Translate this page into:
Is tobacco use increasing among medical students of Bengaluru city, India? Evidence from two cross-sectional studies
Corresponding Author:
Prem K Mony
Division of Epidemiology and Population Health, St John's Medical College and Research Institute, 100 Feet Road, Koramangala, Bengaluru 560034, Karnataka
India
prem_mony@sjri.res.in
| How to cite this article: Mony PK. Is tobacco use increasing among medical students of Bengaluru city, India? Evidence from two cross-sectional studies. Natl Med J India 2016;29:274-276 |
Abstract
Background. Studies investigating secular changes in tobacco use are rare in India. We estimated self-reported prevalence of tobacco use, across a 5-year interval, among medical students in Bengaluru, India.Methods. We did two cross-sectional studies during 2007 and 2013 among third year undergraduate medical students of four medical colleges in Bengaluru. A self-administered questionnaire was used to elicit information on tobacco smoking and chewing.
Results. The participation rates were 82% (323/395) in 2007 and 78% (253/324) in 2013 (p=0.2). Among males, there was no statistically significant change in prevalence of current smoking (3.5% [6/172] in 2007 to 8.9% [12/135] in 2013 [p=0.053]); experimental use of tobacco had however increased from 24% (41/172) in 2007 to 42% (56/135) in 2013 (p=0.001). Similarly among females, experimental use was reported by 3.3% (5/151) in 2007 and 11.2% (13/116) in 2013 (p=0.01). Current smoking among female students was <1 % in both the study years. Reported current chewing levels remained unchanged among males, 1.8% (2/171) and 3.7% (5/135) (p=0.2) and fell from 4% (6/146) in 2007 to 0% in 2013 among females (p=0.04).
Conclusion. There was no increase in current smoking or chewing of tobacco but there was an increase in experimental smoking among male and female medical students in this southern Indian city. Schools and colleges must include tobacco control education in their curriculum.
Introduction
Globally, behaviours and lifestyles are in a state of flux and tobacco companies are shifting their focus to newer markets and products (such as e-cigarettes). [1] It is expected that increasing numbers of youth will begin to use tobacco products and that young women will also be encouraged to smoke. This is likely to alter the epidemiology of tobacco use in countries such as India currently characterized by a preponderance of smokeless tobacco use and beedi smoking rather than cigarette smoking as also predominant tobacco use during middle-age (late 40s) among adult males rather than in young adulthood (20s to 30s) as seen in industrialized countries. [2] Among youth, tobacco use among medical students is a key indicator of tobacco control activities in a country or region. It is therefore important to track tobacco use among medical students over time given their role as future doctors in tobacco cessation counselling and advocacy for stronger tobacco control policies. We estimated the self-reported prevalence of tobacco use, across a 5-year interval, among medical students of a southern Indian city.
Methods
Study setting and population
The studies were undertaken in Bengaluru, a metropolitan city in southern India. [3] The demographic characteristics of the city are: population 8.4 million, literacy rate 90% and sex-ratio 914 females per 1000 males. [4] The studies were conducted in four medical colleges (one government and three private). All third year (6th term) students were the eligible population. [5]
Study design, instrument and data collection
Two cross-sectional studies were done: the first survey was in 2007 [6] and the second in 2013. A self-administered questionnaire was used to obtain information on tobacco smoking and chewing as per the Global Health Professionals Study (GHPS) methodology. [5] Ethical approval was obtained from the Institutional Review Board of St John′s Medical College, Bengaluru. Permission to conduct the study was obtained from the heads of the four participating institutions. Written informed consent was obtained from the participating students. Questionnaires were distributed to the students in a classroom setting and collected after completion; anonymity was respected.
Study definitions and analysis
Definitions of tobacco use status were based on self-reported smoking of cigarettes/beedis and chewing of tobacco. Never-users were defined as persons who had never smoked or chewed tobacco even once in their life-time; experimental users were defined as those who had smoked or chewed tobacco once or twice but never regularly; current users were defined as those who had smoked or chewed tobacco in the last 30 days preceding the survey, either occasionally (at least once a week) or daily (at least once per day). [6] Data were entered and analysed using SPSS 21.0. Simple descriptive analysis was done for the variables of interest; a p value <0.05 was considered significant.
Results
The participation rates were 82% (323/395) in 2007 and 78% (253/324) in 2013 (p=0.2). In different colleges it ranged from 61% to 95% in 2007 and from 72% to 95% in 2013. The proportion of students from the government college was 40% in 2007 and 23% in 2013 (p<0.001). Male students comprised 54% of all participants in both surveys. Among males, experimental use of tobacco was reported by 24% (41/172) in 2007 and 42% (56/135) in 2013; this difference was statistically significant (p=0.001; [Figure - 1]). This appeared to be driven predominantly by a significant change in the private sector (24% v. 43% [p=0.01]) and a non-significant change in the government sector (23% v. 38% [p=0.1]). Current smoking increased from 3.5% (6/172) in 2007 to 8.9% (12/135) in 2013 (p=0.05); the maximum prevalence in a college was 16% in 2007 and 22% in 2013. There was no difference by type of college: change in government sector (1.1% v. 2.5% [p=0.5]) and change in private sector (6% v. 15.6% [p=0.2]). Daily smoking was reported by 1.7% in 2007 and 3.7% in 2013 (p=0.3).
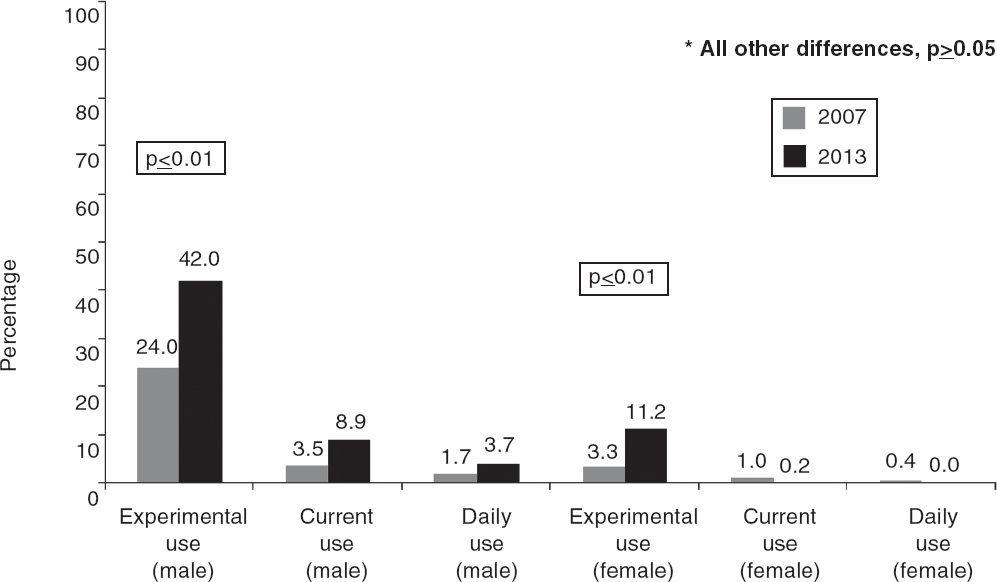 |
| Fgure 1. Changes in prevalence of reported smoking among male and female medical students in Bengaluru in 2007 and 2013 |
Among females, experimental use was reported by 3.3% (5/151) in 2007 and 11.2% (13/116) in 2013; this difference was statistically significant (p=0.01). There was no difference by type of college: change in government sector (2.2% v. 5.6% [p=0.5]) and change in private sector (5% v. 12.2% [p=0.08]). Current smoking was reported by ≤1% of female students in both the surveys.
Among males, current chewing habit was reported by 1.8% (2/171) and 3.7% (5/135) in the two years, respectively. Mixed users (smoking and chewing) were 1.2% in 2007 and 2.2% in 2013. None of these differences were statistically significant. Among females, current chewing was reported by 4% (6/146) in 2007 and by 0% in 2013 (p=0.04, [Figure - 2]).
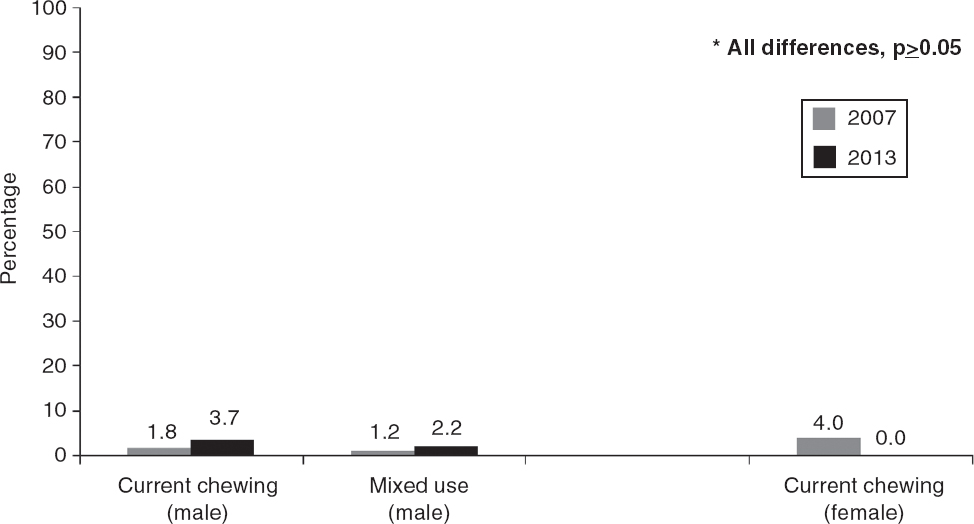 |
| Figure 2. Changes in prevalence of reported chewing (alone and with smoking) among male and female medical students in Bengaluru in 2007 and 2013 |
Discussion
Studies investigating secular changes in tobacco use are rare in India. While three data points may be more suggestive of a trend than the two data points that we have, our study is still useful in showing the overall direction of change. Smoking and chewing rates in Bengaluru were consistently lower than those reported from other colleges in India. [7],[8],[9] Our two separate cross-sectional studies have shown that while regular smoking or chewing habits among male and female students have remained the same, experimental use among male and female students has increased significantly over this time period. These observed differences could be real or due to selection bias (with non-respondents being systematically different from respondents) or information bias (due to tobacco use misclassification). [10],[11] Overall, the participation rate in our study was high and consistent with that observed in earlier studies; [9],[12],[13] further, it is suggested that non-response bias may be less of an issue in surveys of health professionals than of the general public. [14] We, therefore, believe that our findings provide a realistic assessment.
However, college student smokers are not a homogeneous group. Different categories have been identified earlier with different smoking trajectories [15] and different implications for nicotine dependence [16] and health and other outcomes. [17] It is unclear whether students who have experimented with smoking in the past, either in school or college, will transition to regular use in the future in the face of the efforts of the tobacco industry to reach new markets with the aid of multiple traditional gimmicks to lure youth as well as through the introduction of e-cigarettes. [1],[18] An increasing trend of smoking was noted in the east European region about a decade back [19],[20] following large tobacco companies looking for newer markets. Increased psychosocial risk, key socioeconomic factors, external environment and continuing lack of access to tobacco control education could all potentially lead to greater vulnerability among students who have experimented with smoking in the past.
While it is encouraging to know that there was no increase in current smoking or chewing among medical students in Bengaluru over the 5-year period, any tobacco use is still a cause for concern among doctors of tomorrow. It is therefore important for schools and colleges to increase access to tobacco control education so that doctors in training are better prepared to deal with the challenges of the future with regard to their own tobacco use as well as that of their patients.
Acknowledgements
The author is grateful to the deans of the participating institutions for granting permission and facilitating the conduct of the surveys. Students′ participation is also acknowledged. The participating institutions were St John′s Medical College, Bangalore Medical College, M.S. Ramaiah Medical College and Kempegowda Institute of Medical Sciences. The assistance of Anu John, Anita Nath, Smitha K. and Vivek Ramesh in data collection/management is also acknowledged.
| 1. | Stuckler D, McKee M, Ebrahim S, Basu S. Manufacturing epidemics: The role of global producers in increased consumption of unhealthy commodities including processed foods, alcohol, and tobacco. PLoS Med 2012; 9: e1001235. [Google Scholar] |
| 2. | Palipudi KM, Gupta PC, Sinha DN, Andes LJ, Asma S, McAfee T; GATS Collaborative Group. Social determinants of health and tobacco use in thirteen low and middle income countries: Evidence from Global Adult Tobacco Survey. PLoS One 2012; 7: e33466. [Google Scholar] |
| 3. | A. T. Kearney Inc. 2014 Global cities index and emerging cities outlook. Global cities: Present and future. A. T. Kearney Inc. Available at www.atkearney.in/documents/10192/4461492/Global+Cities+Present+and+Future-GCI+2014.pdf/3628fd7d-70be-41bf-99d6-4c8eaf984cd5 (accessed on 10 Nov 2014). [Google Scholar] |
| 4. | Census 2011. Registrar General and Census Commissioner. Ministry of Home Affairs, Government of India, New Delhi, 2011. Available at www.census2011.co.in/census/city/448-bangalore.html (accessed on 13 Apr 2012). [Google Scholar] |
| 5. | WHO. Tobacco-free initiative. WHO/CDC Global Health Professional Survey (GHPS)-2007. Available at www.who.int/tobacco/surveillance/ghps/en/index.html (accessed on 3 Aug 2012). [Google Scholar] |
| 6. | Mony PK, John P, Jayakumar S. Tobacco use habits and beliefs among undergraduate medical and nursing students of two cities in southern India. Natl Med J India 2010; 23: 340-3. [Google Scholar] |
| 7. | SEARO. Report on India Global Health Professionals Survey (Medical). South East Asian Regional Organization, 2006. Available at www.searo.who.int/LinkFiles/GHPS_Report_India2006.pdf (accessed on 18 Jul 2013). [Google Scholar] |
| 8. | Mohan S, Pradeepkumar AS, Thresia CU, Thankappan KR, Poston WS, Haddock CK, et al. Tobacco use among medical professionals in Kerala, India: The need for enhanced tobacco cessation and control efforts. Addict Behav 2006; 31: 2313-18. [Google Scholar] |
| 9. | Sinha DN, Rinchen S, Palipudi KM, Naing Shein NN, de Silva P, Khadka BB, et al. Tobacco use, exposure to second-hand smoke, and cessation training among the third-year medical and dental students in selected member states of South-East Asia region: A trend analysis on data from the Global Health Professions Student Survey, 2005-2011. Indian J Cancer 2012; 49: 379-86. [Google Scholar] |
| 10. | Delgado-Rodríguez M, Llorca J. Bias. J Epidemiol Community Health 2004; 58: 635-41. [Google Scholar] |
| 11. | Levinson AH, Campo S, Gascoigne J, Jolly O, Zakharyan A, Tran ZV. Smoking, but not smokers: Identity among college students who smoke cigarettes. Nicotine Tob Res 2007; 9: 845-52. [Google Scholar] |
| 12. | Smith DR, Leggat PA. An international review of tobacco smoking among medical students. J Postgrad Med 2007; 53: 55-62. [Google Scholar] |
| 13. | Warren CW, Sinha DN, Lee J, Lea V, Jones NR. Tobacco use, exposure to secondhand smoke, and cessation counseling among medical students: Cross-country data from the Global Health Professions Student Survey (GHPSS), 2005-2008. BMC Public Health 2011; 11: 72. [Google Scholar] |
| 14. | Kellerman SE, Herold J. Physician response to surveys: A review of the literature. Am J Prev Med 2001; 20: 61-7. [Google Scholar] |
| 15. | Sutfin EL, Reboussin BA, McCoy TP, Wolfson M. Are college student smokers really a homogeneous group? A latent class analysis of college student smokers. Nicotine Tob Res 2009; 11: 444-54. [Google Scholar] |
| 16. | Lessov-Schlaggar CN, Hops H, Brigham J, Hudmon KS, Andrews JA, Tildesley E, et al. Adolescent smoking trajectories and nicotine dependence. Nicotine Tob Res 2008; 10: 341-51. [Google Scholar] |
| 17. | Caldeira KM, O'Grady KE, Garnier-Dykstra LM, Vincent KB, Pickworth WB, Arria AM. Cigarette smoking among college students: Longitudinal trajectories and health outcomes. Nicotine Tob Res 2012; 14: 777-85. Nicotine Tob Res 2012; 14: 777-85.'>[Google Scholar] |
| 18. | Carroll Chapman SL, Wu LT. E-cigarette prevalence and correlates of use among adolescents versus adults: A review and comparison. J Psychiatr Res 2014; 54: 43-54. [Google Scholar] |
| 19. | Baska T, Basková M, Hudecková H, Straka S, Mad'ar R. Increasing trends of tobacco use in medical students in Slovakia--a reason for concern? Cent Eur J Public Health 2007; 15: 29-32. Cent Eur J Public Health 2007; 15: 29-32.'>[Google Scholar] |
| 20. | Stojanoviæ D, Barbir A, Kralj V, Malatestiniæ D, Cattunar A, Ceroviæ R. Increasing smoking prevalence among pupils of several Croatian secondary medical schools between 1990 and 2006. Coll Antropol 2011; 35: 695-700. [Google Scholar] |
Fulltext Views
1,648
PDF downloads
382




