Translate this page into:
Inclusion of physical medicine and rehabilitation in the medical curriculum: A step in the right direction
1201,Penthouse Drive, Mpuntainside Apartments, Birmingham, Alabama 35202, USA; nehakaudan@gmail.com
[To cite: Singh N. Inclusion of physical medicine and rehabilitation in the medical curriculum: A step in the right direction. Natl Med J India 2023;36:44–8. DOI: 10.25259/NMJI_704_21]
Abstract
Background
Although physical medicine and rehabilitation (PMR) was first introduced in India in the 1960s, it was not until the 1990s when it was offered as an optional rotation to Indian medical graduates. Lately, with the introduction of a competency-based undergraduate curriculum in 2018, PMR has been included as an essential subject in the medical graduate curriculum, to be implemented from 2019. We aimed to ascertain the importance of incorporating PMR in the medical graduate curriculum while also discussing the awareness about PMR among Indian healthcare professionals.
Methods
We drafted an online questionnaire-based survey and sent that to participants through cloud-based software. Responses were collected over a period of 4 weeks and a descriptive analysis was performed.
Results
The initial hypothesis was that most healthcare professionals would be unaware of the scope of PMR as a medical specialty. The results of this study did not support our hypothesis with 96.8% of the participants being familiar with PMR as a medical specialty. In addition, 85% of the participants reported being introduced to PMR either in their medical school or during their residency training and 92% of the participants appreciated the late integration of PMR within the medical graduate curriculum.
Conclusions
Introduction of medical graduates to PMR would help in bridging the gaps faced by people with disabilities in accessing healthcare facilities. It would also help clinicians from other specialties to collaborate with physiatrists in a more coordinated manner.
INTRODUCTION
Physical medicine and rehabilitation (PMR), also known as physiatry or rehabilitation medicine, aims to enhance and restore functional ability and quality of life of people with physical impairments or disabilities. A physician having completed training in this field is referred to as a physiatrist. Unlike other medical specialties that focus on a medical ‘cure’, the goals of the physiatrist are to maximize patients’ independence in activities of daily living and improve quality of life. Physiatrists are experts in designing comprehensive, patient-centred treatment plans and are integral members of the care team. The medical specialty of PMR was first introduced in India in the early 1960s1 and since then, it has been expanding steadily, although at a slower pace compared to other fields of medical specialization. Although PMR was recognized as an optional rotation for undergraduate medical students in the 1990s, it was only in the 2018 that the Medical Council of India included it as an essential subject in the Bachelor of Medicine and Bachelor of Surgery (MBBS) curriculum, which was implemented from August 2019.2
There are misconceptions about the medical specialty of PMR among Indian healthcare professionals, which impede the overall management of people with disabilities. The prevalence of disability in India stands at 2.2% (National Sample Survey, July–December 2018),3 which presents an already stressed Indian healthcare system with an enormous challenge of providing access to health for all.4 Improving the level of familiarity of physicians with PMR would not only facilitate the provision of rehabilitative health service to this subset of patients but also enhance their quality of life through a more comprehensive approach to their problems.5
We designed this study to reflect upon the inclusion of PMR in the Indian medical graduate curriculum and to delineate awareness of different areas of PMR practice among healthcare professionals. We did this survey on already licensed practitioners to understand their viewpoint so that more robust and conclusive measures could be undertaken to increase awareness about PMR among medical students and physicians in the near future. Our hypothesis was that most healthcare professionals would be hesitant about the late expansion of the medical curriculum. A literature search failed to reveal any study discussing the late integration of PMR or illustrating its awareness among Indian healthcare professionals.
METHODS
We conducted this observational study based on a questionnaire over a period of 4 weeks from January 2021 to February 2021. The survey had 10 questions, which focused on the familiarity of healthcare professionals with the medical branch of PMR and also about their views on the late integration of PMR in the curriculum of MBBS graduates (Table I). The cohort of participants was recruited with the help of social media (Facebook, WhatsApp). An introductory message explaining the research project was shared through the social media accounts of the author. All the participants who gave their consent were then sent the survey through an online, cloud- based software (SurveyMonkey Inc.).6 Care was taken not to include any physiatrist. The survey used a combination of fixed and open responses. Upon completion of each survey, data were automatically uploaded to the software. Responses were gathered anonymously with no acquisition of any personal details (name, gender, age, hospital where they worked, state, designation and year of graduation). A descriptive analysis was conducted on the survey data.
| Question | Responses | n (%) | |
|---|---|---|---|
| 1. What is your highest medical qualification? | Medical graduate | 2 | (3.1) |
| Postgraduate | 49 | (76.6) | |
| Fellow | 13 | (20.3) | |
| 2. What is the department/specialty where you work? | Clinical | 54 | (84.4) |
| Paraclinical | 10 | (15.6) | |
| 3. Have you heard about PMR as a medical postgraduate specialty? | Yes | 62 | (96.9) |
| No | 2 | (3.1) | |
| 4. Do you have a department of PMR in your hospital? | Yes | 29 | (45.3) |
| No | 35 | (54.7) | |
| 5. What do we call a medical doctor with MD in PMR? | Medical doctor | 37 | (57.8) |
| Physiatrist | 15 | (23.4) | |
| Physiotherapist | 4 | (6.3) | |
| Do not know | 8 | (12.5) | |
| 6. What is the source of your knowledge about PMR as a medical specialty? | Medical school | 38 | (59.4) |
| Residency training | 15 | (23.4) | |
| Medical studies | 1 | (1.6) | |
| Medical conferences | 1 | (1.6) | |
| Mass media, self-training, others | 0 | ||
| Colleagues | 9 | (14.1) | |
| 7. Are you aware of the following diagnostic/invasive/advanced interventions | Skull traction | 15 | (23.4) |
| being provided by a PMR doctor? | Peri-articular and intra-articular injections | 36 | (56.3) |
| Nerve blocks | 34 | (53.1) | |
| Botulinum toxin injections | 29 | (45.3) | |
| Platelet-rich plasma injections | 23 | (35.9) | |
| Ultrasound/image-guided injections | 30 | (46.9) | |
| EMG, NCV and other electrodiagnostic tests | 27 | (42.2) | |
| Musculoskeletal ultrasound | 23 | (35.9) | |
| Urodynamic evaluations | 10 | (15.6) | |
| Instrumental gait analysis | 21 | (32.8) | |
| Corrective surgical procedures for | 28 | (43.8) | |
| musculoskeletal problems | |||
| Cystoscopy in neurogenic bladder | 8 | (12.5) | |
| Neuroprosthetic implants | 17 | (26.6) | |
| None of the above | 10 | (15.6) | |
| 8. Have you ever referred your patient to a PMR doctor? | Yes | 44 | (68.8) |
| No | 20 | (31.3) | |
| 9. What are your reasons for referral to a PMR doctor? | Therapeutic exercises | 26 | (40.6) |
| Physical modalities | 19 | (29.7) | |
| Electrodiagnostic studies | 8 | (12.5) | |
| Orthosis/prosthesis prescription | 17 | (26.6) | |
| Pain management | 33 | (51.6) | |
| Rehabilitation of CNS disorders | 27 | (42.2) | |
| Diagnosis and rehabilitation of myopathies– | 21 | (32.8) | |
| neuropathies | |||
| Prevention, diagnosis and treatment of musculoskeletal and rheumatic disorders | 15 (23.4) | ||
| Geriatric rehabilitation | 16 | (25.0) | |
| Cardiopulmonary rehabilitation | 7 | (10.9) | |
| Never referred | 20 | (31.3) | |
| 10. Do you believe that the late inclusion of PMR in MBBS curriculum would | Yes | 59 | (92.2) |
| help in changing the overall perception of healthcare professionals | No | 2 | (3.1) |
| towards PMR? | Cannot say | 3 | (4.7) |
PMR physical medicine and rehabilitation EMG electromyography NCV nerve conduction velocity CNS central nervous system MBBS Bachelor of Medicine and Bachelor of Surgery MD Doctor of Medicine
RESULTS
The survey was sent to 120 healthcare professionals working in different medical specialties, of which only 64 participants (53.3%) responded. Surveys with incomplete responses (n=3, 2.5%) were not included in the analysis. The distribution of participants from different medical specialties is shown in Fig. 1. The responses of participants to the questions asked in the survey are given in Table I.
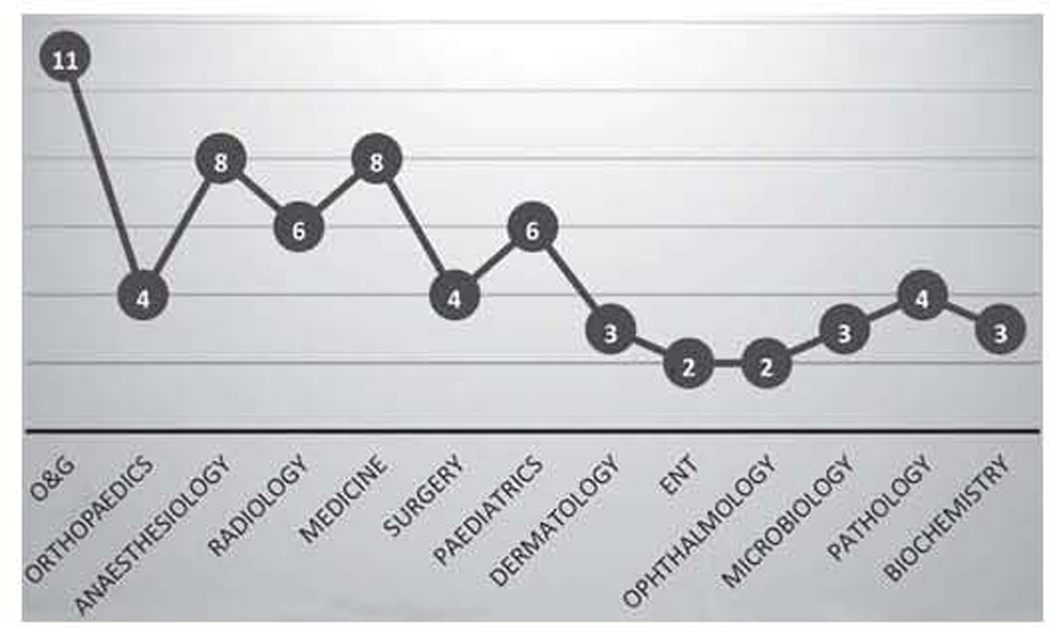
- Distribution of participants from different medical specialties
- O&G obstetrics and gynaecology ENT ear, nose and throat
Question 1–2
Preliminary information was collected to enquire about their highest medical qualification. Two of the participants had started their clinical practice soon after graduation and reported MBBS as their highest medical qualification. A majority of the participants (n=49, 76.6%) had completed some postgraduate training (Diplomate of National Board, Doctor of Medicine, Master of Surgery and Diploma) within their respective fields. Almost one-fifth of the participants reported acquisition of advanced medical training subsequent to their postgraduate training (n=13, 20.3%). The number of participants from clinical specialties (n=54, 84.4%) outnumbered the participants from paraclinical medical specialties (n=10, 15.6%).
Question 3–6
Upon asking the participants if they recognized PMR as a medical specialty, almost 97% of them answered in the affirmative. However, only less than half of the participants had a PMR department in the hospitals where they worked. Though 62 (96.9%) participants could identify PMR as a medical postgraduate specialty, not many could identify the term used to describe a doctor with training in PMR. Only 15 (23.4%) participants were aware that a doctor with training in PMR is called a physiatrist. A worrying observation was the inability to ascertain the difference between a physiatrist and a physiotherapist by 4 (6.3%) participants. Further, when asked about the source of their knowledge about PMR, a majority (n=38, 59.4%) mentioned being introduced to PMR in their medical schools, while a quarter of the participants (n=15, 23.4%) had exposure during their residency training. Few participants (n=9, 14.1%) were made aware of PMR through their colleagues, while some were introduced to it through medical studies (n=1, 1.6%) and medical conferences (n=1, 1.6%).
Question 7
The participants were further asked if they were aware of any diagnostic or interventional procedure being performed by physiatrists on a regular basis. They were asked to mark all the procedures they were aware of and not necessarily choose one option. Multiple procedures ranging from skull traction to nerve blocks, image-guided injections and corrective surgical procedures, etc., were listed in the survey. Most of the participants (n=36, 56.3%) recognized the use of peri-articular and intra-articular injections by a physiatrist followed by the use of nerve blocks (n=34, 53.1%). The other most commonly identified interventions were ultrasound or image-guided injections (n=30, 46.9%) and administration of botulinum toxin injections (n=29, 45.3%). The least known interventions were cystoscopy in neurogenic bladder (n=8, 12.5%) and urodynamic evaluations (n=10, 15.6%). A few participants (n=10; 15.6%) were of the opinion that no diagnostic or advanced interventional procedure is being performed by a physiatrist.
Question 8–10
Since PMR as a medical specialty focuses on comprehensive rehabilitation and optimization of the functional ability of a patient, we felt prudent to ask the participants about their referral practices of transferring a patient to a physiatrist. Most of the referrals were for pain management (n=33, 51.6%) followed by rehabilitation for disorders of the central nervous system (CNS) (n=27, 42.2%) and therapeutic exercises (n=26, 40.6%). The domains with least referrals were identified as cardio- pulmonary rehabilitation (n=7, 10.9%) and electrodiagnostic studies (n=8, 12.5%). Almost a third of the participants had never referred their patients to a physiatrist. Noticeably, when asked to opine if the late inclusion of PMR in MBBS curriculum would help to change the overall perception of healthcare professionals towards PMR, an overwhelming majority of participants (n=59; 92.2%) answered in the affirmative.
DISCUSSION
PMR is an independent clinical branch of medicine that emphasizes the prevention and treatment of disorders, especially of the neuromusculoskeletal, cardiovascular or pulmonary aetiology, at any age, acquired or congenital, that may produce temporary or permanent activity limitation, disability or participation restriction in society including loss of quality of life.7 It follows the WHO International Classification of Functioning, Disability and Health and is involved with the prevention and reduction of disability and handicap arising out of physical impairments along with the provision of medical management of disability from a physical, psychological and vocational point of view.7 The 76th round of NSS (July– December 2018) concluded that the overall prevalence of disability in India was 2.2% with 2.3% in rural and 2.0% in urban areas.3 In a population of 1.353 billion (2018), a disability prevalence of 2.2% translates to approximately 30 million people with a disabling illness. In 2017, WHO launched the ‘Rehabilitation 2030’ initiative to draw attention to the profound unmet need for rehabilitation worldwide and highlight the importance of strengthening of health systems to improve rehabilitative services. Further, the ‘WHO Rehabilitation Need Estimator tool’ estimated that by 2019, approximately 2 in 7 people could benefit from rehabilitation in the South-East Asia Region with the highest need in India, where 410 million people could benefit from rehabilitation. Furthermore, there has been an 86.9% increase in years lived with disability between 1990 and 2019.8 With such a huge proportion of Indian population being in dire need of rehabilitative services, it seems that the late inclusion of PMR in graduate medical training is a step taken in the right direction. The latest Indian undergraduate curriculum follows Harden’s ladder of integration and suggests that integration should not exceed 20% of the total curriculum at recommended levels. Thereby, the clinical branch of PMR has been included in graduate training with 43 lists of objectives and 41 total integrations.2
The results of our study did not agree with the initial hypothesis. It was hypothesized that most of the healthcare professionals would be unaware of the scope of PMR as a medical specialty, but an overwhelming 96.9% (62) of the study participants recognized PMR as a postgraduate medical specialty. Notably, they were also of the opinion that the inclusion of PMR in the MBBS curriculum would help in dispelling confusion regarding the specialty and further help in familiarization of healthcare professionals with the entire continuum of its scope. It should be noted that approximately 60% of the participants were introduced to PMR in their medical schools which in turn reflects that the late inclusion of PMR would facilitate better coordination among health services. On a similar note, health experts from various countries in central Europe are also advocating for inclusion of PMR or rehabilitation medicine or physiatry in graduate medical training as the need of the hour.9 It has been successfully integrated as an essential component of medical training in various developed nations such as Australia, Belgium, Canada, France, Germany, Spain, Sweden, the UK and the USA.10
The most recognized procedures of PMR in our study were injections (intra-articular, peri-articular and ultrasound-guided) and the least recognized were urodynamic evaluations and cystoscopy. Almost two-thirds of the study participants said that they had referred their patients to a physiatrist, depending upon the circumstances. However, most of the referrals were for pain management, rehabilitation for CNS disorders and therapeutic exercises. Over the years, pain management has expanded to include interventional procedures in addition to pharmacological and non-pharmacological measures. This could be a plausible explanation for the injections and nerve blocks being among the most recognizable interventions of PMR and one of the most common causes for patient referral. Similar observations were made by Raeissadat et al. where the most recognized areas of PMR involved CNS disorders and the most common reason for referral was for therapeutic exercises.5 For the other domains of PMR, with the least recognition such as urodynamic evaluations or electrodiagnostic studies or cardiovascular rehabilitation, the low familiarity of healthcare professionals with the scope of PMR could have contributed to this observation. Collaboration of physiatrists with healthcare professionals of different medical specialties should, therefore, be encouraged so that optimum utilization of healthcare services could be facilitated seamlessly.
Almost 60% of participants in our study mentioned an introduction to PMR in their medical schools. Analogous observations have been made by Vlak et al. who observed that the introduction of PMR in undergraduate medical training promotes the acquisition of medical acumen necessary to manage persons with disabilities while contributing significantly to the general medical education obtained by clinicians.11 Similarly, Raeissadat et al. also concluded that familiarization of medical students with the field of PMR has a positive impact on their present, and likely their future association and attitude towards this specialty.5 It is worth mentioning that physicians with no introduction to PMR during their training, have been found to have incomplete knowledge about disability, inability to assess disability and lack of experience in overcoming disability as well as lack of awareness of the possibilities of PMR as a medical specialty.9,12,13 Further, as any patient may require rehabilitation, it is required that all physicians should be familiar with at least a basic knowledge of rehabilitation, while recognizing the importance of timely transfer of a patient to a physiatrist. It is thus important that PMR be taught in all undergraduate medical faculties.14
Limitations
One of the limitations of this study was the small number of study participants. In addition, by the virtue of selection of study participants by the author’s social media accounts, there exists a selection bias in this study. It is to be noted that by default the participants of the study were aware of PMR as a medical specialty, as the author is a practising physiatrist. An extensive application of such surveys is, therefore, desirable to make a more reliable assumption about awareness and attitude of Indian healthcare professionals towards the clinical branch of PMR. Another limitation was that this study should have been supplemented by a suggested follow-up survey of the participants with negative PMR consultation responses to ascertain their reasons for the same. An insight into those reasons would further guide us in facilitating a collaboration between physiatrists and other healthcare professionals from different medical specialties. Furthermore, no conclusions about PMR awareness were on the basis of the participant being from clinical or paraclinical specialty. Doctors from clinical specialties would have a higher likelihood of collaborating with physiatrists than doctors from paraclinical specialties.
Conclusions
The results of our study suggest that healthcare professionals from different medical specialties have different levels of familiarity with and willingness to consult with physiatrists throughout the various areas of PMR practice. Introduction of medical students to the field of PMR is thus an important factor in creating awareness about this medical specialty. It seems especially important for those medical schools and hospitals with academic PMR departments to reach out to other schools that lack academic PMR programmes, as this may be the primary method by which their students gain exposure to this evolving field. We believe that a knowledge of the field of PMR could be valuable for all medical students and their future patients. With a better understanding of the field of PMR, even physicians from other specialties would be able to better utilize the PMR services for their patients.
We also suggest that similar surveys be conducted among healthcare professionals from different parts of the country to allow pooling of data for further analysis. Further efforts should be targeted towards increasing the number of PMR residency programmes, putting PMR rotations in the undergraduate and residency curriculums, improving the collaboration with other departments by offering short-term PMR tours or more actively participating in medical conferences and other scientific meetings. Our study shows that doctors’ familiarity with the various areas of PMR practice is increased by training in hospitals and medical schools that include a department of PMR. This is important because current medical students are the specialists of the future. Finally, we hope that the results of this study would lead to a better understanding of the field of PMR and utilization of resources to introduce this specialty to other physicians and, ultimately, improve care for patients with disabilities.
Conflicts of interest
There are no conflicts of interest.
References
- Dr Mary Verghese: Wheelchair surgeon and pioneer of physical medicine and rehabilitation in India. Curr Med Issues. 2017;15:148-52.
- [CrossRef] [Google Scholar]
- Medical Council of India 2018. Medical Council of India. Available at www.mciindia.org/CMS/information-desk/for-colleges/ug-curriculum (accessed on 22 Feb 2021)
- [Google Scholar]
- NSS Report No. 583: Persons with disabilities in India NSS 76th Round (July-December 2018) Available at https://pib.gov.in/Pressreleaseshare.aspx?PRID=1593253 (accessed on 5 Mar 2021)
- [Google Scholar]
- SRS Statistical Report, 2016. 2016. Office of the Registrar General and Census Commissioner. India: Ministry of Home Affairs, Government of India; Ministry of Home Affairs, Government of India. Available at https://censusindia.gov.in/vital_statistics/SRS_Reports__2016.html (accessed on 7 Mar 2021)
- [Google Scholar]
- Survey of medical residents' attitude toward physical medicine and rehabilitation. Am J Phys Med Rehabil. 2014;93:540-7.
- [CrossRef] [PubMed] [Google Scholar]
- Competency Based Training in Physical Medicine and Rehabilitation. Available at https://nbe.edu.in/mainpdf/curriculum/Physical-medicine-rehabilitation.pdf (accessed on 5 Apr 2021)
- [Google Scholar]
- World Health Organization. Available at www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions (accessed on 2 Apr 2021)
- [Google Scholar]
- What medical doctors and medical students know about physical medicine and rehabilitation: A survey from Central Europe. Eur J Phys Rehabil Med. 2016;52:597-605.
- [Google Scholar]
- Educational objectives in the new interdisciplinary subject 'Rehabilitation, Physical Medicine, Naturopathic Techniques' under the 9th Revision of the Licensing Regulations for Doctors-consensus recommendations of the German Society for Rehabilitative Sciences and the German Society for Physical Medicine and Rehabilitation. Rehabilitation (Stuttg). 2004;43:337-47.
- [CrossRef] [PubMed] [Google Scholar]
- Teaching disability and rehabilitation medicine at the medical school in Split, Croatia. Croat Med J. 2004;45:99-102.
- [Google Scholar]
- Teaching medical students rehabilitation medicine. Disabil Rehabil. 2010;32:1948-54.
- [CrossRef] [PubMed] [Google Scholar]
- Survey of general practitioners' attitudes toward physical medicine and rehabilitation. Int J Rehabil Res. 2006;29:167-70.
- [CrossRef] [PubMed] [Google Scholar]
- Hannover model for the implementation of physical and rehabilitation medicine teaching in undergraduate medical training. J Rehabil Med. 2010;42:206-13.
- [CrossRef] [PubMed] [Google Scholar]




