Translate this page into:
Feasibility study of a low-cost powered air-purifying respirator (PAPR): A hospital-based simulation study to assess the perception of healthcare professionals
Correspondence to AYYAPPAN AJAN; ayyappan.ajan@ammachilabs.org
[To cite: Ajan A, von Lieres JS, Jayan V, Sai Bala M, Sasi DD, Mohandas R, et al. Feasibility study of a low-cost powered air-purifying respirator (PAPR): A hospital-based simulation to assess the perception of healthcare professionals. Natl Med J India 2024;37:315–21. DOI: 10.25259/NMJI_905_2022]
Abstract
Background
There is a need for affordable and effective air-filtering respirators, that provide the user protection against infection and are comfortable to wear. Among the various air-filtering respirators, powered air-purifying respirators (PAPR) that supply the user with filtered air through a powered system provide better protection than the commonly used N-95 masks, that directly filters the air that surrounds the user, with filtration efficiency of these procedures being up to 99.99% and up to 95%, respectively. However, in India, the PAPRs are imported, making them unaffordable. Engineers at our university developed a low-cost PAPR model. We investigated the feasibility of using this low-cost PAPR as a potential air-filtering respirator as part of personal protective equipment.
Methods
In a simulation study, 20 woman nurses wore an N-95 mask with face shield, or the low-cost PAPR in two separate sessions and performed routine nursing tasks. They then answered questionnaires to assess their perceived comfort and suitability for the tasks.
Results
The low-cost PAPR provided better breathing comfort and vision. However, the current N-95 mask system was perceived to be more suitable for tasks requiring high mobility.
Discussion
Our study demonstrated the feasibility of the low-cost PAPR model, particularly for low-mobility tasks.
INTRODUCTION
In healthcare settings with risk of disease transmission through contact, droplets, and airborne particles,1,2 healthcare workers need to use appropriate personal protective equipment (PPE).3 These include: (i) eye and face protection, (ii) hand protection, (iii) body protection, (iv) hearing protection, and (v) respiratory protection.4 For respiratory protection, two types of air-filtering respirators are used, namely filtering facepiece respirators (FFRs) and powered air-purifying respirators (PAPRs). The most common FFR is the N-95 respirator, also referred to as N-95 mask. N-95 masks are designed for close facial fit and filter at least 95% of airborne particles larger than 0.3 microns from the inhaled air.5 As per Occupational Safety and Health Administration (OSHA) of the USA, PAPR is defined as ‘air-purifying respirator that uses a blower to force the ambient air through air-purifying elements to the inlet covering’.6
Efficacy of respirators is measured as assigned protection factor (APF), i.e. the protection a respirator offers when the wearer follows the respiratory protection rules.5 The APF values of N-95 mask and hood-powered PAPR, are 10 and 25, respectively, indicating that the latter provides more effective filtration.
The two types of respirators have other advantages and limitations. Some healthcare workers report headache following the use of N-95 masks,7 which can be mitigated by using PAPR.8 On the other hand, PAPRs have the disadvantages of noise that may impact hearing,9–14 high cost, large size, and a time-consuming donning and doffing process.15 Moreover, inadequate air flow rate in a tight-fitting PAPR may impair the worker’s performance, facial cooling, and respirator comfort.16
During an outbreak of severe acute respiratory syndrome (SARS), the majority of healthcare workers (84%) preferred PAPR over N-95 masks.17 In a study simulating the typical hospital environment, users preferred PAPRs over N-95 mask in 11 of 16 preference categories.18 In a low-temperature environment during low to moderate work for one hour, there was no significant difference between the N-95 and PAPR in the measurements of cardiopulmonary variables, facial and overall body heat perception, and perceived breathing ability.19 In a field observation study, it was found that those respondents wearing PAPR had a higher heat tolerance but were limited by low mobility and audibility.20,21
In India, PAPRs are, for the most part, imported and hence expensive (around ₹100 000 or US$ 1280 each) and thus unaffordable.
Engineers of our university developed a low-cost PAPR (₹30 000), with the aim of making PAPR affordable, while mitigating the drawbacks of the N-95 masks, namely facial heating, a sensation of suffocation, and fogging of the face shield. After working on 3 progressively enhanced prototypes, a final low-cost PAPR22,23 has been developed,24 with features of a PAPR as per the National Institute for Occupational Safety and Health (NIOSH) standards and a higher airflow rate.25 It is in the process of certification.
A major factor deciding the choice of a respirator is the perceived comfort of healthcare workers in delivering patient care after donning these. We assessed the feasibility for use of the low-cost PAPR in a hospital setting, based on the perception of healthcare workers as compared to the N-95 mask system while performing routine hospital tasks.
METHODS
Twenty female nurses with a mean (SD) age of 25.8 (1.8) years who had at least 1 year of professional experience (mean [SD] 2.9 [1.6]) years in current position) and provided informed consent were included in the study. They had prior experience of using an N-95 mask for 4.0 (2.7) months but had no prior experience of using a PAPR. They were trained in donning and doffing of the low-cost PAPR through videos and instruction manuals for one week prior to the study.
The participants rated their prior experience with the tasks to be performed in the study using a 3-point Likert scale (‘very experienced,’ ‘somewhat experienced,’ or ‘inexperienced’). Thereafter, each participant underwent two sessions, wearing one of the two respirators being compared in turn, and performed six nursing tasks––(i) recording vital signs, (ii) communication with and counseling of patient and bystanders, (iii) taking care of patients’ dietary needs, (iv) moving the patient from bed to wheelchair, (v) back care (cleaning and massaging the back to stimulate circulation, prevent bedsores, and provide emotional relaxation), and (vi) bed making. The order in which the two respirators were worn was haphazard.
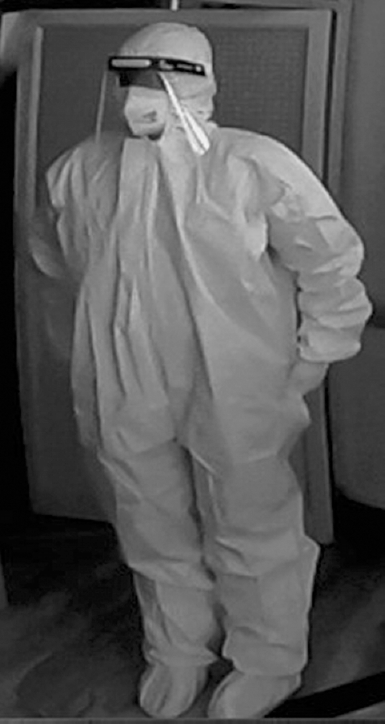
During the two sessions, the participants wore PPE comprising a full body suit and gloves, and one of the two respirators–– (i) the low-cost PAPR (Fig 1), or (ii) N-95 mask system (N-95 mask plus a face shield; Fig 2). The N-95 mask used (Aero 2N95 FFP2 mask head-loop with cord-lock [medium]) had Indian Standards Institution certification. The PAPR consisted of a hood, a breather tube, a blower and a 12 V lithium-ion battery; the battery and the blower were located in a backpack. The system had an airflow of 10 cubic feet per minute, noise level of below 70 db, and could operate for more than 10 hours a day. The hood was manufactured by a company that was certified by the International Organization for Standardization (ISO 13485:2016).

- Low-cost powered air-purifying respirator (PAPR)
- N-95 mask and face shield
The sessions were conducted in a vacant 5-bed intermediate respiratory care unit (IRCU) at ambient temperature. Each participant was assigned one bed with a simulated patient (another study participant) for performing the tasks described above, while being observed by one of the investigators to ensure that the participant executed the assigned tasks correctly. The procedure was then repeated with the other respirator (Fig. 3).
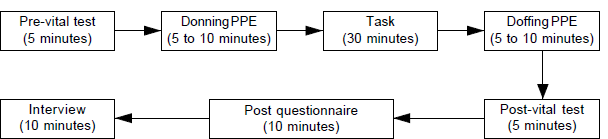
- Flow diagram of the sessions PPE personal protective equipment
After each session, the participants were asked to rate their perception of comfort while performing the six nursing tasks in 16 domains, each using a Likert scale of 1–5 (Table I). They were also asked to indicate (Yes or No) whether they had experienced discomfort, in the form of back pain, dizziness or eye irritation, while doing the prescribed tasks. At the end of the PAPR session, they were also asked to rate whether they were able to perform a selection of assembly and donning tasks, the time taken to do these, and the level of comfort with certain aspects of wearing the PAPR (Table II).
| Category | N-95 mask (Median) | PAPR (Median) | p value | Effect size r |
|---|---|---|---|---|
| Overall general comfort | 3.5 | 3 | 0.166 | –0.219 |
| Overall breathing comfort | 3 | 4 | <0.001 | –0.57 |
| Facial and body heat | 4 | 3 | 0.011 | –0.40 |
| Pressure or pain | 2 | 3 | 0.002 | –0.48 |
| Eye discomfort | 3 | 1 | 0.004 | –0.45 |
| Clear line of vision | 3 | 4 | <0.001 | –0.57 |
| Difficulty of donning | 2 | 3 | 0.013 | –0.39 |
| Difficulty in operating the respiratory protection system | 2 | 3 | 0.032 | –0.33 |
| Difficulty of doffing | 2 | 3 | 0.056 | –0.30 |
| Flexibility of the respiratory protection system during tasks | 4 | 3 | 0.002 | –0.49 |
| Were you able to hear properly while working with the respiratory protection system? | 4 | 2 | 0.001 | –0.50 |
| Perceived efficiency against biological hazards | 3 | 3.5 | 0.717 | –0.057 |
| Were you able you to communicate properly? | 3.5 | 3 | 0.053 | –0.30 |
| How many hours do you think you could wear this respiratory protection system continuously? | 4 | 3 | 0.007 | –0.42 |
| Overall flexibility of the respiratory protection system | 4 | 3 | 0.016 | –0.38 |
| Overall assessment | 4 | 3 | 0.138 | –0.23 |
| Assembly and donning task | Yes | No | Some of them |
|---|---|---|---|
| Were you able to place the items in the specified pockets of the bag without confusion? | 16 (80) | 3 (15) | 1 (5) |
| Where you able to check the working of the blower? | 18 (90) | 0 | 2 (10) |
| Where you able to connect the battery and blower terminals? | 19 (95) | 1 (5) | 0 |
| Where you able to identify the battery switch and voltage level indicator of the battery and proceed accordingly? | 20 (100) | 0 | 0 |
| Where you able to identify the PAPR items according to the user manual given? | 19 (95) | 0 | 1 (5) |
| Time for assembly and donning (minutes) | 0–5 | 5–10 | >10 |
| How long did it take you for the assembly? | 4 (20) | 12 (60) | 4 (20) |
| How long did it take you for the donning? | 5 (25) | 10 (50) | 5 (25) |
| Comfort in assembly and donning | Poor | Fair | Good |
| Comfortable with the assembled bag around your waist? | 3 (15) | 7 (35) | 10 (50) |
| Comfortable with the breather tube connection between the hood and blower? | 1 (5) | 5 (25) | 14 (70) |
| Comfortable with the hood on the head? | 4 (20) | 7 (35) | 9 (45) |
| Which part of the assembly was the most difficult? | n | ||
| Placing the items in specified pockets of the bag | 2 (10) | ||
| Checking the working of the blower | 3 (15) | ||
| Connection between the battery and blower | 6 (30) | ||
| None of the above | 6 (30) | ||
| Others | 3 (15) |
Figures in parentheses are percentages
Further, the participants were asked to indicate which respirator (‘PAPR’ or ‘N-95 mask’) they preferred, they perceived as more effective, and found more acceptable for doing low mobility tasks (tasks 5 and 6), medium mobility tasks (tasks 1 and 4), or high mobility tasks (tasks 2 and 3).
The participants had their vital signs measured before and after the six tasks in each session. These included axillary temperature (using a digital thermometer), pulse rate, peripheral arterial oxygen saturation (SpO2) with a pulse oximeter, and respiration rate (by the participant counting the number of breaths). Changes in vital signs were obtained by subtracting the values before starting the tasks to the values after completing the tasks. The effect size ‘r’ was calculated for each Wilcoxon signed-rank test.
The participants were also interviewed regarding their experience using semi-structured interviews. The open-ended answers were coded and analyzed using a content analysis method.
The study was approved by our Institutional Ethics Committee and registered with Clinical Trials Registry–India (CTRI). The data were analyzed using the Wilcoxon signed-rank, Cochran’s Q, and McNemar tests, with Statistical Package for the Social Sciences (SPSS) version 25, at an α-level of 0.05.
RESULTS
Prior experience of nursing tasks
Most participants reported that they were ‘very experienced’ with performing each of the 6 selected tasks (Table III). The lowest rated experience level was with ‘changing position from bed to wheelchair.’ Two participants reported that they did not have experience in ‘patient communications/counseling of bystander.’
| Task | Very experienced (%) | Somewhat experienced (%) | Inexperienced (%) |
|---|---|---|---|
| 1. Bed making | 15 (79) | 4 (21) | 0 |
| 2. Back care | 16 (84) | 3 (16) | 0 |
| 3. Position changing from bed to wheelchair | 11 (58) | 8 (42) | 0 |
| 4. Supporting the patient in dietary needs; providing food at the bedside; assisting patients for food hygiene | 16 (84) | 3 (16) | 0 |
| 5. Patient communication/counseling of bystander to patient; ward orientation and general awareness to bystanders (through telephone: about medicine and material purchase) | 13 (69) | 4 (21) | 2 (10) |
| 6. Checking vital signs (temperature, pulse rate, respiration rate, oxygen saturation) | 17 (90) | 2 (10) | 0 |
Perceived comfort with N-95 mask versus PAPR
PAPR was perceived as significantly more comfortable with respect to overall breathing comfort, facial and body heat, less eye discomfort, and clear line of vision. By comparison, the participants experienced significantly more pressure or pain, more difficulty in donning, more difficulty in operating the respirator, reduced flexibility of the respirator during tasks, impaired ability to hear properly while working with the respirator, and thought that they could wear the respirator continuously for a shorter time, and lower overall flexibility of the respirator (Table I).
The overall general comfort, efficiency against biological hazards, and overall assessment had a small effect with r<0.3. Facial and body heat, pressure or pain, eye discomfort, the difficulty of donning, difficulty to operate the respirator, flexibility, hearing, and overall flexibility of the respirator had a medium effect with 0.3<r< 0.5. Overall breathing comfort and clear line of vision had a large effect with r>0.5.
Users’ preference, perceived effectiveness, and acceptance of the respirator
Three Cochrane’s Q tests were performed to determine whether there were differences among the following three dichotomous dependent variables: (i) ‘prefer N-95 mask v. prefer PAPR’; (ii) ‘perceive N-95 mask as more effective v. perceive PAPR as more effective’; and (iii) ‘accept N-95 mask more v. accept PAPR more’ while performing the high, medium, and low mobility nursing tasks (Table IV). During the low mobility tasks, a significantly higher proportion of participants preferred, found effective, and accepted the low-cost PAPR. During high mobility tasks, a significantly higher number of participants preferred, found effective, and accepted the N-95 mask system.
| Mobility task | Preference | Perceived effectiveness | Acceptance | |||
|---|---|---|---|---|---|---|
| N-95 mask PAPR | N-95 mask PAPR | N-95 mask PAPR | ||||
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Low | 4 (20) | 16 (80) | 2 (10) | 18 (90) | 4 (20) | 16 (80) |
| Medium | 13 (65) | 7 (35) | 10 (50) | 10 (50) | 12 (60) | 8 (40) |
| High | 19 (95) | 1 (5) | 19 (95) | 1 (5) | 18 (90) | 2 (10) |
| Cochran’s Q | 20.11 | 22.84 | 16.44 | |||
| p value | <0.001 | <0.001 | <0.001 | |||
Bodily discomfort of wearing low-cost PAPR versus the N-95 mask
There was a statistically significant difference in the proportion of participants suffering from back pain, eye irritation, feeling of suffocation, and subjective temperature rise between the N-95 mask and PAPR (p<0.05). A higher proportion of participants suffered from back pain during the PAPR session, but a higher proportion of participants suffered from eye irritation, feeling of suffocation, and subjective temperature rise in the N-95 mask session (Table V).
| Bodily discomfort | N-95 mask | PAPR | p value | ||
|---|---|---|---|---|---|
| Yes | No | Yes | No | ||
| Back pain | 1 | 19 | 8 | 12 | 0.039 |
| Dizziness | 3 | 17 | 2 | 18 | 1.0 |
| Eye irritation | 9 | 11 | 2 | 18 | 0.016 |
| Suffocation | 16 | 4 | 7 | 13 | 0.012 |
| Sweating | 20 | 0 | 16 | 4 | 0.125 |
| Subjective temperature rise | 11 | 9 | 3 | 17 | 0.008 |
| Headache | 2 | 18 | 8 | 12 | 0.07 |
| Hunger | 7 | 13 | 2 | 18 | 0.063 |
| Nausea | 1 | 19 | 0 | 20 | 1.0 |
| Urinary urgency | 4 | 16 | 2 | 18 | 0.5 |
| Unusual smell | 1 | 19 | 0 | 20 | 1.0 |
| Thirst | 14 | 6 | 10 | 10 | 0.125 |
Participants’ competency in the assembly and donning of low-cost PAPR
Most of the participants were able to identify the PAPR items stated in the user manual, check the working of the blower, connect the battery and blower terminals, place the items in the specified pockets of the bag without confusion, and identify the battery switch and voltage level indicator of the battery. Most of the participants took 5–10 minutes for the assembly and donning. The most difficult part of donning was the breather tube connection. The majority of participants rated the comfort of the assembled bag around the waist as fair or good, as well as the breather tube connection between the hood and blower, and the hood on the head.
Vital signs while doing the tasks with the low-cost PAPR and the N-95 mask
There was no significant difference in the changes in vital signs between the two respirators (Table VI).
| Vital sign | Type of protection | Difference between pre- and post-task | p value | Effect size (r) | |
|---|---|---|---|---|---|
| Mean (SD) | Median | ||||
| Pulse | N-95 mask | 2.9 (8.79) | 1.0 | 0.588 | 0.085 |
| PAPR | 1.5 (7.35) | 1.0 | |||
| Respiratory rate | N-95 mask | 1.63 (2.241) | 2.0 | 0.974 | 0.005 |
| PAPR | 1.71 (1.614) | 2.0 | |||
| Oxygen saturation | N-95 mask | –1.05 (1.932) | –1.0 | 0.503 | 0.105 |
| PAPR | –0.40 (1.846) | –0.5 | |||
| Temperature | N-95 mask | –0.49 (1.571) | –0.3 | 0.643 | 0.073 |
| PAPR | –0.13 (1.385) | 0 | |||
Evaluation of the two types of respirators via semi-structured interviews
The majority of participants’ felt that both the N-95 mask and the low-cost PAPR had good airflow (Table VII). The N-95 mask was problematic concerning heat, feeling of suffocation, sweating, and fogging. The low-cost PAPR’s main drawbacks were related to weight, communication, and flexibility. The N-95 mask was regarded as useful in treating Covid-19 patients, whereas the low-cost PAPR was regarded as useful for low-mobility tasks. The N-95 mask was most suitable for nurses and the low-cost PAPR was most suitable for doctors. Most of the participants had prior experience in using the N-95 mask, while none of them had used a PAPR along with the PPE before.
| N-95 mask | n (%) | PAPR | n (%) |
|---|---|---|---|
| Where does the respiratory protection system work well? | |||
| Only initial difficulty | 2 (10) | Full protection | 2 (10) |
| Better than PAPR | 1 (50) | Good air flow | 14 (70) |
| Communications | 2 (10) | Good vision | 8 (40) |
| Mobility | 3 (15) | Low suffocation | 10 (50) |
| Emergency situations | 3 (15) | ||
| Protective | 15 (75) | ||
| Where does the respiratory protection system need improvement? | |||
| Communication difficulties | 4 (20) | Noise of blower | 5 (25) |
| Heat | 8 (40) | Weight | 18 (90) |
| Fogging on the face shield | 7 (35) | Not suitable for emergency tasks | 8 (40) |
| Suffocation | 7 (35) | Low flexibility | 14 (70) |
| Sweating | 7 (35) | Communication difficulties | 16 (80) |
| What if any, would you use the respiratory protection system for? | |||
| All the tasks | 2 (10) | Treating Covid positive patients | 2 (10) |
| Treating Covid positive patients | 6 (30) | While contacting difficulties | 1 (5) |
| Emergency | 2 (10) | Low mobility task | 16 (80) |
| High mobility task | 4 (20) | ||
| While in patient contact and patient care | 5 (25) | ||
| Who would the respiratory protection system be most valuable for? | |||
| All healthcare workers | 2 (10) | Doctors | 13 (65) |
| Nurses | 18 (90) | Nurses | 7 (35) |
| If you have to explain about the respiratory protection system, what would you say? | |||
| Initial difficulties only | 2 (10) | Initial difficulties only | 2 (10) |
| Very useful while dealing with Covid patients | 18 (90) | Weight is not so comfortable | 3 (15) |
| Low flexibility | 2 (10) | ||
| Good air flow | 18 (90) | ||
| Communication problem | 2 (10) | ||
| Suitable for low mobility tasks | 4 (20) | ||
| Protection | 6 (30) | ||
| Have you used any similar systems? How would you compare them? | |||
| Have used 3-layer mask along with N-95 mask for extra protection | 1 (5) | Never used this system or similar systems | 20 (100) |
| Have used the same system with different full body suit material | 4 (20) | ||
| Have used the same system | 15 (75) | ||
DISCUSSION
The majority of study participants said that they were either very experienced or somewhat experienced with almost all the nursing tasks included in the study. When the perceived comfort of wearing the N-95 mask was compared with the low-cost PAPR, some categories of comfort were rated in favour of the PAPR. The main difference between the two respirators was that powered air was being supplied into the hood of the PAPR. With powered airflow, a PAPR could provide breathing comfort, reduce facial heat, sweating, and fogging. This was possibly the reason for participants’ preference for the PAPR for ‘more overall breathing comfort,’ ‘less facial and body heat,’ ‘less eye discomfort,’ and ‘more clear line of vision.’ Particularly the categories ‘overall breathing comfort’ and ‘clear line of vision’ showed a large effect size.
However, some categories were rated in favour of the N-95. During the PAPR session, the participants reported significantly more ‘pressure or pain,’ more ‘difficulty in donning,’ more ‘difficulty in operating the respiratory protection gear,’ less ‘flexibility during tasks,’ less ‘ability to hear properly,’ ‘fewer hours that they thought they could wear it continuously,’ and less ‘overall flexibility of the respiratory protection gear.’ These categories showed a medium effect size. The PAPR had numerous components, such as a blower, battery, breather tube hood, and waist bag, to be assembled before donning and to be disassembled for doffing. With the N-95 mask, only the mask and face shield had to be dealt with for donning and doffing. Fewer items on the body could provide more flexibility, less pressure or pain, and enable the participants to work for longer hours. The PAPR blower was noisy, and could be the reason for participants rating ‘communication’ in favour of the N-95 mask.
The participants’ preference, perceived effectiveness, and acceptance for a particular respirator showed significant differences depending on the mobility requirement of the task. A larger number preferred, perceived as effective, and accepted the PAPR for low mobility tasks, such as vital signs measurement and patient communications/counseling of bystanders. This could be due to airflow inside the hood of the PAPR, which gave the participants breathing comfort, but did not allow for flexibility of movement. The N-95 mask was preferred for high mobility tasks requiring much movement and bending, such as bed making and changing the patients’ position from bed to wheelchair. During the semi-structured interviews, the participants also mentioned that they would prefer the N-95 mask if they had to do cardiopulmonary resuscitation (CPR). These findings are in line with a similar study that found that 50% of the participants preferred the N-95 mask over three types of PAPRs because the N-95 mask was lightweight, easy to wear, and easy to use.18
When comparing bodily discomforts while wearing the N-95 mask versus the low-cost PAPR, the participants complained of back pain more frequently while using the PAPR. This could be due to the backpack of the PAPR that contained a battery weighing 1 kg. However, while using the N-95 mask, the participants had more eye irritation, feeling of suffocation, and subjective temperature rise. This could be due to the lack of airflow, which causes breathing difficulty, sweating, and fogging of the face shield, making it unsuitable for clear vision. Other studies had shown that the use of the N-95 masks as part of the PPE caused tiredness, fogging, headache, mask soakage, and breathing difficulties.26
There were no significant differences in vital signs before and after tasks between the N-95 and PAPR. However, changes in vital signs need not be a strong indicator to evaluate the respirators, because there are other factors, such as the type of the tasks, that could cause changes in vital signs rather than the type of respirator.19,27
When the ability of the participants regarding the assembly and donning of the PAPR was assessed, most participants were quite proficient. The most challenging part of the donning process was the breather tube connection, which needs to be improved in future constructions of the PAPR. Overall, most participants were satisfied with the comfort of the assembled parts of the PAPR.
In the interviews, the participants felt the N-95 mask was a good source of protection. could be especially useful for dealing with Covid-19 patients, high mobility tasks, and emergency patient care. However, the participants felt that the N-95 mask still needed improvement. Due to the lack of airflow, the N-95 mask caused sensations of increased facial heat, suffocation, sweating, and fogging. Some of the participants experienced communication difficulties while wearing the N-95 mask.
Regarding the PAPRs, participants felt the system was protective and had good airflow, a low sense of suffocation, and clear visibility. They preferred PAPR for low mobility tasks or tasks requiring fewer movements, due to lack of flexibility. The PAPR also led to communication issues due to the noise of the blower. Some of the participants felt that they could become used to the PAPR system in the long run, just as they became used to the N-95 mask, as none of them had any previous experience using a PAPR. Most of the participants also felt that the PAPR system could be more useful for doctors who did not perform many tasks that required much movement.
The limitations of our study include the small sample size. A larger and more representative sample would have yielded more generalizable results. All the participants had prior experience with using the N-95 mask, while none of them had used a PAPR before, this could have biased the results. We also did not include male nurses or doctors.
Conclusion
We demonstrated the feasibility of the low-cost PAPR model and its advantages compared to the N-95 mask, especially for low-mobility tasks. Most participants found it easier to breathe while wearing the PAPR compared to the N-95 mask and their face shield was not fogged, which gave them better vision. However, the additional components and items of the PAPR had added weight that nurses had to carry. The noise of the air blower (70 dB, measured using digital sound level meter) also impaired communication. Moreover, the PAPR restricted movements, hence the majority of participants preferred it for low mobility tasks. The participants suggested that the PAPR would be useful for doctors as their tasks did not require as much mobility. A PAPR model that allows for more flexibility of movement and that makes less noise may be more comfortable to use for all health workers.
References
- The health of the healthcare workers. Indian J Occup Environ Med. 2016;20:71-2.
- [CrossRef] [PubMed] [Google Scholar]
- Occupational Safety and Health Administration nd.a., b Healthcare. Infectious diseases. Available at www.osha.gov/healthcare/infectious-diseases (accessed on 7 Mar 2022).
- [Google Scholar]
- Occupational Safety and Health Administration. [Internet] n.d.a., a Control and Prevention. Available at www.osha.gov/coronavirus/control-prevention (accessed on 25 May 2022)
- [Google Scholar]
- Environmental health and safety. 2022. Types of PPE. Available at https://ehs.ucmerced.edu/researchers-labs/ppe/selection (accessed on 7 Mar 2022)
- [Google Scholar]
- Personal protective equipment (PPE) Available at www.physiopedia.com/Personal_Protective_Equipment_(PPE) (accessed on 7 Mar 2022)
- [Google Scholar]
- Occupational Safety and Health Administration n.d.a., c 1910.134-Respiratory protection. Occupational safety and health standards. Available at www.osha.gov/laws-regs/regulations/standardnumber/1910/1910.134 (accessed on 8 Mar 2022).
- [Google Scholar]
- Headaches and the N95 facemask amongst healthcare providers. Acta Neurol Scand. 2006;113:199-202.
- [CrossRef] [PubMed] [Google Scholar]
- PAPR restores the N95 face mask induced cerebral hemodynamic alterations among healthcare workers during COVID-19 outbreak. J Neurol Sci. 2020;417:117078.
- [CrossRef] [PubMed] [Google Scholar]
- Feasibility of cleft lip and palate repair in personal protective equipment (PPE) J Plast Reconstr Aesthet Surg. 2021;74:644-710.
- [CrossRef] [PubMed] [Google Scholar]
- CDC prevention epicenters program. A systematic risk-based strategy to select personal protective equipment for infectious diseases. Am J Infect Control. 2020;48:46-51.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of powered air-purifying respirators on speech recognition among health care workers. Otolaryngol Head Neck Surg. 2021;164:87-90.
- [CrossRef] [PubMed] [Google Scholar]
- Pilot study to examine the use of a powered air purifying respirator (PAPR) in the operating room. Am J Infect Control. 2017;45:S84.
- [CrossRef] [Google Scholar]
- Powered respirators are effective, sustainable, and cost-effective personal protective equipment for SARS-CoV-2. Front Med Technol. 2021;3:729658.
- [CrossRef] [PubMed] [Google Scholar]
- Diminished speech intelligibility associated with certain types of respirators worn by healthcare workers. J Occup Environ Hyg. 2009;7:63-70.
- [CrossRef] [PubMed] [Google Scholar]
- Selection and use of respiratory protection by healthcare workers to protect from infectious diseases in hospital settings. Ann Work Expo Health. 2020;64:368-77.
- [CrossRef] [PubMed] [Google Scholar]
- Exercise performance while wearing a tight-fitting powered air purifying respirator with limited flow. J Occup Environ Hyg. 2005;2:368-73.
- [CrossRef] [PubMed] [Google Scholar]
- The changing face of healthcare worker perceptions on powered airpurifying respirators during the SARS outbreak. Respirology. 2005;10:107-10.
- [CrossRef] [PubMed] [Google Scholar]
- Analysis of user preference with N95 and powered air-purifying respirators in a healthcare work environment. In: Graduate Theses, Dissertations, and Problem Reports. West Virginia University at WVU; 2019. p. :63.
- [Google Scholar]
- Powered air-purifying respirator use in healthcare: Effects on thermal sensations and comfort. J Occup Environ Hyg. 2017;14:947-54.
- [CrossRef] [PubMed] [Google Scholar]
- Use of powered air-purifying respirator (PAPR) by healthcare workers for preventing highly infectious viral diseases-A systematic review of evidence. Syst Rev. 2020;9:173.
- [CrossRef] [PubMed] [Google Scholar]
- Use of powered air-purifying respirator (PAPR) as part of protective equipment against SARS-CoV-2: A narrative review and critical appraisal of evidence. Am J Infect Control. 2021;49:492-9.
- [CrossRef] [PubMed] [Google Scholar]
- A highly cost-effective powered air purifying respirator for frontline workers. Available at https://youtu.be/2oznLSqkT2w (accessed on 8 Mar 2022)
- [Google Scholar]
- Amrita launches a desi low-cost PAPR kits for healthcare workers. Available at https://amrita.edu/news/amrita-launches-desilow-cost-papr-kits-healthcare-workers/ (accessed on 8 Mar 2022)
- [Google Scholar]
- Design and development of a low-cost powered air-purifying respirator for frontline medical workers for COVID-19 response. In: Proceedings of 8th R10 Humanitarian Technology Conference (R10-HTC); Kuching. Malaysia; 2020. IEEE
- [CrossRef] [Google Scholar]
- The use and effectiveness of powered air purifying respirators in health care: Workshop summary Washington (DC): National Academies Press (US); 2015. (accessed on 8 Mar 2022). 10.17226/18990
- [CrossRef] [Google Scholar]
- Physiological effects of N95 FFP and PPE in healthcare workers in COVID intensive care unit. Indian J Crit Care Med. 2020;24:1169-73.
- [CrossRef] [PubMed] [Google Scholar]
- Preference and user experience with powered air purifying respirators in healthcare workers in a simulated work environment: A pilot study Graduate Theses, Dissertations, and Problem Reports West Virginia University at WVU; 2018.
- [Google Scholar]




