Translate this page into:
Malaria case detection in Chhattisgarh, 2015–2019: Comparison of cases reported by the National Vector Borne Disease Control Programme and community health workers
Corresponding Author:
Samir Garg
State Health Resource Centre, Bijli Office Chowk, Kaali Baadi, Raipur 492001, Chhattisgarh
India
koriya@gmail.com
| How to cite this article: Garg S, Chatterjee PK, Dewangan M, Nanda P. Malaria case detection in Chhattisgarh, 2015–2019: Comparison of cases reported by the National Vector Borne Disease Control Programme and community health workers. Natl Med J India 2020;33:252-253 |
The National Vector Borne Disease Control Programme (NVBDCP) has reported a dramatic decline in the cases of malaria in India from 2017 onwards, led by the two high-burden states of Odisha and Chhattisgarh.[1] However, many have doubted the officially reported number of malaria cases in India.[2],[3] Estimates of malaria incidence by the WHO have been several times higher.[4] According to the Joint Monitoring Mission for Malaria in 2014, the actual number of cases could be around six times the NVBDCP’s reported numbers.[5] Therefore, there is a need to triangulate official statistics with other sources, e.g. data from community health workers (CHWs), non-governmental organizations (NGOs) and other healthcare providers.
Chhattisgarh has a network of 70 000 CHWs known as ‘Mitanins’. Mitanin-CHWs are residents of the habitation they cover, and the average population per CHW is around 300.[6] In 2015, the state started implementing community case management of malaria through Mitanin-CHWs.[7] The programme involved training and equipping CHWs for this role—combining social mobilization for prevention, using bivalent rapid diagno stickits (RDKs) to detect malaria and to treat Plasmodium falciparum (Pf) cases with artemisinin combination therapy and Plasmodium vivax (Pv) cases with chloroquine.[7] CHWs used RDKs evaluated and approved by the WHO with a false-positive rate of 1.4% for Pf and 1.3% for Pv.[8] The WHO has recommended these RDKs for use in field conditions.[8] An assessment of 1106 CHWs in 2016 showed that 98% could carry out correct testing and 88% had adequate skills in treatment; this was confirmed later in an external evaluation.[9],[10] Around one-third of annual tests done by formal health workers were through RDKs. In absolute numbers in 2019, RDK tests done by formal health workers were around 1.8 million, almost equal to the number of RDK tests done by CHWs.
The name-wise lists of tests, results and treatment were recorded in the CHW registers. Subcentre-wise reports of testing done by CHWs were collected monthly by their supervisors and compiled at the state level. The reports of NVBDCP covered detection done by the formal health workers of the government and did not include the testing done by CHWs. We believe there is no duplication in the number of cases between the two sources. No information was included by either source on cases detected by NGOs or private providers.
A substantial decline in malaria cases was reported by the NVBDCP as well as CHWs after 2017 [Table - 1]. The increase from 2015 to 2017 is likely to be due to increased testing and not due to malaria increasing in this period.
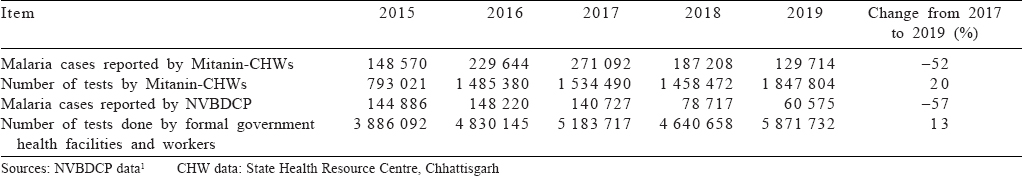
CHWs diagnosed twice as many cases as detected by formal health workers. Although CHWs reported greater incidence than NVBDCP’s reports, this data source confirms the decline in the incidence of malaria after 2017. Factors that might have helped Chhattisgarh include community-level detection and treatment by CHWs and bednet distribution. CHWs are able to diagnose greater number of cases because through them detection has become available close to where people live. It can be a key factor in tribal populations and remote areas in which most malaria occurs in India. Detection by CHWs has been a big part of the success in Odisha too.[11],[12],[13],[14] Odisha has also shown a steep decline in malaria in 2018 using a strategy of mass testing in high-burden areas, including in the afebrile population.[11],[12],[13],[14] Chhattisgarh’s CHWs in high-burden tribal districts will be crucial in achieving good coverage under mass testing on the lines of Odisha.
While malaria is on the decline in some of the key states, further strategies may be needed for sustaining the gains. Many states in India, especially those with sizeable tribal populations, can learn from the CHW-led strategy in managing malaria. Having a well-equipped workforce close to community can offer advantages in sustaining the change.
The key systemic gaps contributing to under-reporting of malaria in India include poor access to detection, poor systems of surveillance and lack of data-sharing between the public and private sectors.[5],[15] A system to integrate private sector data has often been suggested but is yet to emerge. Access to detection has improved due to RDKs, especially through CHWs in case of Chhattisgarh. Chhattisgarh does include RDK-based detection by formal health workers in its reporting, which may not be the case in some other states in India.[16] However, the data of cases diagnosed by CHWs have not been included in Chhattisgarh despite being easily available as part of a government-funded programme. The formal information system needs to take into account the data on testing by CHWs, NGOs and private providers if we want a more realistic picture of malaria in India.
Conflicts of interest. None declared
| 1. | National Vector Borne Disease Control Programme (NVBDCP). Malaria situation in India, 2015. Available at https://nvbdcp.gov.in/WriteReadData/l892s/15048331161580734250.pdf (accessed on 10 Feb 2020). [Google Scholar] |
| 2. | Dash AP. Estimation of true malaria burden in India: A profile of National Institute of Malaria Research. 2nd ed. New Delhi:National Institute of Malaria Research; 2009:91–9. [Google Scholar] |
| 3. | Hay SI, Gething PW, Snow RW. India’s invisible malaria burden. Lancet 2010;376:1716–17. [Google Scholar] |
| 4. | World Health Organization. World Malaria Report 2017. Geneva:WHO; 2017. Available at www.who.int/malaria/world_malaria_report_2017 (accessed on 10 Feb 2020). [Google Scholar] |
| 5. | Director General of Health Services. Joint Monitoring Mission 2014–National Vector Borne Disease Control Programme. NVBDCP, Ministry of Health and Family Welfare, Government of India and WHO; 2015. [Google Scholar] |
| 6. | Ministry of Health and Family Welfare. Update on ASHA Programme. National Health Systems Resource Centre; 2016. [Google Scholar] |
| 7. | Department of Health and Family Welfare, Chhattisgarh. Treatment and prevention of malaria: Guidelines for Mitanin. Raipur:National Vector Borne Disease Control Programme; 2014. Available at https://shsrc.in/wp-content/uploads/ 2019/09/Mitanin_Malaria_Guideline_2014.pdf/ (accessed on 24 Jan 2020). [Google Scholar] |
| 8. | World Health Organization. Malaria rapid diagnostic test performance: Summary results of WHO product testing of malaria RDTs: Round 1–7 (2008–2016). Geneva:WHO; 2017:14. [Google Scholar] |
| 9. | State Health Resource Centre. Field level skill assessment of Mitanin CHWs in testing and treatment for malaria; 2016. Available at https://shsrc.in/wp-content/ uploads/2020/02/Field-Level-Skill-Assessment-of-Mitanin-CHWs-in-Testing- Treatment-for-Malaria-2016.pdf (accessed on 24 Jan 2020). [Google Scholar] |
| 10. | State Health Resource Centre. External evaluation of Mitanin––Skill assessment by NIOS; 2019. Available at https://shsrc.in/wp-content/uploads/2020/02/ External-Evaluation-of-Mitanin-for-Skill-Assessment-by-NIOS-2019.pdf (accessed on 24 Jan 2020). [Google Scholar] |
| 11. | Pradhan MM, Anvikar AR, Daumerie PG, Pradhan S, Dutta A, Shah NK, et al. Comprehensive case management of malaria: Operational research informing policy. J Vector Borne Dis 2019;56:56–9. [Google Scholar] |
| 12. | Panda B, Mohapatra MK, Paital S, Kumbhakar S, Dutta A, Kadam S, et al. Prevalence of afebrile malaria and development of risk-scores for gradation of villages: A study from a hot-spot in Odisha. PLoS One 2019;14:e0221223. [Google Scholar] |
| 13. | Pradhan MM, Meherda PK. Malaria elimination drive in Odisha: Hope for halting the transmission. J Vector Borne Dis 2019;56:53–5. [Google Scholar] |
| 14. | Pradhan S, Pradhan MM, Dutta A, Shah NK, Joshi PL, Pradhan K, et al. Improved access to early diagnosis and complete treatment of malaria in Odisha, India. PLoS One 2019;14:e0208943. [Google Scholar] |
| 15. | Yadav RS, Bhatt RM, Kohli VK, Sharma VP. The burden of malaria in Ahmedabad city, India: A retrospective analysis of reported cases and deaths. Ann Trop Med Parasitol 2003;97:793–802. [Google Scholar] |
| 16. | Rao M. India cannot eliminate malaria if a large state like Andhra Pradesh cannot count its cases correctly. Scroll.in; 2017. Available at https://scroll.in/pulse/ 845255/india-cannot-eliminate-malaria-if-a-large-state-like-andhra-cannot-even-count-its-cases-correctly (accessed on 28 Jul 2017). [Google Scholar] |
Fulltext Views
1,361
PDF downloads
230




