Translate this page into:
Mental and behavioural emergencies at a tertiary healthcare centre in India: Pattern and profile
Corresponding Author:
Raman Deep
Department of Psychiatry, All India Institute of Medical Sciences, Ansari Nagar, New Delhi 110029
India
drramandeep@gmail.com
| How to cite this article: Kumar S, Singh S, Deep R. Mental and behavioural emergencies at a tertiary healthcare centre in India: Pattern and profile. Natl Med J India 2018;31:339-342 |
Abstract
Background. Sparse data are available on service utilization, pattern and profile of mental and behavioural emergencies in India. We explored the pattern and clinical profile of consecutively referred psychiatric emergencies at a premier tertiary healthcare centre in India.Methods. We reviewed the consecutive referrals for acute mental and behavioural problems made by the emergency department and recorded in an emergency psychiatry register between January 2015 and January 2016.
Results. Over a 1 3-month period, 666 patients were assessed; of whom 473 (71 %) had no prior/known psychiatric history and 84 (12.6%) had a comorbid medical condition. Nearly one-third of patients had potential legal issues associated with their emergency. The most common reasons for presentation were: an attempt at self-harm (130; 19.5%), aggression/agitation ( 122; 18.3%) and psychoactive substance use-related problems (69; 10.3%). Schizophrenia and other psychotic disorders (89; 13.4%) and mood disorders (87; 1 3.1%) formed the 2 most common diagnostic groups seen in emergency. Most commonly prescribed medications were benzodiazepines (296; 44.4%) followed by antipsychotics (187; 28.1%) and antidepressants (90; 13.5%). Notably, 11% of patients (76) were advised immediate admission under psychiatry, half of whom could be admitted directly from the emergency.
Conclusion. Our findings suggest that there is a need to optimize emergency mental healthcare and develop service delivery models for common psychiatric emergencies in India.
Introduction
As per WHO estimates, mental and substance-use disorders are the leading cause of disease burden worldwide as measured by years lived with disability (YLDs) and account for 22.9% of all the YLDs.[1]
Psychiatric or behavioural emergencies manifest as an acute disturbance of thought, behaviour or mood of a patient.[2] Various models of care have been prevalent, which include mental health consultations in medical emergency departments (EDs), dedicated mental health wings, crisis stabilization units, psychiatric emergency services (PES), crisis centres and mobile teams.[3] There is a dearth of evidence on management and models of care for mental and behavioural emergencies in low- and middle-income countries.[4] While psychiatric emergencies pose a considerable burden on emergency services in western countries, data are sparse on service utilization for mental and behavioural emergencies in India. A recent meta-analysis on the epidemiology of mental disorders at EDs including 18 studies from 7 countries (Australia, Canada, Ireland, Norway, Portugal, Spain and the UK) calculated that patients with mental and behavioural disorders accounted for approximately 4% of total ED attendances.[5]
Several Indian studies have evaluated the characteristics of ED patients presenting with a specific mental health condition (such as attempt at self-harm[6] or aggressive/psychotic patients[7]). Few other Indian studies have assessed the overall epidemiology of mental and behavioural disorders in ED settings.[8],[9],[10] Most studies have covered a time period limited to a few months. The profile of callers to a helpline number for behavioural emergencies has also been described in a study from India,[11] but these users did not present to EDs and were not diagnosed or examined by a psychiatrist in person. A recent review on burden of psychiatric emergencies in EDs in India pointed to a lack of studies assessing the epidemiology of different psychiatric emergencies and need for developing PES.[12]
There is a need to gather insights into PES in general hospital settings in India where psychiatric services are provided from the same premises as other medical specialties, and consequently, the pattern and service needs are likely to be different from a mental hospital setting.
We explored the clinical characteristics, reasons for presentation and psychiatric diagnoses of patients referred for psychiatric emergency consultation at a premier tertiary care centre in India between January 2015 and January 2016.
Methods
The Department of Psychiatry, All India Institute of Medical Sciences, New Delhi, provides emergency on-call services via a psychiatric emergency team which attends to patients referred by the Department of Emergency Medicine. PES are provided by a junior resident, a senior resident (qualified psychiatrist) and supervised by a consultant psychiatrist. After a screening and initial evaluation at the Department of Emergency Medicine, patients with known or suspected mental health conditions with acute mental and behavioural changes are referred for psychiatric evaluation on the discretion of the medical officer in-charge. During evaluation, information is obtained from the patient and accompanying attendants (family members/relatives/friends/ police, etc.) and a working diagnosis is made as per the International Classification of Diseases, tenth revision (ICD-10) guidelines. Further evaluation and management is initiated in collaboration with other specialties, if needed.
The details of all the cases are recorded in a register maintained by the Department of Psychiatry. We did a descriptive, quantitative study involving retrospective review and analysis of emergency psychiatry records for patients attended to between January 2015 and January 2016. Further, information about patients with potential medicolegal issues as deemed by the medical officer incharge in the ED and registered as medicolegal cases (MLCs) in the ED was extracted. These included cases brought to the ED by the police and other situations (mostly attempts at self-harm), in which an MLC was instituted later in the ED by the emergency medical officer. Patient confidentiality was maintained using anonymized data with unique identifiers and by password-protected dataset with restricted access. Complete anonymity was maintained during presentation of the study findings. Statistical analysis was done using SPSS version 23.0 (SPSS Inc., IBM Chicago, IL, USA).
Results
A total of 666 patients were assessed by the psychiatric emergency team over the study period, with an average of 2 psychiatric consultations per day (mean 1.7). The mean (SD) age of patients was 31.4 (13.9) years.
There was a previously known history of psychiatric illness in 29% and medical illness in 12.6% of patients [Table - 1]. Nearly 8% ofpatients visited the emergency primarily with medical symptoms/ conditions as the presenting reason.
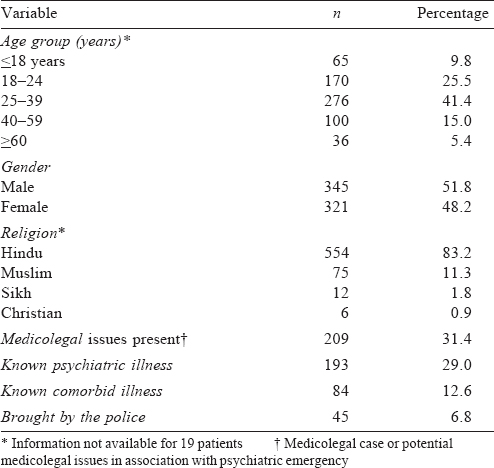
Of the total, 31.4% of patients had either an MLC or potential medicolegal issue associated with their psychiatric emergency, and 45 patients (6.8%) were brought by the police. The common reasons for which patients presented to the ED were attempt at self-harm, followed by aggression/agitation, psychoactive substance use-related problems and dissociation.
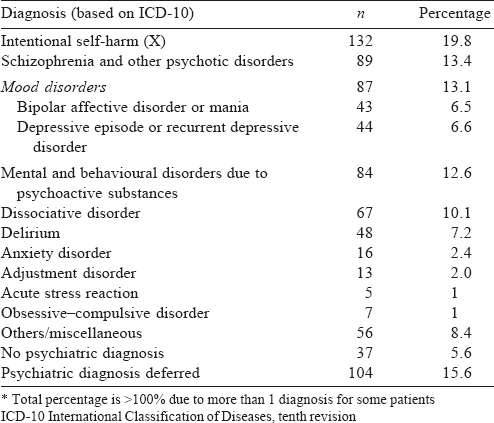
Schizophrenia and other psychotic disorders (13.4%) and mood disorders (13.1%) formed the two most common diagnostic groups followed by psychoactive substance use-related problems [Table - 2]. The most commonly prescribed medications were benzodiazepines (44.4%) followed by antipsychotics (28.1%) and antidepressants (13.5%). About 23% of patients were not prescribed any psychotropic drug on discharge from the Department of Emergency Medicine.
Of the 666 patients, 76 (11%) were advised admission for further psychiatric inpatient care, of which nearly half (34/666) could be admitted directly from the emergency for further inpatient management.
Discussion
We aimed to add some useful information on the profile and pattern of service use for psychiatric emergencies catered by a general hospital psychiatry department in India.
Around two-thirds of the patients belonged to the age range of 18–39 years, considered as the most productive age group, which is consistent with prior reports from other centres.[6],[8] Similar to our study, previous studies also reported an average of 2 psychiatric emergency consultations per day attended by psychiatric units at general hospital settings in India.[7],[8]
The majority of cases were brought by family members or friends (87%), and a significant subset (7%) was also brought by the police (which included the homeless mentally ill, those found wandering in public places or involved in some illegal activity). This is important from the overall management perspective, as these patients have poor social support systems and would require the involvement of a psychiatric/medical social welfare worker, preferably working in the emergency setting itself.
About one-third of patients had potential medicolegal issues or an MLC related to their mental condition. These included cases brought to the ED by the police and other situations (mostly attempts at self-harm), in which an MLC was instituted later in the ED by an emergency medical officer. In addition to providing therapeutic care, emergency psychiatric teams often have to deal simultaneously with the police, protect rights of mentally ill patients and tackle other legal issues hindering effective management. Thus, there is a need to include emergency case management and related medicolegal aspects as part of the training of psychiatrists.[13]
A proportion (12.6%) of patients had a known comorbid medical condition and nearly 8% presented to the ED primarily with a medical symptom and/or physical conditions. Since many medical disorders are known to cause psychiatric symptoms, a failure to suspect and recognize them might delay the requisite treatment and lead to serious morbidity.[14],[15] There is a need for thorough medical evaluation of all patients before and during the psychiatric consultation. This should involve both a careful clinical history and physical examination for the primary or comorbid medical condition.
Interestingly, for more than two-thirds of the patients, it was their first contact ever with the mental healthcare services. A large proportion of patients presenting with psychiatric emergencies had no prior contact with mental healthcare services and/or did not have a diagnosed psychiatric illness. This also has been reported in some earlier studies.[16] After the onset of the initial mental symptoms or behavioural changes, initial contacts are often with faith/alternate healers, and specialized services are sought only when a crisis arises.[17] Further, mental illness and patients are still stigmatized and there is a lack of awareness about psychiatric disorders among the lay people. This highlights the need for mental health professionals to strengthen their link with the community via both the general psychiatric services and the emergency services.
Attempt to self-harm (19.8%) was the most common reason for presentation followed by aggressive/agitated behaviour (18%) and psychoactive substance use-related problems (10.3%). These conditions contribute to half of the psychiatric emergency burden and merit special attention. Regarding emergency mental health interventions, psychotropic drugs were required in a majority of our patients. In nearly one-fourth of patients (23%), only a psychiatric opinion was provided, and wherever relevant, psychological interventions were provided; however, no pharmacotherapy was initiated from the emergency for a certain subset of patients.
A recent systematic review examining management strategies for psychiatric emergencies in non-specialist settings in low- and middle-income countries (LMICs) such as ours emphasized on providing immediate management by treating symptoms of psychiatric emergencies causing distress in the ED rather than focusing on syndromal diagnoses.[4] Further, the two most common emergency presentations seen in our study were of attempted self- harm and agitated/aggressive behaviour, both of which cut across diagnostic categories.[18],[19] The WHO’s mhGAP programme intervention guide for mental, neurological and substance use disorders provides high-quality guidelines for managing different phenotypic presentations of psychiatric emergencies related to these disorders, especially in non-specialist settings in LMICs.[20] These guidelines should be adapted and contextualized according to the resources available to cater to the needs of the target population.
There are 3 models for delivery of psychiatric emergency services: (i) the mental health professional consulting on patients in the ED itself; (ii) a dedicated mental health wing in the ED providing separate and often more calming environment with specially trained and dedicated staff; and (iii) stand-alone psychiatric emergency services—a facility separate from the ED that is solely for treatment of patients with acute mental health issues.[15] In India, with our limited resources and keeping in mind the profile and pattern of patients seeking PES, a hybrid of the first 2 models may be considered. This may be achieved by providing mental health professional services in the ED round-the-clock, on-call basis and, additionally, earmarking a designated area near the nursing/doctors’ counter for psychiatric emergencies for better observation and/or management of patients such as those presenting with an attempt to self-harm or agitated/aggressive behaviour. This may facilitate a routine medical assessment before psychiatric consultation, risk assessment to triage the patients, observation during crisis, provision of immediate psychiatric interventions and decision for further management.
A psychiatric diagnosis could not be reached upon initial evaluation in about 15% of patients which is consistent with prior studies, where diagnosis was deferred in up to one-fourth of cases.[12] Establishing psychiatric diagnosis sometimes requires longitudinal follow-up, whereas in emergency, only limited information may be available. There are additional constraints such as lack of privacy and, at times, a clinician is forced to take only a brief focused history due to the distressing nature of symptoms or risk of imminent threat posed to the patient or other people around the patient.[21]
Notably, 1 in 10 patients was advised admission under psychiatry for further management, of which half of them could be admitted directly from emergency. For the remaining half, either there was a refusal for admission by attendants or other logistic aspects such as non-availability of beds which precluded admission; however, these patients were advised for subsequent admission or appropriate referrals were made for other centres.
The findings have several important implications for organization of PES in general hospital settings. This study emphasizes the need to optimize emergency mental healthcare and develop better service delivery models. There is a need to strengthen resources and workforce training (including emergency medical officers, nursing staff, resident doctors and ancillary workers) on how to handle some of the commonly presenting mental health conditions.
The present study has limitations. The findings from one centre may not be generalizable to other settings or regions. It is possible that some cases of anxiety, depressive or somatic complaints may have been missed or may have been managed by emergency medical officers themselves, not requiring a psychiatric referral in the ED.[22],[23] The study being retrospective could not capture some of the mental health parameters, including the follow-up status.
Conclusion
Our findings add relevant and useful information on psychiatric emergencies catered by the psychiatry department of a tertiary care hospital in India.
Acknowledgements
We acknowledge Dr S .K. Khandelwal, former Professor and Head, Department of Psychiatry for his guidance. We also acknowledge the help of the residents and faculty on-call for their help and support.
Conflicts of interest. None declared
| 1. | Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry 2016;3:171-8. [Google Scholar] |
| 2. | Sudarsanan S, Chaudhury S, Pawar AA, Salujha SK, Srivastava K. Psychiatric emergencies. Med J Armed Forces India 2004;60:59-62. [Google Scholar] |
| 3. | Zeller SL, Rieger SM. Models of psychiatric emergency care. Curr Emerg Hosp Med Rep 2015;3:169-75. [Google Scholar] |
| 4. | Nadkarni A, Hanlon C, Bhatia U, Fuhr D, Ragoni C, de Azevedo Perocco SL, et al. The management of adult psychiatric emergencies in low-income and middle-income countries: A systematic review. Lancet Psychiatry 2015;2:540-7. [Google Scholar] |
| 5. | Barratt H, Rojas-García A, Clarke K, Moore A, Whittington C, Stockton S, et al. Epidemiology of mental health attendances at emergency departments: Systematic review and meta-analysis. PLoS One 2016;11:e0154449. [Google Scholar] |
| 6. | Grover S, Sarkar S, Bhalla A, Chakrabarti S, Avasthi A. Demographic, clinical and psychological characteristics of patients with self-harm behaviours attending an emergency department of a tertiary care hospital. Asian J Psychiatr 2016;20:3-10. [Google Scholar] |
| 7. | Garekar H, Bhargava M, Verma R, Mina S. Aggression and psychosis in patients seeking emergency psychiatric care in New Delhi, India. Int J Emerg Ment Health HumResil 2015;17:616-17. [Google Scholar] |
| 8. | Sidana A, Sharma RP, Chavan BS, Arun P, Raj L. Psychiatric profile of patients attending General Emergency room services—a prospective study. J Ment Health Hum Behav 2009;14:80-3. [Google Scholar] |
| 9. | Kelkar DK, Chaturvedi SK, Malhotra S. A study of emergency psychiatric referrals in a teaching general hospital. Indian J Psychiatry 1982;24:366-9. [Google Scholar] |
| 10. | Adityanjee, Mohan D, Wig NN. Determinants of emergency room visits for psychological problems in a general hospital. Int J Soc Psychiatry 1988;34:25-30. [Google Scholar] |
| 11. | Saddichha S, Vibha P, Saxena MK, Methuku M. Behavioral emergencies in India: A population based epidemiological study. Soc Psychiatry Psychiatr Epidemiol 2010;45:589-93. [Google Scholar] |
| 12. | Saddichha S, Vibha P. Behavioral emergencies in India: Would psychiatric emergency services help? Prehosp Disaster Med 2011 ;26:65-70. [Google Scholar] |
| 13. | Murthy P, Malathesh BC, Kumar CN, Math SB. Mental health and the law: An overview and need to develop and strengthen the discipline of forensic psychiatry in India. Indian J Psychiatry 2016;58: S181-S186. [Google Scholar] |
| 14. | Vincent A, Bien CG. Anti-NMDA-receptor encephalitis: A cause of psychiatric, seizure, and movement disorders in young adults. Lancet Neurol 2008;7:1074-5. [Google Scholar] |
| 15. | Zeller SL. Treatment of psychiatric patients in emergency settings. Prim Psychiatry 2010;17:35-41. [Google Scholar] |
| 16. | Larkin GL, Beautrais AL, Spirito A, Kirrane BM, Lippmann MJ, Milzman DP, et al. Mental health and emergency medicine: A research agenda. Acad Emerg Med 2009;16:1110-19. [Google Scholar] |
| 17. | Kate N, Grover S, Kulhara P, Nehra R. Supernatural beliefs, aetiological models and help seeking behaviour in patients with schizophrenia. Ind Psychiatry J 2012;21: 49-54. [Google Scholar] |
| 18. | Kapur N, Cooper J, Hiroeh U, May C, Appleby L, House A, et al. Emergency department management and outcome for self-poisoning: A cohort study. Gen Hosp Psychiatry 2004;26:36-41. [Google Scholar] |
| 19. | McNiel DE, Binder RL. Psychiatric emergency service use and homelessness, mental disorder, and violence. Psychiatr Serv 2005;56:699-704. [Google Scholar] |
| 20. | WHO. mhGAP Intervention Guide for Mental, Neurological, and Substance use Disorders in Non-Specialized Settingss: Mental Health Gap Action Programme (mhGAP) — Version 2.0. Geneva:World Health Organization; 2016. [Google Scholar] |
| 21. | Stowell KR, Florence P, Harman HJ, Glick RL. Psychiatric evaluation of the agitated patient: Consensus statement of the American association for emergency psychiatry project Beta psychiatric evaluation workgroup. West J Emerg Med 2012; 13:11-16. [Google Scholar] |
| 22. | Trivedi JK, Gupta AK. A study of patients attending emergency out-patient services of a large teaching institution. Indian J Psychiatry 1982;24:360-5. [Google Scholar] |
| 23. | Larkin GL, Claassen CA, Emond JA, Pelletier AJ, Camargo CA. Trends in U.S. Emergency department visits for mental health conditions, 1992 to 2001. Psychiatr Serv 2005;56:671-7. [Google Scholar] |
Fulltext Views
3,284
PDF downloads
1,557




