Translate this page into:
Graduate Medical Education Regulations 2019: Competency-driven contextual curriculum
Corresponding Author:
Avinash Supe
Department of Surgical Gastroenterology, K.E.M. Hospital and Medical Education and Major Hospitals Division, Municipal Corporation of Greater Mumbai, Mumbai, Maharashtra
India
avisupe@gmail.com
| How to cite this article: Supe A. Graduate Medical Education Regulations 2019: Competency-driven contextual curriculum. Natl Med J India 2019;32:257-261 |
With modern medicine expanding its horizons, scientific data are becoming robust and voluminous information is available on various facets of medical practice. Technological advances have enabled medical ‘hands’ to reach the most intricate interior of the human body to aid diagnosis and therapeutics. The widespread use of internet and other media have enabled lay people to become more informed about what is happening to them. The commercialization of healthcare has resulted in increasing costs as well as a trust deficit between doctors and patients.
India’s national goal of ‘Health for All’ is guided by multiple factors—economic, sociocultural, literacy, political will and availability of healthcare service providers. At the centre of this scheme is the presence of a competent doctor with a caring attitude. Unlike in other professions, doctors must not only demonstrate a comprehensive knowledge of their subject but also retain a humane perspective in their conduct. They should know what is required in terms of ‘appropriate’ diagnostic tests and therapeutic measures. To reach this goal of a ‘balanced doctor’, who is both knowledgeable and humane, the first step is to redefine the curriculum of medical students at the undergraduate and postgraduate levels.
The Medical Council of India (MCI) is responsible for continuously assessing the needs, aspirations, quality and standards of medical education in India. One of their initiatives was to standardize the output of graduate medical education in the form of an ‘Indian Medical Graduate’ (IMG); a skilled, competent and motivated doctor with five intended roles as ‘Clinician, Leader, Communicator, Professional and Lifelong learner’ as per ‘Vision 2015’.[1] To achieve this, the MCI undertook a huge exercise of developing a competency-driven contextual curriculum over the past 5 years.
The MCI chose an expert-based approach for curricular change. The factors considered were: (i) the burden of diseases in India;[2] (ii) faculty and graduate perceptions about curricular deficiencies;[3] and (iii) students’ feedback and suggestions from social and health researchers. The revised World Federation of Medical Education basic guidelines[4] were used to make the IMG globally relevant. The MCI curricular reforms have systematically addressed these issues and developed strategies to make medical education more relevant for India in the changing context.
Medical education worldwide is shifting towards competency-based medical education (CBME). CBME emphasizes domains beyond medical knowledge and clinical skills, e.g. communication, professionalism and a focus on health systems. Usually, competency or outcome-based education involves all specialties put together and is better implemented in a problem-based education system.[5]
Competency-driven learning includes designing and implementing a medical education curriculum that focuses on predefined desired and observable abilities in real-life situations. Competency is an approach to preparing physicians for practice (i) oriented to the graduate’s abilities and (ii) organized around the requirement of capabilities based on societal and patient needs.[6],[7],[8] It de-emphasizes time-based training (tea bag approach)[9] and promises greater accountability, flexibility and learner-centredness. The MCI along with subject experts across India have prepared a list of competencies for every discipline.[10],[11],[12] An expert group has collated all of them to develop a final list of competencies and possible areas for integration.
Proposed curriculum
The new proposed curriculum signifies a paradigm shift in acquiring competencies, skill enhancement and attitude development among prospective medical graduates. It emphasizes the development of communication skills along with awareness of ethical issues in medical practice. It retains the total duration of the undergraduate Bachelor of Medicine and Bachelor of Surgery (MBBS) course of five-and-a-half years (including internship). However, the restructured course ensures that the student participates actively in the learning process and becomes competent clinically. A new feature of this curriculum is a foundation course[13] of 1 month at admission to introduce students to the profession of medicine. This will orient students to national health programmes, community service, medical ethics, health economics, learning and communication skills, life support measures, computer learning, sociology and demographics, biohazard safety and environmental issues. This course will provide an overview of the three core subjects of anatomy, physiology and biochemistry that are taught in first MBBS. Some key features of the new curriculum are:
- Integration:[14] horizontal and vertical—the new, innovative curriculum aims to facilitate horizontal and vertical integration among disciplines, bridging the gaps between theory and practice of medicine and between hospital-based medicine and community medicine.
- Early clinical exposure:[15] The purpose of introducing some aspects of clinical and social contexts of patient care in the first year is to provide a reference to basic science learning to reinforce comprehension of the normal and altered expression in disease states. Clinical training on communication and basic clinical skills will be imparted by the preclinical, paraclinical and clinical faculty.
- Student doctor method of clinical training: Learning through clerkship/student doctor method will involve participation of a student as a team member in patient care including in investigations, management and doing simple procedures.
- Electives: These will allow flexible learning options such as clinical electives, laboratory postings or community exposure (not usually a part of the regular curriculum). Students will be able to do projects and enhance self-directed learning, critical thinking and research abilities.
- Skill development and training: The new curriculum recommends the use of contemporary education technologies such as e-learning and simulation. Certification of skills would be necessary before licensure.
- Secondary hospital exposure: Emphasis will be on linking to the local health system including primary healthcare centres.
- Attitude, ethics and communication (AETCOM) module:[16] The AETCOM module is based on the principle that changing a person’s attitude can change his or her behaviour. The cognitive components of attitudes are fundamental and constant over time. Behavioural attitudes are manifestations of underlying cognitive and affective attitudes. Ethical dimensions play a crucial role in behavioural evolution, and the basic building block of good communication is the feeling that every human being is unique and of value.
The MCI has prepared revised regulations on graduate medical education and competency-driven contextual undergraduate curriculum, accompanied by guidelines for its implementation. As the traditional undergraduate curriculum in India is discipline-based, for feasibility and practical implementation, the proposed competency-driven approach retains the existing discipline-based format with horizontal and vertical integration. At the preclinical and paraclinical level, the foundational sub-competencies will converge to attain the desired clinical competencies [Table - 1].
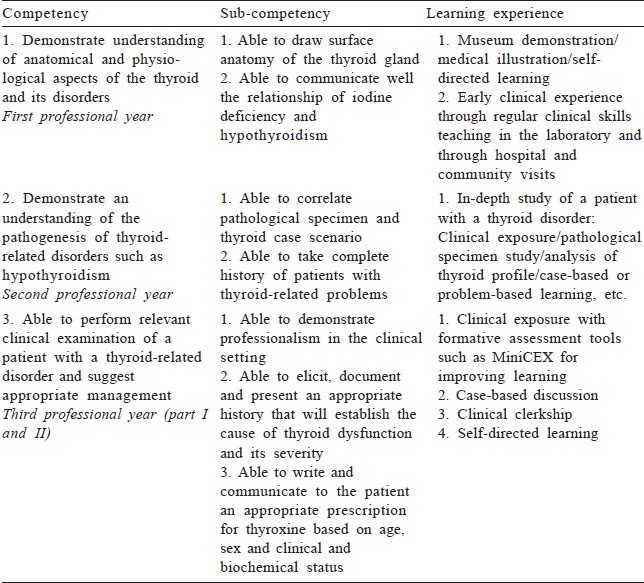
Teaching of CBME would need framing of entrustable professional abilities (EPA) along with milestones for a particular symptom or disease. EPAs are drawn from the needs of society. For example, if prevention of malaria is a need then along with diagnosis and treatment, EPAs on prevention need to be framed. The teaching and assessment method would be designed around the EPAs.[16] Though the new curriculum does not have EPAs, a comprehensive list of competencies and sub-competencies [Figure - 1] can suffice at this stage to bring the change. Over the years, EPAs and milestones need to be developed in India as per contextual needs.
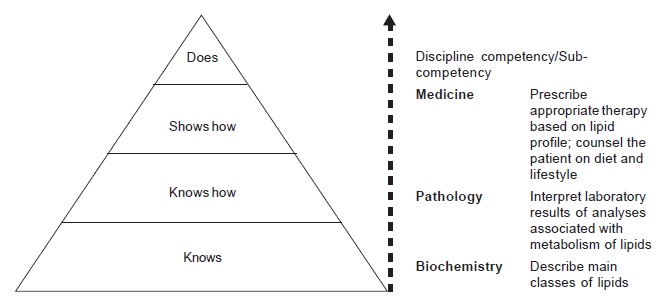 |
| Figure 1: Ascendency of competence—lipid profile abnormalities |
A module for assessment[17] for the new curriculum has also been prepared, which would facilitate universities and colleges to develop their assessment plans within a prescribed framework.
Challenges in implementation
Implementing such a curriculum across 532 medical schools with 76 876 seats[18] in India is a major challenge. It cannot be achieved without extensive faculty development, efficient management, intensive monitoring and evaluation of the programme.
Earlier experience with implementation of curricular changes suggests that a professionally managed, sustainable approach is necessary for effective implementation. For faculty development the MCI has established a functional network of 12 regional and 10 nodal centres[19] across the country. These centres have been successfully running courses in medical education for the past 10 years. Over 43 000 faculty members have been trained through the basic and revised basic courses and over 900 teachers have been trained through the advanced course in medical education.
In terms of regulation, it was recognized that every medical college needs to develop a capacity to adapt to the requirements of the new guidelines. The MCI mandated each medical college to establish a curriculum committee for implementation and monitoring of the competency-driven contextual curriculum. For the past 3 years, it also revised the format of its existing faculty development programme to orient it towards preparing faculty for implementation of the competency-driven curriculum. An AETCOM forms a part of this new faculty development curriculum.[20] Each member of the curriculum committee is required to undergo this training as they will lead the change and implement the competency-driven curriculum. This capacity building work is in progress at present. Latest articles on CBME in Indian journals indicate rolling out of a competency-driven curriculum for medical undergraduates in the near future.[21],[22],[23]
Implementation at the institutional level: Expected challenges and possible solutions
Curricular implementation needs involvement and efforts of institutions and teachers. Both the stakeholders need to keep the outcomes/goals in mind with an emphasis on skills and performance than on acquisition of knowledge alone. There is a need for intensive monitoring by the curricular committee. Institutions and policy-makers must be clear that implementation will be gradual requiring a long-term commitment of time and resources for evaluation and continuous improvement in the guidelines.
Implementing the new curriculum will involve considerable new learning and some unlearning for those teachers who will reorient the curriculum. Further, teaching other faculty and preparing them for implementation will be an added responsibility. The skills required, besides those related to the CBME approach, include ability to work together, willingness for change and ability to negotiate resistance. Faculty requires considerable leadership skills to navigate the complexities of the entire process, including time and resource constraints. The MCI successfully completed the Curriculum Implementation Support Programme from January to September 2019 through faculty development network for training of more than 10 000 faculty members.
Assessment approaches and methodologies with clinical relevance also require an enormous scale of curricular restructuring. Lastly, the new curriculum needs to be evaluated for its overall effectiveness over the next 5–10 years. The new assessment module will facilitate universities and colleges to prepare a plan to overcome the challenge of multiple-choice questions, which are the basis of entrance examinations for postgraduate courses.
Conclusion
Medical education in India is on the threshold of a major change. The competency-driven curriculum developed by the MCI has the potential to address the deficiencies that have arisen in the training of health professionals in the Indian context. The new curriculum emphasizes skill enhancement and development of attitudes, ethics and communication skills to make the future IMG more competent and humane. The proposed National Medical Commission[24] should adopt this well-designed contextual curriculum to bridge the gaps in the medical curriculum. A well-planned implementation strategy at the institutional level, faculty development and intensive monitoring by all stakeholders will ensure improvement in the much-needed educational outcomes and thereby have a positive impact on healthcare in India.
Acknowledgements
I am grateful to the Board of Governors of the MCI and Dr Rajlakshmi, Academic Consultant, MCI and all members of the expert group for their support.
Conflicts of interest. I continue to be convener of the expert group of the Board of Governors of the MCI.
| 1. | Available at https://old.mciindia.org/tools/announcement/MCI_booklet.pdf (accessed on 15 Aug 2019). [Google Scholar] |
| 2. | WHO. The global burden of disease. 2004 update. Available at www.who.int/healthinfo/global_burden_disease/ GBD_report_2004update_full.pdf (accessed on 15 Aug 2019). [Google Scholar] |
| 3. | Supe A, Rege N. Medical curricula. Faculty and graduate perceptions. Indian Pract 2000;53:593-8. [Google Scholar] |
| 4. | World Federation of Medical Education. Basic medical education. Available at http://wfme.org/standards/ bme/ (accessed on 15 Aug 2019). [Google Scholar] |
| 5. | Frank JR, Mungroo R, Ahmad Y, Wang M, De Rossi S, Horsley T. Toward a definition of competency-based education in medicine: A systematic review of published definitions. Med Teach 2010;32:631-7. [Google Scholar] |
| 6. | Frank JR, Snell LS, Cate OT, Holmboe ES, Carraccio C, Swing SR, et al. Competency-based medical education: Theory to practice. Med Teach 2010;32:638-45. [Google Scholar] |
| 7. | Gruppen LD, Mangrulkar RS, Kolars JC. The promise of competency-based education in the health professions for improving global health. Hum Resour Health 2012;10:43. [Google Scholar] |
| 8. | Snell LS, Frank JR. Competencies, the tea bag model, and the end of time. Med Teach 2010;32:629-30. [Google Scholar] |
| 9. | Medical Council of India. Competency based undergraduate curriculum for the Indian medical graduate. Volume-I (2018). Available at www.mciindia.org/CMS/wp-content/uploads/2019/01/UG-Curriculum-Vol-II.pdf (accessed on 21 Oct 2019). [Google Scholar] |
| 10. | Medical Council of India. Competency based undergraduate curriculum for the Indian medical graduate. Volume-II (2018). Available at www.mciindia.org/CMS/wp-content/uploads/2019/01/UG-Curriculum-Vol-ILpdf (accessed on 21 Oct 2019). [Google Scholar] |
| 11. | Medical Council of India. Competency based undergraduate curriculum for the Indian medical graduate. Volume-III (2018). Available at www.mciindia.org/CMS/wp-content/uploads/2019/01/UG-Curriculum-Vol-III.pdf (accessed on 21 Oct 2019). [Google Scholar] |
| 12. | Ten Cate O. Nuts and bolts of entrustable professional activities. J Grad Med Educ 2013;5:157-8. [Google Scholar] |
| 13. | Medical Council of India. Available at https://mciindia.org/CMS/wp-content/uploads/2019/10/ Module_Competence_based_02.09.2019pdf (accessed on 21 Oct 2019). [Google Scholar] |
| 14. | Medical Council of India. College and course search. Available at www.mciindia.org/CMS/information-desk/ college-and-course-search (accessed on 21 Oct 2019). [Google Scholar] |
| 15. | Available at https://old.mciindia.org/InformationDesk/ForColleges/NationalFacultyDevelopment Programme.aspx (accessed on 15 Aug 2019). [Google Scholar] |
| 16. | Medical Council of India. Competency based undergraduate curriculum for the Indian medical graduate. Module 1. Foundation course. Available at www.mciindia.org/CMS/wp-content/uploads/2019/08/foundation-new_compressed.pdf (accessed on 21 Oct 2019). [Google Scholar] |
| 17. | Medical Council of India. Competency based undergraduate curriculum for the Indian medical graduate. Module 4. Alignment and integration. Available at www.mciindia.org/CMS/wp-content/uploads/2019/10/Alignment-and-Integration_03.10.2019.pdf (accessed on 21 Oct 2019). [Google Scholar] |
| 18. | Medical Council of India. Competency based undergraduate curriculum for the Indian medical graduate. Module 2. Early clinical exposure. Available at www.mciindia.org/CMS/wp-content/uploads/2019/08/early-new_compressed.pdf (accessed on 21 Oct 2019). [Google Scholar] |
| 19. | Medical Council of India. AETCOM. Attitude, ethics and communication. Available at www.mciindia.org/CMS/wp-content/uploads/2019/01/AETCOM_book.pdf (accessed on 21 Oct 2019). [Google Scholar] |
| 20. | Medical Council of India. Program of the revised basic course workshop. Available at www.mciindia.org/ documents/informationDesk/8.%20Three%20day%20revised%20BCW%20programme.pdf (accessed on 15 Aug 2019). [Google Scholar] |
| 21. | Modi JN, Gupta P, Singh T. Competency-based medical education, entrustment and assessment. Indian Pediatr 2015;52:413-20. [Google Scholar] |
| 22. | Chacko TV. Moving toward competency-based education: Challenges and the way forward. Arch Med Health Sci 2014;2:247-53. [Google Scholar] |
| 23. | Ananthakrishnan N. Competency based undergraduate curriculum for the Indian Medical Graduate, the new MCI curricular document: Positives and areas of concern. J Basic Clin Appl Health Sci 2018;2:182-90. [Google Scholar] |
| 24. | President gives assent to National Medical Commission Bill. Available at www.indiatoday.in/india/story/president-gives-assent-to-national-medical-commission-bill-1578801-2019-08-08 (accessed on 15 Aug 2019). [Google Scholar] |
Fulltext Views
10,554
PDF downloads
1,475




