the reasons for this decrease. Possibly, most patients and their family members were either self-employed or informal workers in the organized/unorganized sector. Such employment provides little job security during an illness.
The movement by the government in the 1990s to outsourcing led to a change with more workers in the informal sector [Table - 9].[22] This has had implications [Figure - 1] for such households on account of expenditure on healthcare in the absence of any healthcare cover/insurance being made available to them.
Other changes
Barring ‘decrease in expenditure on health’ and ‘sale of cattle’, the upper and upper middle socioeconomic classes were the worst sufferers [Table - 3]. While 63.5% and 44.9% of the upper socioeconomic households among rural and urban patients, respectively, experienced a decline in their expenditure on food, these proportions were 28.3% and 26%, respectively, among the lower socioeconomic class. This difference between the upper and lower classes was significant for both rural and urban patients. A possible explanation for this could be that many lower socioeconomic households were consuming such low quantities of food that there was not much scope for further decrease in food consumption. As the upper socioeconomic classes had relatively better food consumption, the decline in their consumption was more prominent.
Similarly, the changes with respect to decrease in expenditure on education can be explained by families withdrawing children from public schools and putting them in government schools while others withdrew tuitions or decreased expenditure on books, notebooks, stationery or other ancillary items. In the lower classes, the expenditure on education may have been low to start with.
In rural India, social classes are based on ownership of land. The lower socioeconomic classes are usually landless agricultural labourers or marginal farmers while the upper classes have land holdings.[23],[24] This is reflected in the significant difference in the proportion of rural households of different classes who had to sell land to meet expenditure on illness. The same could be the case with sale of cattle where again the difference in the proportion of families among different classes resorting to sale was significant.
Indebtedness status and the source of loan
The lower socioeconomic classes were expectedly the most indebted; but next to them were the upper and the upper middle classes rather than the intermediate class. Among rural upper and upper middle class families, more than 50% were indebted; this corroborates our finding that among these classes the proportion of families who sold land and cattle was 46.8% and 41.9%, respectively. Even though the lack of availability of institutional loans at low rates of interest to meet illness expenses is of concern, it must be noted that even for the better off sections it is the moneylender who is the source of immediate relief. On the other hand, the poor go without treatment if they fail to raise money from friends and relatives as they are shunned both by banks and the moneylender due to their low creditworthiness.
Conclusion
Our study shows that out-of-pocket expenses on healthcare are not only a formidable obstacle for the poor, but also a drag for the ‘middle classes’ of India. Scrapping ‘user charges’ altogether from the public health system is imperative to improve access to healthcare for large sections of our population.
| 1. | Garg CC, Karan A. Reducing out-of-pocket expenditures to reduce poverty: A disaggregated analysis at rural-urban and state level in India. Health Policy Plan 2009;24:116–28. [Google Scholar] |
| 2. | Bhandari L, Berman P, Ahuja R. The impoverishing effect of healthcare payments in India: New methodology and findings. Eco Pol Wkly 2010;45:65–71. [Google Scholar] |
| 3. | Binnendijk E, Koren R, Dror DM. Hardship financing of healthcare among rural poor m Orissa, India. BMC Health Serv Res 2012;12:23. doi: 10.1186/1472-6963-12-23. [Google Scholar] |
| 4. | Mishra D, Singh HP. Kuppuswamy socioeconomic status scale—a revision. Indian J Pediatr 2003;70:273–4. [Google Scholar] |
| 5. | The Constitution of India (as modified up to the 1st December, 2007). Available at http://lawmin.nic.in/coi/coiason29july08.pdf (accessed on 26 Feb 2014). [Google Scholar] |
| 6. | World Bank. Health Financing Indicators. Available at http://data.worldbank.org/indicator/SH.XP D. PUBL. GX. ZS?end=201 0&locations=IN- US&start=2000&view=chart (accessed on 15 Jun 2017). [Google Scholar] |
| 7. | Chambers R. Poverty unperceived: Traps, biases and agenda. IDS Working Paper 270. Brighton, UK:Institute of Development Studies, University of Sussex; July 2006. [Google Scholar] |
| 8. | Whitehead M, Dahlgren G, Evans T. Equity and health sector reforms: Can low income countries escape the medical poverty trap? Lancet 2001;358:833–6. [Google Scholar] |
| 9. | WHO. World Health Report: Health system financing—the path to universal coverage. Geneva:WHO; 2010. [Google Scholar] |
| 10. | Garg CC, Karan A. Health and Millennium Development Goal 1: Reducing out-of-pocket expenditures to reduce income poverty—evidence from India, EQUITAP Project: Working Paper # 15. Available at www.esocialsciences.org/Download/repecDownload. aspx?fname=Document172200840.4928247.pdf&fcategory=Articles&AId=1378&fref=repec (accessed on 15 Jun 2017). [Google Scholar] |
| 11. | van Doorslaer E, O'Donnell O, Rannan-Eliya RP, Somanathan A, Adhikari SR, Akkazieva B, et al. Paying out-of-pocket for health care in Asia: Catastrophic and poverty impact. EQUITAP Working Paper 2, Erasmus University, Rotterdam and IPS, Colombo, May 2005. Available at www.esocialsciences.org/Download/repec Download.aspx?fname=Document172200840.4928247.pdf&fcategory=Articles& Aid=823&fref=repec (accessed on 15 Jun 2017). [Google Scholar] |
| 12. | Gertler P, Gruber J. Insuring consumption against illness. Am Eco Rev 2002;92: 51–76. [Google Scholar] |
| 13. | Russell SJ. Can households afford to be ill? The role of the health system, material resources and social networks in Sri Lanka. PhD thesis. London School of Hygiene and Tropical Medicine, London, United Kingdom; 2001. doi: 10.17037/PUBS.00682239. [Google Scholar] |
| 14. | Dercon S, Krishnan P. In sickness and in health: Risk-sharing within households in rural Ethiopia. J Pol Eco 2000;108:688–727. [Google Scholar] |
| 15. | Duggal R. Inequities in access to health care. In: Nilangi S, Shukla A (eds). A report on health inequities in Maharashtra. Report prepared by SATHI (Support for Advocacy and Training into Health Initiatives) for Maharashtra Health Equity and Rights Watch, Implemented in collaboration with CEHAT and TISS; 2008:29–7. [Google Scholar] |
| 16. | Patil SS, Berad AS, Angadi MM. A study to assess catastrophic household expenditure on childhood illness in an urban slum in Bijapur. Indian J Community Med 2009; 34:335–7. [Google Scholar] |
| 17. | Pal R. Analysing catastrophic OOP health expenditure in India: Concepts, determinants and policy implications, Working Paper 2010-001. Mumbai:Indira Gandhi Institute of Development Research; February 2010. Available at www.igidr.ac.in/pdf/publication/WP-2010-001.pdf (accessed on 30 May 2016). [Google Scholar] |
| 18. | Mukherjee S, Haddad S, Narayana D. Social class related inequalities in household health expenditure and economic burden: Evidence from Kerala, south India. Int J Equity Health 2011;10:1. doi: 10.1186/1475-9276-10-1. [Google Scholar] |
| 19. | Ministry of Health and Family Welfare. Select health parameters: A comparative analysis across the National Sample Survey Organization (NSSO) 42nd, 52nd and 60th Rounds. MoHFW:Government of India; 2007. [Google Scholar] |
| 20. | Sengupta A, Raveendran G, Kannan KP. India's common people: Who are they, how many are they and how do they live? Eco Pol Wkly 2008;43:49–63. [Google Scholar] |
| 21. | Alam M, Tyagi RP. A study of out of pocket household expenditure on drugs and medical services: An exploratory analysis of UP, Rajasthan and Delhi. Delhi:Population Research Centre, Institute of Economic Growth; 2009:118–34. [Google Scholar] |
| 22. | Srivastava R. Changing employment conditions of the Indian workforce and implications for decent work. Global Labour J 1 2012;3(1):63–90. [Google Scholar] |
| 23. | Patnaik U. Class differentiation within the peasantry: An approach to analysis of Indian agriculture. Eco Pol Wkly 1976;11(39):A82–A85, A87–A101. [Google Scholar] |
| 24. | Mehta J. Changing agrarian structure in Indian economy. Revolutionary Democracy 2004;10:(1). Available at http://revolutionarydemocracy.org/rdv10n1/agrarian.htm (accessed on 15 Jun 2017). [Google Scholar] |
Fulltext Views
3,525
PDF downloads
2,722




