Translate this page into:
Opioid use disorder: Long-term use of oral naltrexone for promoting abstinence
[To cite: Kabra V, Jadeer M, Sarkar S. Opioid use disorder: Long-term use of oral naltrexone for promoting abstinence. Natl Med J India 2024;37: 358–9. DOI: 10.25259/NMJI_950_2024]
Naltrexone is an opioid antagonist that has clinical potential for use in patients with opioid dependence. While long-term use of opioid agonists such as buprenorphine and methadone has been well described, there is a lack of evidence of the long-term outcomes of patients being put on naltrexone.1,2 We describe a patient with opioid dependence who has been treated with oral naltrexone for about 8 years.
An 18-year-old male came to us in 2016 with opioid, cannabis, and tobacco dependence for 6 months, 3 years, and 5 years, respectively. He had behavioural disturbances, muttering to self, sexually inappropriate behaviour, and grandiosity for 6 months at the time of presentation. He was detoxified and started on oral naltrexone 50 mg per day (based on stated preference for opioid-free lifestyle), and olanzapine 10 mg was started for psychiatric symptoms which were remitted. Over the next 3 years, he did not relapse back to opioid regular use, though he stopped naltrexone for 5–6 days and tried heroin on 2 such occasions. However, each time his parents were vigilant and brought him to the outpatient services to restart naltrexone. Later, he tried heroin on 3–4 occasions but did not experience a high on consuming it as he was on regular naltrexone, supervised properly by family members. In 2017 he again had heightened psychomotor activity, decreased need for sleep, grandiose ideation, verbal and physical aggression toward family members, as well as muttering, giggling, and sexual disinhibition. The onset of symptoms was not related to the use of any specific substance such as cannabis. He was admitted, olanzapine was started and resolution of symptoms occurred in 14 days. Naltrexone was continued. Subsequently, in 2018, he presented with delusions of reference and persecution, followed by social withdrawal and then catatonia. Again, olanzapine 10 mg was started and the patient improved over the course of 5 weeks. An additional diagnosis of schizophrenia was the most tenable based on the psychiatric history.
The patient over the course of time took oral naltrexone and olanzapine regularly (Fig. 1). He was gainfully engaged in the family business, changed peer groups to avoid substance-using peers, and joined a gymnasium to pay attention to his physical health. He relapsed to regular cannabis use subsequently and was admitted for a period ranging from 7 to 10 days for cessation of cannabis on four occasions between 2019 and 2023. He was admitted in 2024 when he reported consuming alcohol very frequently (5–6 drinks, 3–4 times a week) and acknowledging gradually losing control over drinking. His admission helped in the cessation of alcohol use, and again the possibility of stopping naltrexone was discussed. Even after 5 years of complete abstinence from opioid use, the patient willingly wanted to continue using oral naltrexone regularly, as he felt it safeguarded him against situations of peer influence and negative emotional state when he was likely to relapse. Regular use of olanzapine also seemingly ensured a lack of recurrence of psychotic symptoms. This suggests that stability in cases of psychosis can be effectuated with good compliance to antipsychotics. Dual diagnosis, i.e. the co-occurrence of substance use disorder and psychiatric disorder is a common occurrence in the clinical setting.
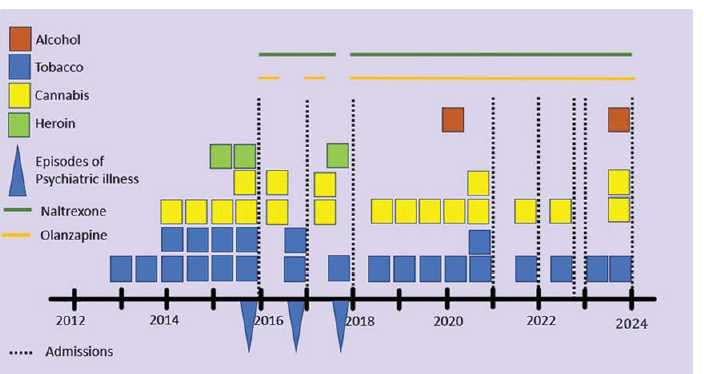
- Life course of the patient
This case illustrates that long-term naltrexone can help some patients on their road to recovery from opioid use disorders. Naltrexone is reported as the fourth most effective treatment option for the treatment of opioid use disorder.3 Naltrexone is a particularly suitable option for patients who require an opioid-free lifestyle.4,5 This case also highlights the importance of retention in treatment, supervision by family members, and the potential of naltrexone in achieving and sustaining abstinence from opioids. By providing effective treatment and support, we can help individuals reclaim their functional lives and respect in society and overcome the challenges of living with addiction.
References
- Long term outcomes of pharmacological treatments for opioid dependence: Does methadone still lead the pack? Br J Clin Pharmacol. 2014;77:272-84.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment retention among patients randomized to buprenorphine/naloxone compared to methadone in a multi-site trial. Addiction. 2014;109:79-87.
- [CrossRef] [PubMed] [Google Scholar]
- Relative effectiveness of medications for opioid-related disorders: A systematic review and network meta-analysis of randomized controlled trials. PLoS One. 2022;17:e0266142.
- [CrossRef] [PubMed] [Google Scholar]
- Naltrexone for probationers and parolees. J Subst Abuse Treat. 2006;31:107-11.
- [CrossRef] [PubMed] [Google Scholar]
- Successful use of naltrexone in addicted physicians and business executives. Adv Alcohol Subst Abuse. 1984;4:89-96.
- [CrossRef] [PubMed] [Google Scholar]




