Translate this page into:
Evaluation of a novel flushing protocol for a peripherally inserted central catheter (PICC) in the neurological intensive care unit: A prospective randomized study
2 Neuro-ICU, Critical Care Medicine Department, West China Hospital, Sichuan University, No. 37 Guo Xue Xiang, Chengdu 610041, P.R. China
Corresponding Author:
Fan Liu
Department of Nursing, West China Hospital of Stomatology, Sichuan University, 14# Renmin, South Road No. 3, Chengdu 610041
P.R. China
samotj@163.com
| How to cite this article: Liu F, Liao T, Wang Q, Tao Y. Evaluation of a novel flushing protocol for a peripherally inserted central catheter (PICC) in the neurological intensive care unit: A prospective randomized study. Natl Med J India 2018;31:5-7 |
Abstract
Background Peripherally inserted central catheters (PICCs) are increasingly used in critical care units. Venous arterial blood management protection (VAMP) for PICCs could decrease the rate of blockage of PICCs. We investigated whether a novel flushing method for PICCs could decrease the risk of venous thromboembolism (VT) and catheter-associated bloodstream infections (CABSIs) compared to the traditional flushing method.
Methods In this prospective randomized study, we evaluated 360 patients with PICCs who were admitted to our neurological intensive care unit from March 2012 to February 201 4. The patients were randomized into the experimental group (n= 186) and the control group (n= 174). The VAMP-system flushing method was used in the experimental group whereas in the control group the PICCs were flushed with a 10 ml syringe of saline. Baseline clinical information, blockage rate of PICCs, occurrence of VT and CABSIs and average time for flushing (seconds per flushing time) were compared and analysed.
Results The occurrence of CABSIs and average time for flushing were statistically lower in the experimental group. The rate of blockage of PICCs, proportion of male subjects, age of subjects, APACHE II score and length of stay in hospital showed no significant differences between the two groups.
Conclusion This study showed that the VAMP-system flushing method is simple to use and may be more beneficial for patients with a PICC; it may also lower the risk of CABSIs.
Introduction
Peripherally inserted central catheters (PICCs) are frequently used in intensive care units (ICUs).[1] In comparison to centrally inserted central catheters (CICCs), insertion of a PICC is much easier, and the risk of a haemothorax, pneumothorax or the possibility of a primary malposition can be avoided.[2],[3] Compared to a central venous access device (CVAD), using a PICC is better in patients with coagulation disorders.[2],[4]
PICCs can also be used in sick patients who have malnutrition, obesity or severe cardiopulmonary problems.[3] However, the longer duration of use of a venous access device (VAD), including PICCs, could increase the risk of venous occlusion and catheter-associated bloodstream infections (CABSIs).[5],[6] Thus, we hypothesized that using a novel flushing protocol with a closed blood conservation device (venous arterial blood management protection, VAMP) for PICCs could decrease the rate of blockage of the PICC and CABSIs. VAMP was originally marketed for decreasing requirements for transfusion of packed red blood cells (PRBCs). However, as there are no data showing the advantages of VAMP compared to the traditional method, we did a randomized controlled trial to ascertain the differences between the two methods of flushing in PICCs in terms of occlusion, infection, cost and time spent.
Methods
Trial design
This study was a single-centre, controlled, double-blinded, randomized trial. Patients with severe neurological illnesses such as cerebral haemorrhage, aneurysms, etc., were admitted to the Neurological Critical Care Medicine Department, West China Hospital, Sichuan University. Patients who underwent the PICC procedure from March 2012 to February 2014 were randomized to the experimental and control groups. Written informed consent was obtained.
Participants
PICCs were placed by the vascular access team which included nurses and nurse practitioners specifically trained in insertion of PICCs using aseptic precautions. The position of the PICC was confirmed on a chest X-ray by an attending radiologist. Patients with the following were excluded: local contraindications such as a skin infection or burns; PICC implantation with a three-way valve; insertion through the supraclavicular, femoral or external carotid approach; and patients requiring continuous infusion and a strict liquid input limitation.
Interventions
The experimental group received the flushing protocol using the VAMP system (Edwards Lifesciences, Irvine, CA, USA), which has been described previously.[7] First, 5 ml of saline was drawn into the reservoir, which was in a fully closed position. Second, the existing venous catheter was opened and all the fluids were re-infused into the venous line under positive pressure and in an impulse mode. The control group received the traditional flushing method, which was by disconnecting the infusion tube, and then injecting saline with a 10 ml syringe. Both procedures were repeated every 4 hours.
Outcomes
These were rate of occlusion, rate of CABSI and the average time for flushing during the hospital stay.
Allocation and implementation
Randomization was predetermined, and assignment to the treatment arm was done using sealed envelopes. Participants and those assessing the outcomes were blinded. The study was approved by the ethics committee of the West China Hospital of Sichuan University. The research assistant ensured that appropriate interventions were carried out depending on the group. Clinical project coordinators regularly monitored the accuracy of recruitment and data collection as well as strict compliance to the study protocol. The following clinical information was recorded: gender, age, Acute Physiology and Chronic Health Evaluation (APACHE) II score, ICU length of stay (LOS), duration of dwelling time for the device, average amount of time for flushing, incidence of CABSIs and occlusion rate during maintenance.
Analysis
The variables were expressed as mean (SD) and numbers (percentages); categorical variables were compared using the chi-square test, and continuous variables were compared using Student’s t-test. A 2-tailed p<0.05 was considered statistically significant. The data were analysed using SPSS version 22.
Results
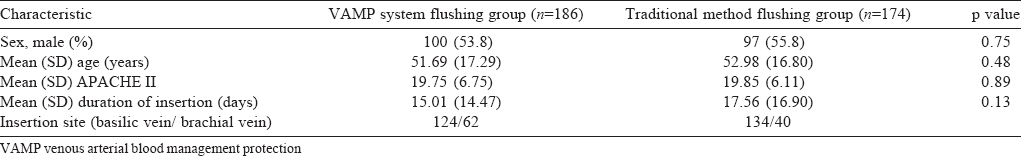
Of the 360 patients who had a PICC placed, 186 patients were randomized to the active VAMP system group and 174 to the traditional method [Figure - 1]. There were no significant differences between those in the VAMP system and the traditional method in terms of age, sex or APACHE II scores [Table - 1].
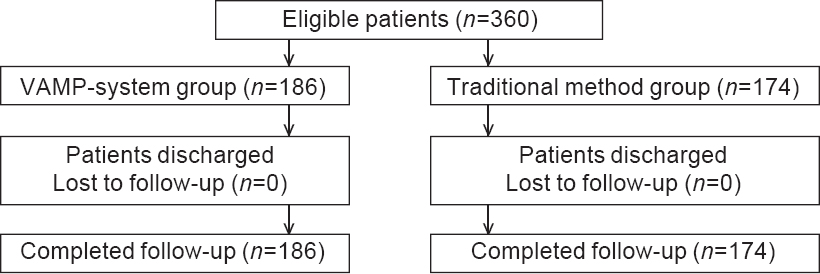 |
| Figure 1: Participant flow |
The occurrence of CABSIs and the average time for flushing were statistically lower in the VAMP flushing system group. There was no obvious difference in the occlusion rates of both systems (p=0.36). In 1 patient in the traditional method group, occlusion of the PICC required its removal. The other episodes of occlusion were transient and overcome by flushing. Seven patients in the traditional method group, and one in the VAMP flushing system group had CABSIs [Table - 2].

Discussion
The first clinical application experience of PICCs in the ICU was reported in 1996.[8] Recently, the results of this experience have been particularly promising; for example, power-injectable PICCs are capable of central venous pressure monitoring and are used for high-velocity infusion of radio-contrast agents during computed tomography scans and other radiological procedures. Moreover, power injectors can tolerate pressures as high as 300 psi.[3] Because of these advantages, power-injectable PICCs can be considered for use in ICUs.[9] However, reports about the use of VAMP for flushing of PICCs are scarce. This is possibly the first study to assess the differences in occlusion, infection and time used in VAMP flushing compared to traditional method in critically ill patients in the ICU.
The rate of occlusion was low regardless of which method was used to flush. The low rate of occlusion in our study may be explained by the choice of a vein with an appropriate diameter. With regard to the incidence of infections, accumulated evidence suggests that the rate of infection in PICCs is lower than that in CVCs because the exit site is less prone to contamination (the upper mid-arm skin is specific for a lower bacterial colonization compared to the skin in the infraclavicular area).[2],[10],[11] A recent study reviewed 37 PICCs in a burns unit[12] and found that the incidence of PICC-related bloodstream infections was zero episodes for 1000 catheter-days. Another study in a surgical ICU[13] reported that PICCs had 2.2 episodes of CABSIs per 1000 catheter-days.
We had anticipated that VAMP flushing was likely to have a lower rate of infection compared with the traditional method. However, that was not the case and consistent with previous studies,[12],[14] we too found the rate of CABSIs to be low. Flushing of PICCs is done to keep it patent by reducing the precipitation of any drugs or the formation of any clots inside the lumen.[15] Flushing should be done before and after the administration of drugs, before locking the device, after obtaining blood samples and after parenteral nutrition or blood products. Thus, flushing can be a time-consuming event in the ICU where a number of other such activities also have to be done for each patient. Although the VAMP system is more expensive than traditional equipment, it can be used to collect blood samples without needles. Thus, VAMP flushing is more convenient and has the advantage of reducing procedure time, preventing needle stick injuries and improving work efficiency.
We did not assess the long-term outcomes of our patients and our study was a single-centre study and hence may not be generalizable to other institutions, which have a different workflow and patient profile.
Conclusions
This prospective trial suggests that the VAMP flushing protocol for a PICC could be effectively used in most ICU patients with a similar occlusion rate as with the traditional method. VAMP flushing was better in minimizing CABSIs and decreasing the flushing time. However, VAMP flushing is more expensive.
Funding. None
Conflicts of interest: None
| 1. | Griffiths VR, Philpot P. Peripherally inserted central catheters (PICCs): Do they have a role in the care of the critically ill patient? Intensive Crit Care Nurs 2002; 18:37-47. [Google Scholar] |
| 2. | Pittiruti M, Hamilton H, Biffi R, MacFie J, Pertkiewicz M; ESPEN. ESPEN guidelines on parenteral nutrition: Central venous catheters (access, care, diagnosis and therapy of complications). Clin Nutr 2009;28:365-77. [Google Scholar] |
| 3. | Pittiruti M, Brutti A, Celentano D, Pomponi M, Biasucci DG, Annetta MG, et al. Clinical experience with power-injectable PICCs in intensive care patients. Crit Care 2012;16:R21. [Google Scholar] |
| 4. | Gallieni M, Pittiruti M, Biffi R. Vascular access in oncology patients. CA Cancer J Clin 2008;58:323-46. [Google Scholar] |
| 5. | Hadaway LC. Best-practice interventions: Keeping central line infection at bay. Nursing 2006;36:58-63, quiz 63-4. [Google Scholar] |
| 6. | Cowl CT, Weinstock JV, Al-Jurf A, Ephgrave K, Murray JA, Dillon K. Complications and cost associated with parenteral nutrition delivered to hospitalized patients through either subclavian or peripherally-inserted central catheters. Clin Nutr 2000; 19:237-43. [Google Scholar] |
| 7. | Silver MJ, Jubran H, Stein S, McSweeney T, Jubran F. Evaluation of a new blood-conserving arterial line system for patients in intensive care units. Crit Care Med 1993;21:507-11. [Google Scholar] |
| 8. | Ng PK, Ault MJ, Maldonado LS. Peripherally inserted central catheters in the intensive care unit. J Intensive Care Med 1996;11:49-54. [Google Scholar] |
| 9. | Cotogni P, Pittiruti M. Focus on peripherally inserted central catheters in critically ill patients. World J Crit Care Med 2014;3:80-94. [Google Scholar] |
| 10. | Loveday HP, Wilson JA, Pratt RJ, Golsorkhi M, Tingle A, Bak A; UK Department of Health. epic3: National evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect 2014;86 (Suppl 1):S1-70. [Google Scholar] |
| 11. | Pratt RJ, Pellowe CM, Wilson JA, Loveday HP, Harper PJ, Jones SR, et al. epic2: National evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect 2007;65 (Suppl 1):S1-64. [Google Scholar] |
| 12. | Fearonce G, Faraklas I, Saffle JR, Cochran A. Peripherally inserted central venous catheters and central venous catheters in burn patients: A comparative review. J Burn Care Res 2010;31:31-5. [Google Scholar] |
| 13. | Gunst M, Matsushima K, Vanek S, Gunst R, Shafi S, Frankel H. Peripherally inserted central catheters may lower the incidence of catheter-related blood stream infections in patients in surgical intensive care units. Surg Infect (Larchmt) 2011;12:279-82. [Google Scholar] |
| 14. | Trerotola SO, Stavropoulos SW, Mondschein JI, Patel AA, Fishman N, Fuchs B, et al. Triple-lumen peripherally inserted central catheter in patients in the critical care unit: Prospective evaluation. Radiology 2010;256:312-20. [Google Scholar] |
| 15. | Vescia S, Baumgärtner AK, Jacobs VR, Kiechle-Bahat M, Rody A, Loibl S, et al. Management of venous port systems in oncology: A review of current evidence. Ann Oncol 2008;19:9�15. [Google Scholar] |
Fulltext Views
3,818
PDF downloads
13,870




