Translate this page into:
Metreleptin replacement treatment improves quality of life and psychological well-being in congenital generalized lipodystrophy
2 Erenkoy Mental and Neurological Diseases Training and Research Hospital, Istanbul, Turkey
3 Division of Endocrinology and Metabolism Disorders, Dokuz Eylul University Medical Faculty, Izmir, Turkey
Corresponding Author:
Ilgin Yildirim Simsir
Division of Endocrinology and Metabolism Disorders, Ege University Medical Faculty, 35100 Izmir
Turkey
ilginyildirim@hotmail.com
| How to cite this article: Simsir IY, Yurekli BS, Polat I, Saygili F, Akinci B. Metreleptin replacement treatment improves quality of life and psychological well-being in congenital generalized lipodystrophy. Natl Med J India 2020;33:278-280 |
Abstract
The near total lack of subcutaneous fat in congenital generalized lipodystrophy (CGL) leads to the accumulation of fat in ectopic organs and severe insulin resistance, which are associated with serious metabolic abnormalities. Cosmetic aspects of the disease are likely to affect the quality of life (QoL) and physiological well-being in these individuals. Metreleptin, recombinant human leptin, replacement treatment has been shown to have benefits in treating the metabolic abnormalities of CGL. In a patient with CGL caused by a homozygous AGPAT2 pathogenic variant, we examined QoL and mood alterations (depression and anxiety) caused by this chronic disease. Metreleptin replacement treatment led to dramatic metabolic improvement in our patient. It was also was associated with improvements in QoL, depression and anxiety scores. We suggest that there is need for studies to document the benefit of metreleptin replacement treatment on QoL and physiological well-being in patients with CGL.Introduction
Congenital generalized lipodystrophy (CGL) is a group of rare diseases characterized by near total loss of subcutaneous fat starting at birth and is diagnosed based on specific clinical signs.[1] CGL is associated with accumulation of fat in ectopic organs and severe insulin resistance that cause serious metabolic abnormalities. The causes of morbidity and mortality associated with CGL include long-term complications of uncontrolled diabetes, attacks of pancreatitis associated with hypertri-glyceridaemia, hepatic steatosis that can lead to cirrhosis, atherosclerotic vascular disease and renal failure.[2],[3] In addition to standard medical care, metreleptin replacement therapy is the only available treatment option to prevent such metabolic complications, which can lead to premature death.[4]
Patients with lipodystrophy can develop psychological disturbances associated with the need for continuous treatment as well as cosmetic issues related to fat loss, particularly in the face and other subcutaneous areas, or ectopic fat accumulation.[5] In addition to metabolic complications, cosmetic problems, which are usually considered somewhat less important by clinicians, are a cause of impairment in the patient’s quality of life (QoL). We did a detailed evaluation of physiological well-being, which primarily focuses on symptoms of depression and anxiety, in a patient with CGL before and after metreleptin treatment, as well as the change in her QoL.
Method
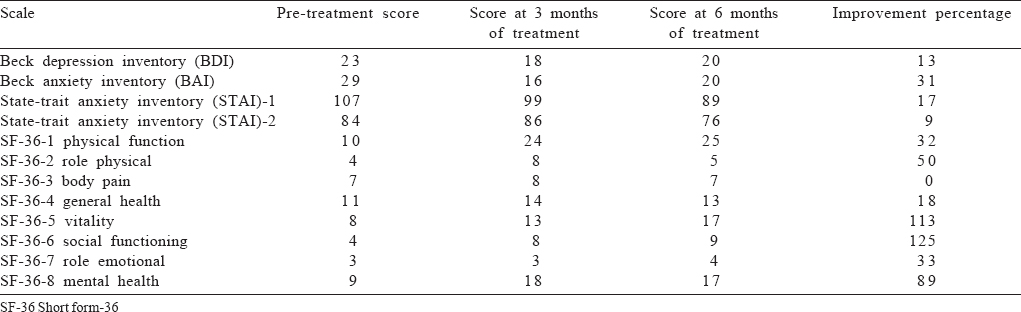
Beck Depression Inventory (BDI), State-Trait Anxiety Inventory (STAI) and Short Form-36 (SF-36) were applied before and at the third and sixth months of metreleptin treatment. Validation and reliability studies of the Turkish versions of these evaluation tools have been previously published.[6],[7],[8] Depressive symptoms were assessed with BDI, a self-assessment scale composed of 21 items for assessing characteristic attitude and depression symptoms. The scale’s cut-off point was reported as 17.[7] Anxiety symptoms were assessed with STAI, a scale to determine state anxiety and trait anxiety levels. Principal properties evaluated with this tool are feelings of perturbation, nervousness, irritability and anxiety.[8] Patient’s QoL was assessed with SF-36. SF-36 is a self-filled scale composed of eight subscales, and there is no cut-off point. Its subscales are physical functioning, social functioning, role limitations due to physical health, role limitations due to emotional problems, mental health, energy/vitality, pain and general health perception. Subscales evaluate health on a scale of 100, where 0 means poor health and 100 means good health state.[6]
The Case
A 20-year-old female was admitted to our clinic with acute pancreatitis secondary to hypertriglyceridaemia and in a hyper-osmolar hyperglycaemic state. The patient had been diagnosed with diabetes mellitus (DM) at the age of 14 and hyperlipidaemia at 17. Several aspects of the patient’s history, including no history of ketoacidosis during hyperglycaemic episodes, being diagnosed with DM at a young age and not being overweight, the presence of hypertriglyceridaemia, and examination findings of near total lack of adipose tissue in the whole body led us to suspect lipodystrophy. A homozygous AGPAT2 (c.144 hom C>A; p. C48X) pathogenic variant was detected and the patient was diagnosed with CGL.
The patient was 167 cm tall, 55 kg in weight and her body mass index (BMI) was 19.7 kg/m2 at initial examination. She was managed with standard medical treatment to keep her triglyceride level <500 mg/dl. In addition to omega-3 and gemfibrozil, the patient received atorvastatin with consideration of myopathy risk. Plasmapheresis was also used during acute pancreatitis. For regulation of blood glucose, the patient received metformin 2 g/day, pioglitazone 30 mg/day and insulin 198 i.u./day. Her haemoglobin A1c (HbA1c) level was 14.4% despite being treated with relatively high doses of insulin and with good treatment compliance. Her lipid levels were also far above target values despite treatment with multiple lipid-lowering agents.
Metreleptin replacement
Metreleptin treatment was started at a dose of 5 mg once a day as a part of an early access programme, which resulted in dramatic improvement in her metabolic control and profound reduction in insulin requirement. Her proteinuria reduced to 2.1 g/day from 15.2 g/day. The reduction in the size of her palpable liver under the right costal margin was considered as an indirect sign of reduced hepatosteatosis. Magnetic resonance imaging studies showed a reduction in liver size from 270 to 222 mm at 6 months, and the reduction in hepatosteatosis was apparent in dual phase and spectroscopy as well. Her appetite decreased weeks after metreleptin, and her excessive sweating, a sign of increased metabolic activity, disappeared. Metreleptin treatment resulted in improvements in beta cell function indices. Except for a lower urinary tract infection that occurred once, no adverse reactions were observed. At the sixth month of treatment, the patient weighed 48.3 kg and her BMI was 17.3 kg/m2. She did not require any plasmapheresis after metreleptin treatment. She was never non-compliant. On her latest visit, we observed that HbA1c remained at target levels after discontinuing insulin for 2 months. We observed a dramatic decrease in proteinuria which was at extreme levels before treatment.
Assessment of physiological well-being and quality of life
In the evaluation before the initiation of metreleptin treatment, the patient had a score of 23 on BDI. This score was above the cut-off score, indicating the presence of mild depressive symptoms. Patient’s BDI score at the third month of treatment was 18, a 22% improvement in depression symptoms. A slight increase was observed in the patient’s BDI score at the sixth month of treatment, and overall improvement in symptoms compared to the baseline was calculated as 13% at the sixth month of treatment.
The patient’s state of anxiety subscale score of STAI reduced from the pre-treatment value of 107 to 99 at the third month and 89 at the sixth month of treatment. The improvement was calculated as 7% at month 3 and 17% at month 6. The reduced scores suggest a tendency of the anxiety state to improve during the treatment. Patient’s trait anxiety score was 84 before treatment, 86 at the third month and 76 at the sixth month of treatment. Calculated improvement rate at the sixth month of treatment was 9%.
Short Form-36 revealed physical functioning scores that showed 26.6% improvement at the third month and 32% improvement at the sixth month of treatment. Social functioning scores improved more than two-fold. Scores of role limitations due to physical health subscale showed 100% improvement at the third month and 50% improvement at the sixth month. Scores of role limitations due to emotional problems subscale improved by 33%, general health perception scores improved by 18%, vitality score improved by 113% (more than two-fold) and mental health scores improved by 89%, whereas no change was observed in the pain subscale scores [Table - 1].
Discussion
Metreleptin improved glycaemic control[9] and this may have contributed to improve the psychological profile of this patient. In addition to dramatic metabolic improvements after metreleptin replacement treatment, we observed considerable improvements in different components of QoL in CGL. Physical and social function scores improved. Our patient also benefited from metreleptin replacement treatment in terms of mental health. These favourable results need to be confirmed in other patients who are on continuous long-term metreleptin replacement treatment.
There is limited and controversial information regarding the relationship between mood and leptin level/signalling in humans. Improvements in depression symptoms with activation of hippocampal leptin receptors through leptin treatment have been previously shown.[10] On the other hand, both leptin deficiency and resistance can contribute to mood changes. Higher leptin levels have been observed in depressed individuals,[11],[12] which might reflect an association between increased adiposity and depression.[13]
Because lipodystrophy is a rare disease, it is difficult to obtain sufficient and satisfactory information about the treatment and its psychological effects. Several studies have shown an association between leptin deficiency and depression in animals and humans, and leptin treatment has been reported to have antidepressant effects in rodents.[14],[15] Our experience suggests that patients with lipodystrophy are likely to benefit from metreleptin treatment by means of physiological well-being. There was a decline in depression scores just after 3 months of treatment. Anxiety score also improved but anxiety is influenced by the conditions that the individual experiences and usually varies according to the personality type. Therefore, it is hard to reach a conclusion regarding the association of our data with metreleptin treatment. The identification of intracellular signalling pathways and key brain areas that mediate the antidepressant activity of leptin may provide new insight into the pathogenesis of depression.[14] In this sense, lipodystrophy may provide guidance, as a model disorder, to study the effects of leptin on depression and anxiety and signalling pathways of leptin in the central nervous system since obesity or leptin resistance is not a confounding factor in this clinical setting.
Conclusion
As diminished physiological well-being is an important factor that may deteriorate the clinical course of CGL, this chronic disease itself can also cause depressive symptoms and anxiety. In our patient, depressive symptoms, anxiety and QoL improved following metreleptin replacement treatment. Further studies are needed to document the benefits of long-term metreleptin replacement on QoL and physiological well-being in a large number of patients with CGL.
Acknowledgements
Metreleptin used in this patient was obtained through an early access programme without any reimbursement paid by any local or national authority.
Conflicts of interest. None declared
| 1. | Garg A. Acquired and inherited lipodystrophies. N Engl J Med 2004;350:1220–34. [Google Scholar] |
| 2. | Garg A. Clinical review#: Lipodystrophies: Genetic and acquired body fat disorders. J Clin Endocrinol Metab 2011;96:3313–25. [Google Scholar] |
| 3. | Garg A, Misra A. Lipodystrophies: Rare disorders causing metabolic syndrome. Endocrinol Metab Clin North Am 2004;33:305–31. [Google Scholar] |
| 4. | Chan JL, Oral EA. Clinical classification and treatment of congenital and acquired lipodystrophy. Endocr Pract 2010;16:310–23. [Google Scholar] |
| 5. | Sanches RS, Mill J, Machado AA, Donadi EA, Morais Fernandes AP. Facial lipoatrophy: Appearances are not deceiving. J Assoc Nurses AIDS Care 2009; 20:169–75. [Google Scholar] |
| 6. | Kocyigit H, Aydemir O, Fisek G, Olmez N, Memis A. [Reliability and validity of Turkish version of Short Form-36 (SF-36)]. İlac ve Tedavi Dergisi 1999;12: 102–6. [Google Scholar] |
| 7. | Hisli N. [A study on the validity of Beck Depression Inventory]. Turk Psikoloji Dergisi 1988;6:118–26. [Google Scholar] |
| 8. | Oner N, Le Compte WA. [State-Trait Anxiety Inventory Handbook]. Istanbul: Bogazici Universitesi Yayinlari; 1985. [Google Scholar] |
| 9. | Simsir IY, Yurekli BS, Saygili F, Altay C, Akinci B. First metreleptin treatment for generalized lipodystrophy in Turkey. Diabetes Obes Metab 2017;19:299–301. [Google Scholar] |
| 10. | Lu XY, Kim CS, Frazer A, Zhang W. Leptin: A potential novel antidepressant. Proc Natl Acad Sci U S A 2006;103:1593–8. [Google Scholar] |
| 11. | Pasco JA, Jacka FN, Williams LJ, Henry MJ, Nicholson GC, Kotowicz MA, et al. Leptin in depressed women: Cross-sectional and longitudinal data from an epidemiologic study. J Affect Disord 2008;107:221–5. [Google Scholar] |
| 12. | Gecici O, Kuloglu M, Atmaca M, Tezcan AE, Tunckol H, Emül HM, et al. High serum leptin levels in depressive disorders with atypical features. Psychiatry Clin Neurosci 2005;59:736–8. [Google Scholar] |
| 13. | Morris AA, Ahmed Y, Stoyanova N, Hooper WC, De Staerke C, Gibbons G, et al. The association between depression and leptin is mediated by adiposity. Psychosom Med 2012;74:483–8. [Google Scholar] |
| 14. | Lu XY. The leptin hypothesis of depression: A potential link between mood disorders and obesity? Curr Opin Pharmacol 2007;7:648–52. [Google Scholar] |
| 15. | Garza JC, Guo M, Zhang W, Lu XY. Leptin restores adult hippocampal neurogenesis in a chronic unpredictable stress model of depression and reverses glucocorticoid-induced inhibition of GSK-3â/â-catenin signaling. Mol Psychiatry 2012;17:790–808. [Google Scholar] |
Fulltext Views
1,755
PDF downloads
276




