Translate this page into:
Male infertility in India: Demographics, aetiology and outcomes of standard clinical practice
2 Department of Anatomy, All India Institute of Medical Sciences, New Delhi, India
Corresponding Author:
Rajeev Kumar
Department of Urology, All India Institute of Medical Sciences, New Delhi
India
rajeev.urology@aiims.edu
| How to cite this article: Kaushal R, Gurnani N, Kumar M, Dada R, Kumar R. Male infertility in India: Demographics, aetiology and outcomes of standard clinical practice. Natl Med J India 2020;33:340-343 |
Abstract
Background. Although the outcomes of assisted reproductive technologies (ART) and corrective surgery for male infertility are reported in the literature, these are based on studies specifically designed to assess the outcomes of individual interventions and do not reflect the real-life (intent-to-treat) outcomes of managing infertility. There are sparse data on the actual utilization of treatment and pregnancy outcomes in these patients. We aimed to evaluate the demographics, aetiology, treatment utilization and outcomes of treatment of male infertility in a tertiary care centre.Methods. We prospectively enrolled 447 infertile males for evaluation over 30 months beginning October 2015. All patients were evaluated and investigated as per the study protocol to identify the cause of infertility. The patients were advised interventions based on the diagnosis and were followed up to assess delivery of treatment and outcomes of interventions in terms of pregnancy rates.
Results. Of the 447 enrolled patients, 426 (mean age 31 years) completed the initial diagnostic evaluation. About 83% had primary infertility, 40% had oligo/astheno/ teratozoospermia, 40% had azoospermia, and 21.1% had obstructive azoospermia. Genetic abnormalities were detected in 9.3% of the 162 patients screened. ART was advised for 71.8% of patients, but only 18% of patients actually received the treatment though they had a high success rate (38%). In contrast, surgery was recommended to only 35 (8.2%) patients, but only 18 (58%) received the recommended treatment with a pregnancy rate of 33.3%. Overall, only 24.4% of patients received the advised treatment with a pregnancy rate of 36.8%.
Conclusions. ART was the most common intervention recommended, but less than one-fourth of couples received the recommended treatment. Surgery is indicated in a small number of patients, but is delivered to a larger proportion than those advised ART with both modalities having similar pregnancy outcomes.
Introduction
Pregnancy is the outcome of a complex interplay between the male and female partner and around 15% of couples fail to achieve spontaneous pregnancy, requiring evaluation and management for infertility.[1],[2] Advances in assisted reproductive technologies (ART) have enabled conception among couples with wide ranging abnormalities. The male partner contributes to infertility in nearly 50% of couples.[3] However, it is often considered unrewarding to look for the cause and treat male infertility because ART facilitates bypassing the cause of infertility by enabling conception with sperm retrieved from the testis or epididymis, providing a quick solution to male factor infertility.
While ART is the only option available in a proportion of cases, many others may be candidates for alternative modalities of treatment including medications and surgery. ART not only places the onus of treatment on the ‘normal’ female partner who may have to suffer adverse social and physical effects,[4] it is expensive and not always affordable.[5],[6] Evaluating and treating the infertile males may lead to a spontaneous conception, lower treatment costs and identification of key underlying pathologies.[7]
Many studies have evaluated the outcomes of individual treatments of male factor infertility including drug therapy, surgery and ART.[8],[9],[10] However, these have assessed the results of specific interventions in select populations, akin to a per-protocol analysis and not the treatment outcomes of male infertility as a whole.[11] Even though physicians may advise the most appropriate treatment, the actual treatment received is often different and may be influenced by affordability, availability and acceptability. This is particularly relevant in the case of male infertility where the treatment is expensive and involves the ‘normal’ partner. Data on real-life outcomes of managing the infertile male population as a whole would be useful in devising policies and strategies for addressing this issue. We prospectively evaluated the overall profile of patients who presented to us with male infertility, their aetiology and outcomes of interventions for these conditions to assess the role of each intervention and lacunae in the current treatment delivery systems.
Methods
This prospective study was approved by the ethics committee and was carried out in a dedicated Andrology and Male Infertility clinic of a tertiary care public hospital over 36 months beginning October 2015. All males presenting with infertility were screened for inclusion. The clinic registers over 40 patients weekly and to avoid diversion of resources to the research protocol, a maximum of 5 consecutive new patients were invited to enrol for the study on each clinic day. There were no exclusion criteria other than refusal to participate.
Males who consented for inclusion underwent a standard clinical evaluation comprising detailed history, focused physical examination and at least two semen analyses (reported as per the WHO 1999 classification).[12] If the two reports were discordant in terms of categorization of infertility, the report suggesting the less severe abnormality (azoospermia/oligo/astheno/teratozoo-spermia [OATs]/normal semen) was considered for planning further investigations, followed by appropriate treatment and assessment of outcomes.
Additional tests were carried out to identify the aetiology of infertility. All males with unexplained infertility (normal semen parameters) were tested for reactive oxygen species (ROS) levels. Azoospermic males with low volume ejaculate (<1.5 ml) underwent serum total testosterone measurement, transrectal ultrasound for ejaculatory duct obstruction and post-ejaculatory urine analysis for sperms to rule out retrograde ejaculation. Serum follicle-stimulating hormone (FSH) was tested for males with normal volume azoospermia and palpable vas deferens; fine-needle aspiration cytology of the testis was done if the FSH was less than twice the normal value. If spermatogenesis was normal, the patients were diagnosed to have obstructive azoospermia (OA). Patients classified as non-obstructive azoospermia (NOA) underwent karyotyping and Yq microdeletion analysis. All patients with OATs were advised ROS testing and those with severe OATs (counts <5 million/ml) underwent karyotype and Yq microdeletion assays. Details of our evaluation and diagnostic protocols have previously been published.[13],[14]
Measurement of ROS[15]
ROS levels were determined using a chemiluminescence technique using luminol (5-amino-2,3-dihydro-1,4-phthalazinedione) as a probe. Aliquots of liquefied semen were centrifuged at 300 g for 7 minutes. A 10 μl aliquot of luminol prepared as 5 mmol/L stock in dimethylsulfoxide was added to 400 μl of the washed sperm suspension; 10 ml of 5 mol/L luminol was added to 400 μl of PBS, which served as a negative control. Levels of ROS were determined by measuring chemiluminescence with a luminometer. Results were expressed in RLU/ minute/20 million sperms.
Interventions were recommended based on the diagnosis with no study-specific intervention. The options for intervention included drug therapy, surgery and ART. All males who completed the initial evaluation were included in the assessment of demographics and aetiology of infertility. All males who were available for follow-up were assessed for the completion of recommended treatment and outcomes in terms of pregnancy till the date of last follow-up.
Results
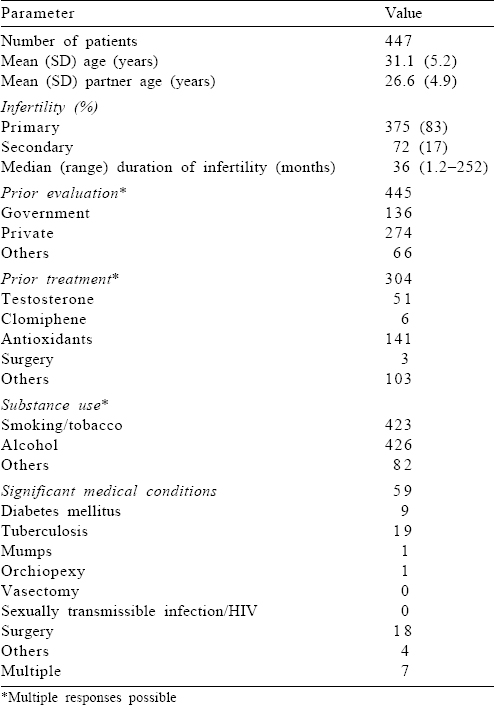
Four hundred and forty-seven infertile males were enrolled in the study, of whom 426 completed the evaluation. The mean (SD) age was 31.1 (5.2) years and the mean (SD) partner age was 26.6 (4.9) years. The median duration of infertility was 36 months (range 1.2–252 months); 83% had primary infertility. All patients had undergone evaluation for infertility before presenting to our clinic, of which 274 were evaluated at a private centre while the remaining at a government institution or by some unqualified practitioner. One hundred and forty-one (31.5%) patients had received antioxidant therapy and 163 (36.4%) had received other forms of therapy before presenting to us [Table - 1]. Nearly all patients had a history of consuming tobacco and/or alcohol. Eighty-one patients consumed alcohol occasionally and 51 habitually; whereas there were 20 occasional and 132 habitual users of tobacco.
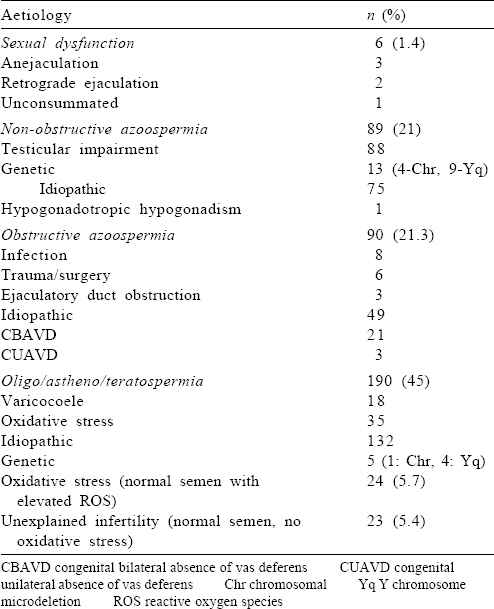
OAT was the single largest category of patients (190; 45%) followed by azoospermia (179, 42.3%) of whom nearly half were diagnosed to have OA (90, 21.3%). Twenty-three (5.4%) patients had unexplained infertility (provided female factor was excluded) with a normal semen analysis and normal ROS levels [Table - 2].
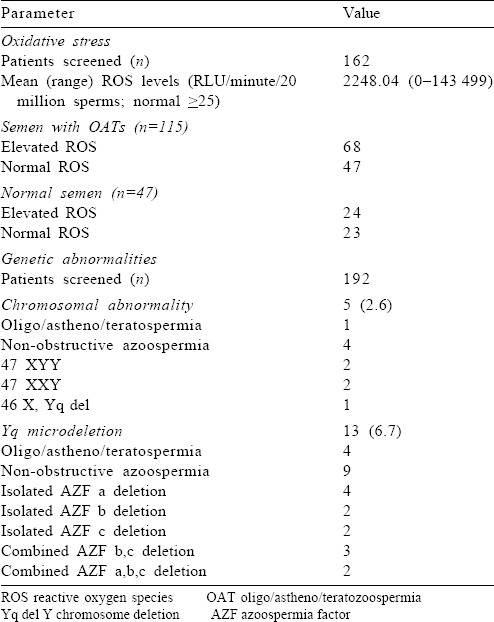
One hundred and sixty-two patients (115 OATs, 47 normal semen parameters) were screened for ROS [Table - 3]. Sixty-eight of the 115 OAT (60%) patients and 24/47 (51%) patients with normal semen parameters had elevated ROS. A total of 192 patients (100 OATs, 92 NOA) were screened for genetic abnormalities; 5/192 (2.6%) patients had chromosomal abnormalities, while 13 (6.7%) patients had Yq microdeletion(s) [Table - 3].
Of the 422 patients who were assigned a treatment after complete evaluation, 309 were available for follow-up and only 103 had received the assigned treatment [Table - 4]. The most common intervention recommended was ART (306/422, 72.5%) with intracytoplasmic sperm injection (ICSI)/artificial insemination with donor sperms in 233 patients and intrauterine insemination with partner’s sperm in 73. Among these 306, only 55 (18%) underwent the recommended treatment. Surgery was recommended for 31 patients (7.3%) of whom 18 received the treatment (58%). Drug therapy was offered to 70 patients of whom 29 (41%) received the treatment.
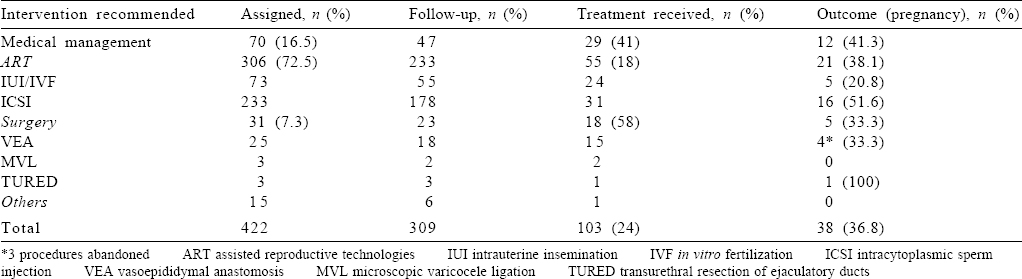
The overall pregnancy rate among 103 patients who received treatment was 36.8%. For surgery, the pregnancy rate was 33.3%, for ART it was 38%, and for those who received medical therapy it was 41%.
Discussion
Our study highlights many aspects of real-life management of male infertility in India. Most males present late and suffer from primary infertility. Almost all have undergone prior interventions and the use of tobacco and alcohol is common among them. A diagnosis can be made in nearly 95% of males. Azoospermia and OATs contribute around 40% of cases each while sexual dysfunction is an uncommon cause of infertility. The majority of patients are advised ART but few received the treatment. Surgery is recommended in fewer patients, but a higher percentage receives the recommended treatment. More than one-third of couples who receive the intended treatment are able to achieve pregnancy.
Delayed presentation with a mean duration of infertility of over 6 years could be due to multiple reasons, most of which are a reflection on our societal and healthcare systems. First, social norms place the onus of fertility on the female partner and the male is rarely investigated before evaluation of the female.[14] Second, though most males had received prior evaluation and some form of treatment, indicating that the true presentation is at <6 years, their continued unresolved problems suggest a lack of sufficient resources both in terms of trained human resource and finances to address the problem.
The overall pattern of diagnoses in our cohort is similar to that previously reported but has some remarkable differences, which could be because of referral bias.[16] Only a single case of hypogonadotropic hypogonadism was diagnosed in this cohort suggesting most cases were referred to endocrinologists, a potential referral bias. Although OA was diagnosed in 90 patients, 24 of these were due to an absent vas deferens. This is an uncommonly high occurrence in any cohort and may be due to referral patterns, or the patients’ failure to receive appropriate advice and treatment in their prior consultations.[17] Congenital bilateral absence of vas deferens is a clinical diagnosis and requires the least number of investigations and patient visits. However, it requires experience and clinical examination that may not always have been performed. On the other hand, only 18 patients (4.7%) among the OATs cohorts were diagnosed to have a varicocele while most series of infertile males would have a much higher prevalence (30%–40%) of varicoceles.[18],[19] Since varicoceles are easier to diagnose, both clinically and with an ultrasound, patients with this diagnosis may have been identified and treated before they presented to us. Both these factors contributed to a relatively small proportion (7.3%) of patients in our cohort who were considered candidates for surgery. This would also explain the high recommendation rate for ART since treatable conditions may have been addressed before referral.
About 60% of patients with OATs and 51% of those with normal semen analysis in our cohort had elevated ROS levels. Oxidative stress has been suspected to contribute to male infertility by impairing sperm counts, motility and other seminal parameters by causing oxidant DNA damage.[20],[21],[22] However, its exact role in causation of infertility is uncertain and needs further study. Genetic abnormalities are reported to cause about 10% of male infertility and we found a similar percentage of abnormalities in our cohort.[23],[24] Identification of these abnormalities helps counsel couples and can prevent the transmission of genetic disorders in the foetus.
Despite the 3-year duration of our study, only 103 among the 422 (25%) patients actually completed the assigned treatment, while another 134 were awaiting initiation of treatment. Among those who completed the assigned treatment, 36.8% achieved successful pregnancy. Although ART was the most common recommended treatment (72.5%) and had a high success rate among those who received the treatment (38%), few actually received the treatment (18%). The lowest utilization rate was for ICSI where only 13.3% of patients received the recommended treatment despite its high pregnancy rate of 51.6%. In contrast, although surgery was recommended to fewer patients, a much higher percentage received the treatment (58%) with equivalent success rate (33.3%). This could be a reflection on the socioeconomic status of our patient as ours is a public-funded tertiary care institution with long waiting lists. In our institution, surgery is available at very little cost to the patient while ART is less expensive than private institutions.
We did not aim to determine the outcome of any individual form of treatment for male infertility. Our objective was to assess the real-life picture of management of male infertility in India. A limitation of this study is the potential referral bias. Patients who visit our institution are primarily from lower socioeconomic strata and they often have to wait for long periods to avail its services. Their lack of resources also limits access to advanced interventions such as ART. However, as about two-thirds of the Indian population belongs to this stratum, it reflects the situation in most of the country. We used a convenient sampling method by including only 5 new cases from each clinic instead of all patients, which could lead to a selection bias. The overall low number of patients who received the treatment in each group is also a potential limitation, but this is the reality the study aimed to seek.
Conclusions
Our study identifies the demographics, aetiology, delivery of treatment and outcomes of treatment of male infertility in India. Pregnancy rates following interventions are around 37% while only <25% of couples were able to receive the recommended treatment. ART has a high success rate, but only 18% of the patients who were advised treatment received it. In comparison, surgery was received by 58% of patients with a similar success rate. There is a need to intensify training and increase facilities for providing appropriate diagnosis and surgical interventions for male infertility.
Acknowledgements
The study was funded by the Indian Council of Medical Research, New Delhi vide grant number RCH/Ad-hoc/27/2014-2015.
Conflicts of interest. None declared
| 1. | Brandes M, Hamilton CJ, Van Der Steen JO, De Bruin JP, Bots RS, Nelen WL, et al. Unexplained infertility: Overall ongoing pregnancy rate and mode of conception. Hum Reprod 2011;26:360–8. [Google Scholar] |
| 2. | Aanesen A, Westerbotn M. Prospective study of a Swedish infertile Cohort 2005–08: Population characteristics, treatments and pregnancy rates. Fam Pract 2014;31:290–7. [Google Scholar] |
| 3. | Esteves SC, Miyaoka R, Agarwal A. An update on the clinical assessment of the infertile male. Clinics (Sao Paulo) 2011;66:691–700. [Google Scholar] |
| 4. | Springen K. How women around the world cope with infertility. Available at www.newsweek.com/id/158625 (accessed on 13 Nov 2018). [Google Scholar] |
| 5. | Allahbadia GN. Have we finally written the obituary for conventional IVF? IVF Lite 2014;1:1–5. [Google Scholar] |
| 6. | Lunenfeld B, van Steirteghem A. Infertility in the third millennium: Implications for the individual, family and society: Condensed meeting report from the Bertarelli Foundation’s second global conference. Hum Reprod Update 2004;10:317–26. [Google Scholar] |
| 7. | Alukal JP, Lipshultz LI. Why treat the male in the era of assisted reproduction? Semin Reprod Med 2009;27:109–14. [Google Scholar] |
| 8. | Garg H, Kumar R. Empirical drug therapy for idiopathic male infertility: What is the new evidence? Urology 2015;86:1065–75. [Google Scholar] |
| 9. | Agarwal A, Sekhon HL. The role of antioxidant therapy in the treatment of male infertility. Hum Fertil (Camb) 2010;13:217–25. [Google Scholar] |
| 10. | Chiles KA, Schlegel PN. Role for male reconstruction in the era of assisted reproductive technology. Fertil Steril 2016;105:891–2. [Google Scholar] |
| 11. | Winters BR, Walsh TJ. The epidemiology of male infertility. Urol Clin North Am 2014;41:195–204. [Google Scholar] |
| 12. | World Health Organization. WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction. Geneva:WHO; 1999. [Google Scholar] |
| 13. | Tiwari DP, Razik A, Das CJ, Kumar R. Prospective analysis of factors predicting feasibility and success of longitudinal intussusception vasoepididymostomy in men with idiopathic obstructive azoospermia. Indian J Med Res 2019;149:51–6. [Google Scholar] |
| 14. | Kumar R. Surgery for azoospermia in the Indian patient: Why is it different?Indian J Urol 2011;27:98–101. [Google Scholar] |
| 15. | Moustafa HM, Sharma RK, Thornton J, Mascha E, Hafez AA, Thomas AJ, et al. Relationship between ROS production, apoptosis and DNA denaturation in spermatozoa from patients examined for infertility. Hum Reprod 2004;19:129–38. [Google Scholar] |
| 16. | Sabanegh E, Agarwal A. Male infertility. In: Scott McDougal W, Wein AJ, Kayoussi LR, Novick AC, Partin AW, Peters CA, et al. (eds). Campbell-Walsh Urology. 10th ed. Philadelphia:Elsevier Saunders; 2011:616–47. [Google Scholar] |
| 17. | Ferlin A, Raicu F, Gatta V, Zuccarello D, Palka G, Foresta C. Male infertility: Role of genetic background. Reprod Biomed Online 2007;14:734–45. [Google Scholar] |
| 18. | Cozzolino DJ, Lipshultz LI. Varicocele as a progressive lesion: Positive effect of varicocele repair. Hum Reprod Update 2001;7:55–8. [Google Scholar] |
| 19. | Al-Said S, Al-Naimi A, Al-Ansari A, Younis N, Shamsodini A, A-Sadiq K, Shokeir AA. Varicocelectomy for male infertility: A comparative study of open, laparoscopic and microsurgical approaches. J Urol 2008;180:266–70. [Google Scholar] |
| 20. | Venkatesh S, Riyaz A, Shamsi MB, Kumar R, Gupta NP, Mittal S, et al. Clinical significance of reactive oxygen species in semen of infertile Indian men. Andrologia 2009;41:251–6. [Google Scholar] |
| 21. | Shamsi MB, Venkatesh S, Tanwar M, Talwar P, Sharma RK, Dhawan A, et al. DNA integrity and semen quality in men with low seminal antioxidant levels. Mutation Res 2009;665:29–36. [Google Scholar] |
| 22. | Shamsi MB, Imam SN, Dada R. Sperm DNA integrity assays: Diagnostic and prognostic challenges and implications in management of infertility. J Assisted Reprod Genet 2011;28:1073–85. [Google Scholar] |
| 23. | Mitra A, Dada R, Kumar R, Gupta NP, Kucheria K, Gupta SK. Screening for Y-chromosome microdeletions in infertile Indian males: Utility of simplified multiplex PCR. Indian J Med Res 2008;127:124–32. [Google Scholar] |
| 24. | Nagvenkar P, Desai K, Hinduja I, Zaveri K. Chromosomal studies in infertile men with oligozoospermia and non-obstructive azoospermia. Indian J Med Res 2005;122:34–42. [Google Scholar] |
Fulltext Views
11,260
PDF downloads
2,723




