Translate this page into:
Optimal anthropometric measures to predict incidence of coronary heart disease in adults in Turkey
2 Department of Cardiology, Cerrahpasa Medical Faculty, Istanbul University-cerrahpasa, Istanbul, Turkey
3 Biochemistry Section, Cardiology Institute, Istanbul University, Turkey
4 Department of Cardiovascular Surgery, Siyami Ersek Center for Cardiovascular Surgery, Istanbul, Turkey
Corresponding Author:
Günay Can
Department of Public Health, Cerrahpasa Medical Faculty, Istanbul University-cerrahpasa, Istanbul
Turkey
gunaycan09@yahoo.fr
| How to cite this article: Can G, Onat A, Sayili U, Hayiroglu MI, Ademoglu E, Yurtseven E. Optimal anthropometric measures to predict incidence of coronary heart disease in adults in Turkey. Natl Med J India 2019;32:334-341 |
Abstract
Background. We aimed to identify the most suited anthropometric measure for the prediction of risk for incident coronary heart disease (CHD) among the Turkish population.Methods. We collected data on body mass index, waist circumference (WC), hip circumference, waist-to-hip ratio (WHR), waist-to-height ratio (WHtR) and a body shape index. We analysed these using both C-statistics and Cox regression models adjusted for age, systolic blood pressure, glucose and high-density lipoprotein (HDL)-cholesterol for assessing risk of incident CHD among 3203 Turkish Adult Risk Factor (TARF) study participants (mean [SD] age 48.5 [11] years).
Results. Over a mean follow-up of 9.93 years, new CHD developed in 573 individuals. Multi-adjusted C-statistics were highest for WHtR followed by WC, in both sexes. Except WHR, all measures were significantly associated with incident CHD in combined sexes in the full model. There was a sex difference, however, in the mediation of the three risk factors for adiposity; these attenuated hazard ratios (HRs) in males, whereas in females, significant prediction of incident CHD persisted for each measure. WC (HR 1.36 [95% CI 1.13; 1.64]), followed by WHtR (HR 1.24 [95% CI 1.10; 1.40]), were in combined sex, as in females, the most informative surrogates of adiposity. Hip circumference did not protect, but rather conferred modest CHD risk, especially in females, rendering a low utility of predictive value for WHR. The CHD risk curve did not have a J shape.
Conclusions. WC is the most suitable of five adiposity surrogates for CHD risk among Turkish adults, while in males, unmediated adiposity risk was similarly identified by WHtR. Retention of the large part of CHD risk in females perhaps reflects the underlying autoimmune activation.
Introduction
Waist circumference (WC) and waist-to-hip ratio (WHR) are recognized as better indicators of abdominal obesity than body mass index (BMI) as they have a stronger correlation with intra-abdominal fat content and cardiometabolic risk factors.[1],[2],[3],[4] Waist-to-height ratio (WHtR), investigated in fewer studies,[1],[2],[3],[4],[5],[6] also appears to be better than BMI. Despite this, BMI is the most commonly used measure of body fat worldwide.[7]
In the Nurses' Health study, the WHtR was comparable to WC and WHR, but superior to BMI, for the prediction of the incidence of coronary artery disease (CHD) among over 45 000 middle-aged females predominantly of Caucasian origin.[5] It has been established that measures of abdominal adiposity are predictive of CHD independent of BMI in females.[8] A metaanalysis of over 300 000 individuals has indicated that WHtR may be superior in predicting cardiometabolic risk.[4] Compared with BMI, WC improved the discrimination of adverse outcomes by 3% and WHtR improved by 4%–5%. Within-study difference in area under the curve (AUC) showed WHtR to be significantly better than WC for diabetes, hypertension, cardiovascular disease (CVD) and all outcomes in males and females.
In the PRIME study among 10 600 middle-aged French and Irish males, WHtR identified CHD risk more strongly than WC, WHR or BMI, though the difference was marginal.[9] In 24 508 middle-aged males and females of the EPIC-Norfolk cohort, followed up over 9.1 years, the indices of abdominal obesity (WHR and WC) had stronger predictive value for incident CHD risk than BMI, especially in females. Hazard ratios (HRs) for hip circumference (HC) increment were significant.[10]
Turkish adults have the following distinctive features. Metabolic syndrome (MetS) is common in both sexes[11] and is rising, as is type-2 diabetes,[12] both conditions being associated with obesity. Low-grade inflammation is more pronounced in females than males.[13]
In search of a more appropriate measure between BMI and WC for the prediction of CHD risk, the Turkish Adult Risk Factor (TARF) study reported in 2007 that the risk for CHD independently imparted by a higher WC in males was essentially mediated by the associated atherogenic dyslipidaemia and elevated blood pressure (BP).[14] In females, multi-adjusted relative risks for dyslipidaemia, elevated BP, MetS and CHD rose sharply and asymptomatically from WC ≥83 cm.[15] However, head-to-head comparison of various adiposity indicators in relation to incident CHD risk over a relatively long period of follow-up (nearly 600 new CHD cases) has not been done among the Turkish population.
We therefore investigated six anthropometric measures in relation to incident CHD risk among Turkish adults to identify the most appropriate measure for both sexes. We also studied the adiposity–CHD risk association in 3203 participants over a mean follow-up period of 9.93 years.
Methods
Study sample
The TARF study is a prospective cohort study on the prevalence of cardiac disease and risk factors in adults in Turkey carried out biennially since 1990 in 59 communities scattered in all the geographical regions of the country.[16] It comprises a random sample of the Turkish adult population, representatively stratified for sex, age, geographical regions and for rural–urban distribution. New random recruitment forming 15% of the study sample was done in 2002–03 and 2007–08. The survey conducted in 1997–98 was selected as baseline because high-density lipoprotein (HDL)-cholesterol and WC were done first at that time. Our study sample did not include individuals who had CHD at baseline (n= 182) or had died prior to the baseline (n=26), and 616 participants with a follow-up of <2 years. Participants numbering 3203 composed the cohort of the current study. The study was approved by the ethics committee of the Medical Faculty of Istanbul University. Written informed consent for participation was obtained from all participants. Data were obtained by using a questionnaire for the past years, physical examination of the cardiovascular system, sampling of blood and recording a resting 12-lead electrocardiogram.
Measurement of risk factors
BP was measured with an aneroid sphygmomanometer (Erka, Bad Tölz, Germany) in the sitting position on the right arm, and the mean of two recordings 5 minutes apart was recorded. Height was measured without shoes using a measuring stick and weight was measured without shoes in light indoor clothes using a scale. WC was measured at the level midway between the lower rib margin and the iliac crest. We measured HC, which is the widest diameter on the hip, using the trochanter majors as the reference point. Physical activity was graded by the participant himself/herself into four categories of increasing order with the aid of a scheme.[16] Cigarette smoking status was categorized into never, former and current smokers. Anyone who reported the use of alcoholic beverages once a week or more was considered as an alcohol user.
Blood samples were collected, spun at 1000 g, shipped to Istanbul and stored at –75 °C, until analysed within weeks. Serum concentrations of glucose, total cholesterol, fasting triglycerides, low-density lipoprotein (LDL)-cholesterol and HDL-cholesterol were determined using the Cobas 500 autoanalyser (Roche Diagnostic GmbH, Germany).
Definitions
Five obesity indicators were selected to predict CHD risk: BMI, WC, HC, WHR, WHtR and a body shape index (ABSI).[17]
Diagnosis of CHD was based on the presence of angina pectoris, of a history of myocardial infarction with or without accompanying Minnesota codes of the electrocardiogram (ECG)[17] or a history of myocardial revascularization. Typical angina and, in females, age >45 years were a prerequisite for a diagnosis when angina was isolated. ECG changes of ‘ischaemic type’ of greater than minor degree (Codes 1.1–2, 4.1–2, 5.1–2 and 7.1) were considered as myocardial infarct sequelae or myocardial ischaemia. A fatal coronary event comprised death from heart failure of coronary origin.
Data analysis
Descriptive parameters are reported as mean (SD) or in percentages. For variables with skewed distribution, values derived from log-transformed (geometric) means were used. In variables with skewed distribution, Mann–Whitney U-test was applied. Two-sided t-tests and Pearson's Chi-square tests were used to analyse the differences between means and proportions of two groups. Cut-offs for quintile 4 in males/females, respectively, were as follows: WC 98.8–103.0/94.0–102.0 cm; BMI 27.7–30.0/30.2–33.7 kg/m2; and WHtR 0.575–0.611/0.606–0.658. Analyses for area under AROC were performed, both unadjusted and adjusted for four major cardiovascular risk factors, for predicting incident CHD in each sex using Cox regression.
Cox proportional hazard regression analyses of the anthropometric measures for CHD risk were performed in models that adjusted for age and further for mediating factors (systolic BP [SBP], HDL-cholesterol and glycaemia). The hazard ratios (HRs) for CHD risk were estimated and expressed each in terms of 1-SD increment. This applied to the log-transformed SDs of 7.6%/9.4% for WHR and 12.0%/15.5% for WtHR in males/ females, respectively. Residual adiposity risk was estimated as percentage of excess risk mediated by the three risk factors deducted from the excess risk of the adiposity measure. A value of p<0.05 on two-tailed test was considered statistically significant. Statistical analyses were performed using SPSS-10 for Windows.
Results
Females made up 1636 of 3203 (51.1%) participants of the study. The mean (SD) age of males and females was 48.7 (11) years and 48.3 (11) years, respectively. The mean (SD) follow-up was 9.86 (4.7) years in males and 9.99 (4.6) years in females. CHD incidence (in 573 cases) was 19.6 per 1000 person-years in males and 19.7 per 1000 person-years in females.
Males and females who developed CHD were 6.1 and 6.6 years, respectively, older and were roughly 2 cm shorter in height and had 11.3/5 and 16/6.4 mmHg higher BP [Table - 1]. All the reported biomarkers were significantly different among females with the exception of serum HDL-cholesterol and fasting glucose in males. Smoking habit and the prevalence of alcohol use were similarly distributed in the two groups in each sex, and low physical activity was significantly higher among males who developed incident CHD, but not in females.
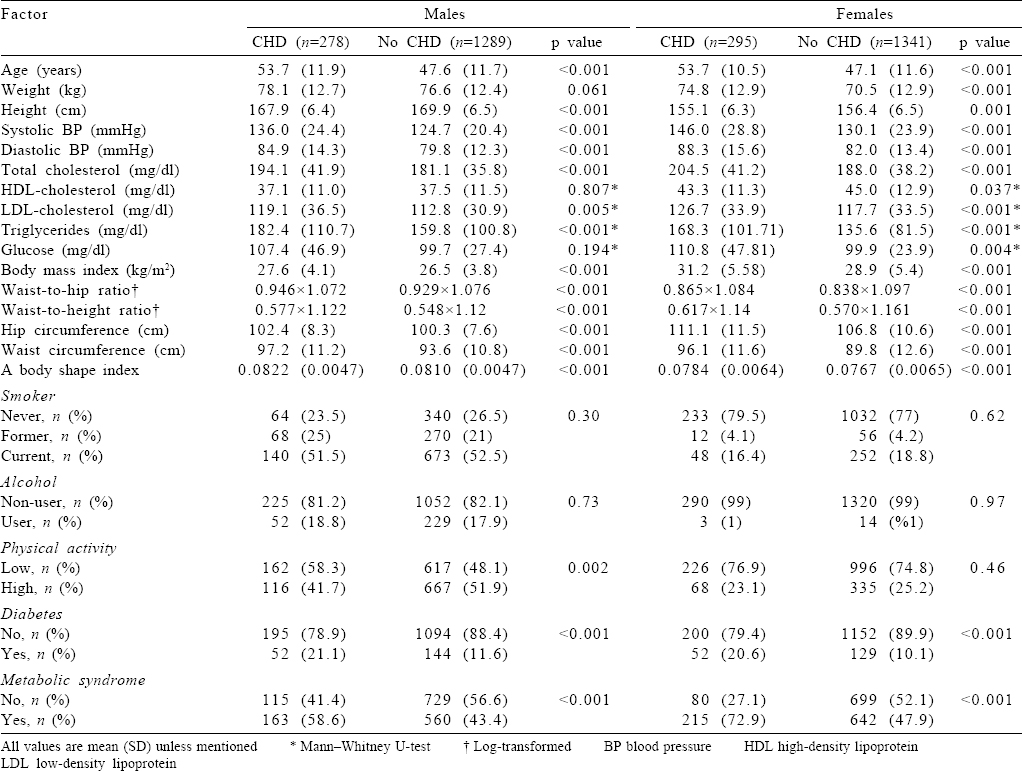
Of the six anthropometric measures, all, including the HC, were significantly wider among those who subsequently developed CHD in each sex. The difference of WC was 3.6 cm and 4.3 cm and of WHtR was 0.029 and 0.047 in males and females, respectively.
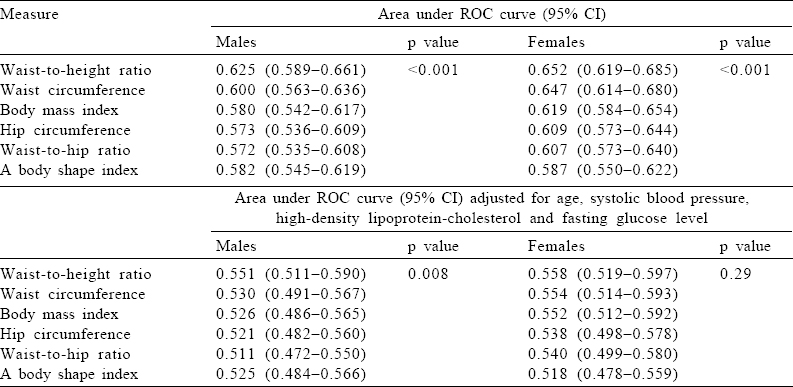
Comparison of the adiposity indicators by C-statistics
Crude area under ROC was significant for all six surrogates in each sex, being highest among males in WHtR (0.625; 95% CI 0.589–0.661) followed by WC (0.600; 95% CI 0.563–0.636). In females too this was apparent with WHtR (0.652; 95% CI 0.619–0.685) and WC (0.647; 95% CI 0.614–0.680). Multivariable-adjusted area under ROC disclosed attenuation for the anthropometric measures so that mild significance was retained in males for WHtR only and in females for WC, WHtR and BMI.
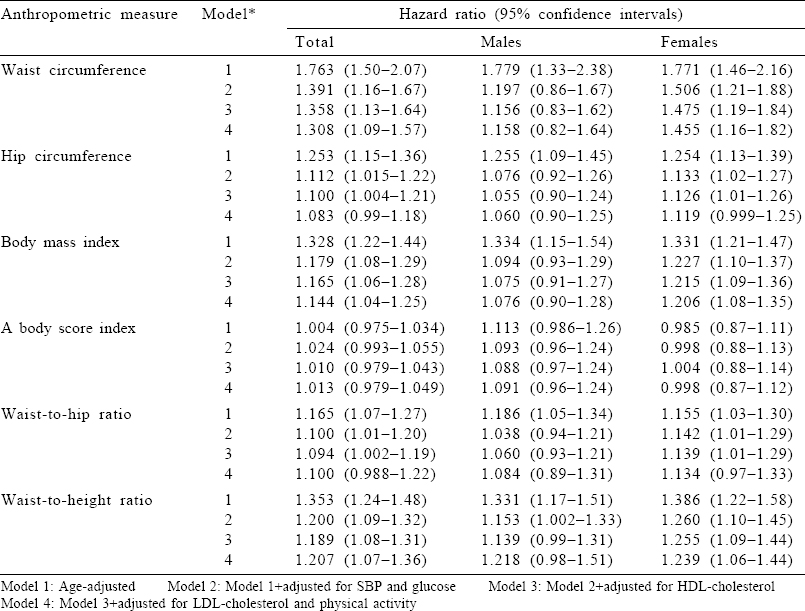
Cox regression analyses
Four models were tested, using Cox regression analyses for the association of anthropometric measures with subsequent incident CHD [Table - 3], each adjusted for age (Model 1), further for SBP and glucose (Model 2), additionally for HDL-cholesterol (Model 3) and further for LDL-cholesterol and physical activity (Model 4). WC, BMI and WHtR were significantly associated with incident CHD in both sexes in the full model. However, a sex difference was apparent as in males all adiposity measures that were significantly associated in the age-adjusted model attenuated in the full model except for WHtR in Model 2. In contrast, in females, significant prediction of incident CHD persisted for WC, BMI and WHtR in the full model as well and also borderline significance relative to HC and WHR in the full model. WC (HR 1.46; 95% CI 1.16–1.82), followed by WHtR (HR 1.24; 95% CI 1.06–1.44]), was the most informative surrogate of adiposity.
Seeking a non-linear relationship
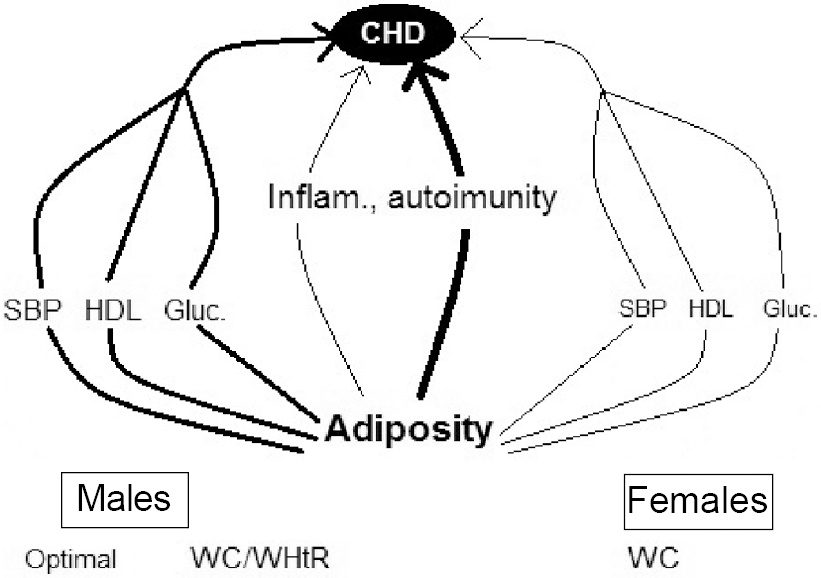
HRs of age-adjusted CHD risk were sought also in quintiles of anthropometric measures to possibly detect a J-shaped relationship [Figure - 1] and [Table - 4]. Linearity was evidenced by significant p trends in all measures in both sexes except for ABSI and WHR in men (p=0.064). An inverted U-shaped CHD risk curve was detected only in ABSI of females, although BMI quintile 4 showed a clear dip compared to Q3 and Q5. Increasing hip categories revealed rising HRs in each sex. Finally, WC and WHtR distinctly reflected the best increasing HRs, where WC was slightly superior in females and WHtR was so in males.
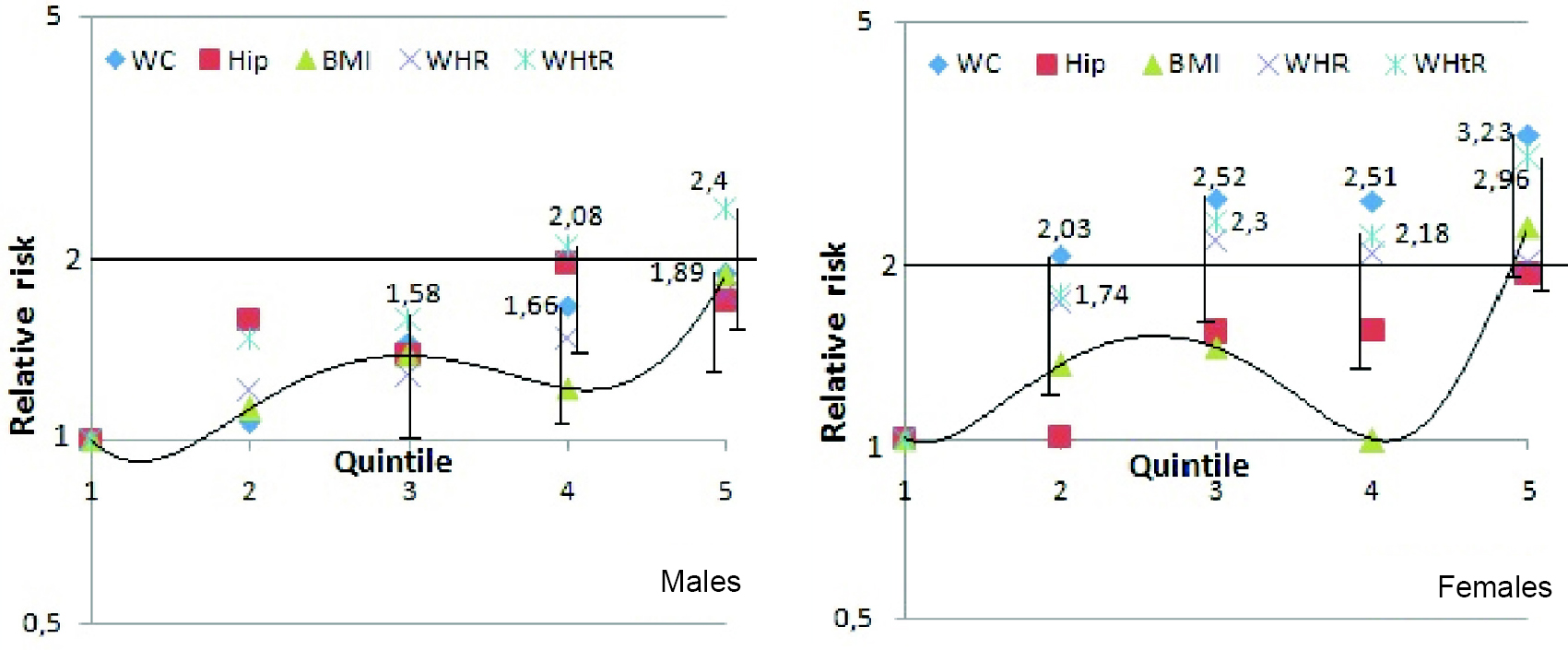 |
| Figure 1: Graph represents age-adjusted risk for coronary heart disease by quintiles of adiposity indicators in males and females. Waist circumference and waist-to-height ratio are the two most suitable measures (where significant hazard ratios are indicated with lower standard deviation bars). In contrast, body mass index has significant hazard ratios confined to the top quintile and shows a dip in hazard ratios of the 4th quintile (mean 28.7/31.8 kg/m2 body mass index in males/females) |
 |
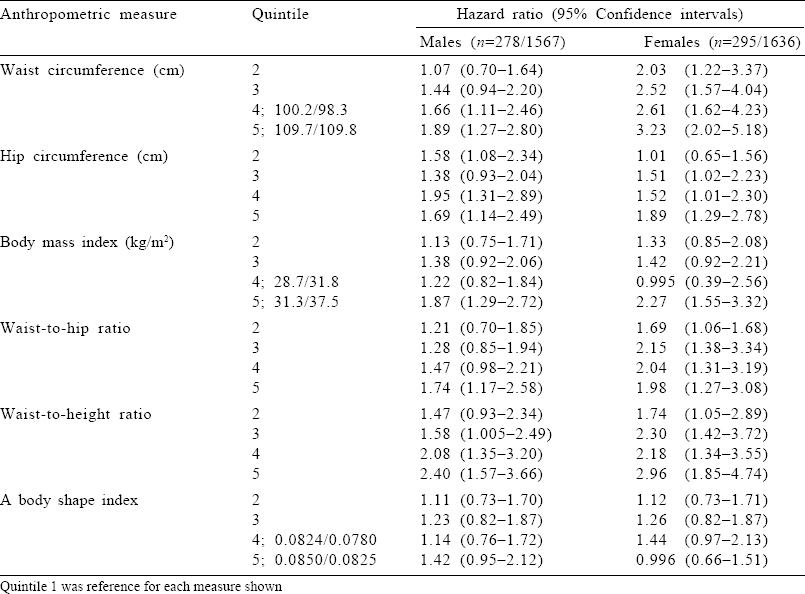
| Figure 2: Schematic representation of factors involved in imparting adiposity on risk for coronary heart disease (CHD) in Turkish adults and the mediators. Systolic blood pressure (SBP), highdensity lipoprotein-cholesterol (HDL) and fasting glucose are the major mediators in males, leaving low-grade inflammation (Inflam.) a minor role. In contrast, the stated risk factors in females assumed minor mediation, while the bulk of CHD risk was retained by excess adiposity, presumably through the autoimmune process WC waist circumference WHtR waist-to-height ratio |
Discussion
Our longitudinal study investigating the most appropriate adiposity indicator in predicting incident CHD risk among 3203 middle-aged and elderly adults showed that: (i) WC and WHtR were most suitable among six surrogates of adiposity including BMI; (ii) risk inherent to anthropometric measures was mediated differently depending on sex such that a greater extent of risk effect was mediated by conventional risk factors (SBP, glycaemia and HDL-cholesterol) in males regarding WC, thus rendering WHtR an equivalent indicator to WC in them; (iii) HC was not protective against CHD risk, but rather conferred modest risk, especially in females, rendering a lower utility of predictive value for WHR; (iv) age-adjusted ABSI was only a borderline surrogate in males and the least informative one in females, showing a non-linear relation; and (v) the CHD risk curves disclosed an inverted U shape for ABSI in females alone.
Best surrogates for risk of CHD
WC was the best indicator of absolute CHD risk insofar as the age-adjusted HR in combined sex was 1.76, compared to 1.36 for WHtR. The same ranking was valid also for the ‘fully adjusted’ model: HRs of 1.31 and 1.21, respectively, as well as in females alone. Yet when males were considered, both adiposity measures attenuated to non-significant HRs.
In the large Health Professionals Follow-up and the Nurses' Health studies with over 3000 CHD end-points over a mean follow-up of 16 years, it was concluded that WC may predict CHD risk better than BMI among males and females >60 years of age.[18] Their overall data for females were consistent with a superiority of WC compared to BMI. In post hoc analyses, they reported evidence that WC thresholds as low as 84 cm in males and 71 cm in females may be useful in identifying those at an increased risk of developing CHD.
Using computed tomography, it was found that the best surrogate of visceral adiposity was WC among the Turkish people.[19] Apolipoprotein B and HDL-cholesterol in males and, the latter in females, were independently associated with VAT area, closely related to CHD risk. A lower BMI at a given waist girth suggested higher visceral adipose tissue (VAT) in males alone. In females, a commensurate overall obesity and visceral adiposity prevailed, suggesting no preferential accumulation of subcutaneous or visceral fat tissue.
The association of abdominal subcutaneous and visceral fat volumes with CVD risk factors was evaluated by computed tomography in 1106 adults of the Third Generation cohort of Framingham study.[20] In a follow-up of 6.1 years, changes in both abdominal volumes were associated with an increased incidence of CVD risk factors, even after adjustment for changes in BMI and WC. Hypercholesterolaemia and low HDL-cholesterol were associated only with VAT but not with subcutaneous (SAT) volume change.
Sex difference in mediation by CHD risk factors of risk imparted by adiposity
In examining the association of BMI with the risk of CHD in a meta-analysis of 21 cohorts, the BMI–CHD collaboration investigators concluded that adverse effects of overweight on BP and cholesterol levels could account for about 45% of the increased CHD risk.[21] A residual independent risk by excess weight was emphasized. A similar conclusion was reached by the effects of BMI on CVD in a pooled analysis of 97 prospective cohort studies. BP was the most important factor causing a third of the excess risk on CHD and two-thirds on stroke.[22] Neither of these meta-analyses reported findings stratified for sex.
In males of the TARF study, two-thirds of the risk conferred by WC and one-fifth of effect by WHtR were due to SBP and fasting glucose. HDL-cholesterol affected CHD risk marginally (by 2%–3%). The effects of LDL-cholesterol and physical activity on incident CHD were negligible. In females, only 15% of the risk conferred by WC and 10% by WHtR were mediated by SBP and fasting glucose. HDL-cholesterol affected CHD risk also in females only marginally (by 1%–1.5%). LDL-cholesterol and physical activity affected around 2% for incident CHD. With respect to coronary mortality among TARF participants, the risk was fully mediated by SBP, fasting glucose and total cholesterol among males, in contrast to substantial retention by BMI.[23] The adiposity measure WHtR, found best in older Swedish adults, also showed sex difference in CVD risk mediation, but interestingly in reverse sex, namely, greater risk retention among males.[6]
During a median follow-up of 7.9 years in the DECODE study,[1] 3436 individuals died, two-fifths from CVD. A linear relationship was detected for all five indicators with CVD mortality and for WHR with all-cause mortality, while a J-shaped relationship was detected for WC and WHtR with all-cause mortality in both sexes.
Sex-specific thresholds of WC and WHtR for risk of CHD
A J-shaped association between any adiposity surrogate and CHD risk was not observed in either sex. This differs materially from our experience with regard to risk of all-cause death. In people free of CHD, insofar as WC values for multivariable-adjusted mortality risk were U-shaped, becoming more prominent at a 4-year (rather than 10-year) follow-up (unpublished data). This suggests that a narrow WC confers mainly non-coronary death risk (likely through autoimmune pathways).
Using 0.3 SD for the adiposity measures, we can propose the following thresholds for risk of CHD in males and females: 97 and 94 cm in WC and 0.585 and 0.62 in WHtR, respectively. These WHtR thresholds would correspond to 99 and 97 cm of WC in average Turkish males and females having mean heights of 1.70 and 1.57 cm, respectively. Hence, the initially stated WC thresholds appear to be practical for adoption. Their specificity (63% and 65% in males and females) and sensitivity (52% and 54% in males and females) yielded a high negative predictive value of 86% in each sex, yet a relatively low positive predictive value (23% and 25% in males and females) in such middle-aged individuals.
BMI has been the indicator of adiposity used and recommended by the Turkish Health Ministry for the purpose of health promotion. We believe that this policy is inappropriate and instead WC should be monitored.
Sex-modulated role of hip circumference and height
Contrary associations of waist and HC with CHD have been reported in general.[10] However, HC emerged in this study to impart an age-adjusted risk of CHD in each sex and, in females, even after adjustment for the three mediating risk factors. This is the reason why WHR among Turkish people is distinctly inferior to WC in predictive value. In a comparison between German and Turkish adults, we had previously reported that changes in WC and HC were significantly associated independently with elevated LDL-cholesterol in Germans, but not among Turkish people.[24] Excess of overall obesity in Germans and Turkish women, and abdominal obesity among Turkish males, appeared to be major determinants of SBP. In contradistinction of the high relevance of abdominal obesity in Turkish males, females tend to be burdened by increased CHD risk also through body fat mass,[19],[25] being in line with the tomographic finding that impaired fasting glucose (IFG) was associated only with SAT but not with VAT volume change, beyond generalized or central adiposity.[20] The latter measure exhibited sex interaction in association with both IFG and incident MetS. This disparity in ethnicity and sex reflects pathogenic differences and requires a modified emphasis of preventive and therapeutic measures. However, HC was documented in a study to be a significant predictive risk factor of atrial fibrillation independent of other anthropometric measures except for weight.[26] Thus, the notion of HC being a cardioprotective factor seems to need revision or modification.
As regards height, short stature was a significant risk factor of death (and tended to be so for incident CHD) in Turkish females alone, attenuating only marginally by adjustments for relevant factors.[27] Shorter height presumably reflects enhanced low-grade inflammation already in puberty, the persistence of which may lead preferentially to CHD. Hence, a decrement in the denominator of WHtR would contribute to a higher WHtR.
In the Rotterdam Study, ABSI was documented to modestly predict CVD in males––though not in females––in a non- laboratory-based model.[28] In a study from Iran which was conducted on 9555 patients, the relationship of ABSI with CHD risk factors or metabolic syndrome was reported to be weak.[29] And also, in another study which was conducted on 10 141 patients, ABSI was found to have a lower value in predicting incident CHD.[30] Current unadjusted C-statistics showed ABSI to be an intermediate surrogate in each sex, but strongly attenuated upon adjustment for four conventional risk factors. Based on our results, we have shown that ABSI was not a good predictor on incident CHD. This may be attributed to the inclusion in the equation of a BMI exponent, which is inferior to WC as a residual risk factor in Turkish males. Traditional eating habits or physical characteristics of the Turkish population may have contributed to that finding.
Possible explanation for independent relevance of adiposity surrogates in females
Obesity mediation by conventional risk factors varied across sexes, being prominent in males, compared to contributing little mediation in females. The sex-modulated retained CHD risk by excess adiposity thus may follow pathways of systemic inflammation, endothelial dysfunction and thrombogenic factors––beyond elevated BP, dyslipidaemia or dysglycaemia. The retention of the majority of the obesity risk in females supports the notion of an autoimmune process activated by obesity, being more common in females than males.[31] This finding supports the one reported in the TARF study on residual risk related to the influence of BMI on CHD and coronary mortality.[23] It is recognized that enhanced low-grade inflammation may lead to insulin resistance and diabetes in people with adiposity.[32]
Implications. The most appropriate adiposity measure among Turkish adults to assess future risk of CHD was WC, which should be monitored. WHtR is similarly suited to indicate CHD risk only in males but complicates if a second measure is used.
Limitations and strengths
We avoided potential overadjustment by not adjusting for variables such as serum triglycerides, socioeconomic status or physical activity that could mediate associations between adiposity indicators and CHD risk.[32] As a limitation, we have not evaluated dietary habits in our study. The large number of incident CHD cases, separate analysis in the sexes and head-to-head comparison of five adiposity surrogates constitute the strengths of our study.
Conclusions
WC was the most suitable of the five adiposity indicators for estimating risk for CHD among middle-aged and elderly Turkish adults. Unmediated adiposity risk in males was similarly identified by WHtR. In contrast to the risk mediated by conventional risk factors to a larger extent in males, retention of a large part of the risk in females may be due to other not well known factors.
Acknowledgement
We acknowledge the Turkish Society of Cardiology, Istanbul, Turkey, for supporting the Turkish Adult Risk Factor (TARF) surveys.
Conflicts of interest. None declared
| 1. | Song X, Jousilahti P, Stehouwer CD, Söderberg S, Onat A, Laatikainen T, et al. Comparison of various surrogate obesity indicators as predictors of cardiovascular mortality in four European populations. Eur J Clin Nutr 2013;67:1298–302. [Google Scholar] |
| 2. | Browning LM, Hsieh SD, Ashwell M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0.5 could be a suitable global boundary value. Nutr Res Rev 2010;23:247–69. [Google Scholar] |
| 3. | Cornier MA, Després JP, Davis N, Grossniklaus DA, Klein S, Lamarche B, et al. Assessing adiposity: A scientific statement from the American Heart Association. Circulation 2011;124:1996–2019. [Google Scholar] |
| 4. | Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: Systematic review and meta-analysis. Obes Rev 2012;13:275–86. [Google Scholar] |
| 5. | Page JH, Rexrode KM, Hu F, Albert CM, Chae CU, Manson JE, et al. Waist-height ratio as a predictor of coronary heart disease among women. Epidemiology 2009;20:361–6. [Google Scholar] |
| 6. | Carlsson AC, Risérus U, Engström G, Ärnlöv J, Melander O, Leander K, et al. Novel and established anthropometric measures and the prediction of incident cardiovascular disease: A cohort study. Int J Obes (Lond) 2013;37:1579–85. [Google Scholar] |
| 7. | Emerging Risk Factors Collaboration, Wormser D, Kaptoge S, Di Angelantonio E, Wood AM, Pennells L, et al. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: Collaborative analysis of 58 prospective studies. Lancet 2011;377:1085–95. [Google Scholar] |
| 8. | Hartz A, Grubb B, Wild R, Van Nort JJ, Kuhn E, Freedman D, et al. The association of waist hip ratio and angiographically determined coronary artery disease. Int J Obes 1990;14:657–65. [Google Scholar] |
| 9. | Gruson E, Montaye M, Kee F, Wagner A, Bingham A, Ruidavets JB, et al. Anthropometric assessment of abdominal obesity and coronary heart disease risk in men: The PRIME study. Heart 2010;96:136–40. [Google Scholar] |
| 10. | Canoy D, Boekholdt SM, Wareham N, Luben R, Welch A, Bingham S, et al. Body fat distribution and risk of coronary heart disease in men and women in the European prospective investigation into cancer and nutrition in Norfolk cohort: A population-based prospective study. Circulation 2007;116:2933–43. [Google Scholar] |
| 11. | Onat A, Ceyhan K, Baºar O, Erer B, Toprak S, Sansoy V, et al. Metabolic syndrome: Major impact on coronary risk in a population with low cholesterol levels: A prospective and cross-sectional evaluation. Atherosclerosis 2002;165:285–92. [Google Scholar] |
| 12. | Satman I, Omer B, Tutuncu Y, Kalaca S, Gedik S, Dinccag N, et al. Twelve-year trends in the prevalence and risk factors of diabetes and prediabetes in Turkish adults. Eur J Epidemiol 2013;28:169–80. [Google Scholar] |
| 13. | Onat A, Hergenç G. Low-grade inflammation, and dysfunction of high-density lipoprotein and its apolipoproteins as a major driver of cardiometabolic risk. Metabolism 2011;60:499–512. [Google Scholar] |
| 14. | Onat A, Uyarel H, Hergenç G, Karabulut A, Albayrak S, Can G, et al. Determinants and definition of abdominal obesity as related to risk of diabetes, metabolic syndrome and coronary disease in Turkish men: A prospective cohort study. Atherosclerosis 2007;191:182–90. [Google Scholar] |
| 15. | Onat A, Sari I, Hergenç G, Yazici M, Uyarel H, Can G, et al. Predictors of abdominal obesity and high susceptibility of cardiometabolic risk to its increments among Turkish women: A prospective population-based study. Metabolism 2007;56:348–56. [Google Scholar] |
| 16. | Onat A, Þurdum-Avcý G, Þenocak M, Örnek E, Gözükara Y. Serum lipids and their interrelation in Turkish adults. J Epidemiol Community Health 1992;46:470–6. [Google Scholar] |
| 17. | Rose G, Blackburn H, Gillum RF, Prineas RJ. Cardiovascular Survey Methods. 2nd ed. Geneva, Switzerland:WHO; 1982;124–7. [Google Scholar] |
| 18. | Flint AJ, Rexrode KM, Hu FB, Glynn RJ, Caspard H, Manson JE, et al. Body mass index, waist circumference, and risk of coronary heart disease: A prospective study among men and women. Obes Res Clin Pract 2010;4:e171–81. [Google Scholar] |
| 19. | Onat A, Avci GS, Barlan MM, Uyarel H, Uzunlar B, Sansoy V, et al. Measures of abdominal obesity assessed for visceral adiposity and relation to coronary risk. Int J Obes Relat Metab Disord 2004;28:1018–25. [Google Scholar] |
| 20. | Lee JJ, Pedley A, Hoffmann U, Massaro JM, Fox CS. Association of changes in abdominal fat quantity and quality with incident cardiovascular disease risk factors. J Am Coll Cardiol 2016;68:1509–21. [Google Scholar] |
| 21. | Bogers RP, Bemelmans WJ, Hoogenveen RT, Boshuizen HC, Woodward M, Knekt P, et al. Association of overweight with increased risk of coronary heart disease partly independent of blood pressure and cholesterol levels: A meta-analysis of 21 cohort studies including more than 300 000 persons. Arch Intern Med 2007;167:1720–8. [Google Scholar] |
| 22. | Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration (BMI Mediated Effects), Lu Y, Hajifathalian K, Ezzati M, Woodward M, Rimm EB, et al. Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: A pooled analysis of 97 prospective cohorts with 1.8 million participants. Lancet 2014;383:970–83. [Google Scholar] |
| 23. | Can G, Onat A, Yurtseven E, Karadeniz Y, Akbaº-aimºek T, Kaya A, et al. Gender-modulated risk of coronary heart disease, diabetes and coronary mortality among Turks for three major risk factors, and residual adiposity risk. BMC Endocr Disord 2016;16:54. [Google Scholar] |
| 24. | Can G, Schwandt P, Onat A, Hergenç G, Heiss GM. Body fat measures, dyslipidemia, blood pressure and effects of smoking among German vs. Turkish men and women. Turk J Med Sci 2009;39:579–89. [Google Scholar] |
| 25. | Onat A, Uður M, Can G, Yüksel H, Hergenç G. Visceral adipose tissue and body fat mass: Predictive values for and role of gender in cardiometabolic risk among Turks. Nutrition 2010;26:382–9. [Google Scholar] |
| 26. | Fenger-Grøn M, Overvad K, Tjønneland A, Frost L. Lean body mass is the predominant anthropometric risk factor for atrial fibrillation. J Am Coll Cardiol 2017;69:2488–97. [Google Scholar] |
| 27. | Onat A, Ornek E, Can G, Ciçek G, Murat S. Short stature is an independent risk marker for mortality and incident coronary heart disease only in women: A structural relationship? Anadolu Kardiyol Derg 2012;12:289–97. [Google Scholar] |
| 28. | Dhana K, Ikram MA, Hofman A, Franco OH, Kavousi M. Anthropometric measures in cardiovascular disease prediction: Comparison of laboratory-based versus non-laboratory-based model. Heart 2015;101:377–83. [Google Scholar] |
| 29. | Haghighatdoost F, Sarrafzadegan N, Mohammadifard N, Asgary S, Boshtam M, Azadbakht L, et al. Assessing body shape index as a risk predictor for cardiovascular diseases and metabolic syndrome among Iranian adults. Nutrition 2014;30: 636–44. [Google Scholar] |
| 30. | Sözmen K, Ünal B, Sakarya S, Dinc G, Yardim N, Keskinkilic B, et al. [Association of Anthropometric Measurement Methods with Cardiovascular Disease Risk in Turkey]. Dicle Med J 2016;43:99–106. [Google Scholar] |
| 31. | Onat A, Can G. Enhanced proinflammatory state and autoimmune activation: A breakthrough to understanding chronic diseases. Curr Pharm Des 2014;20: 575–84. [Google Scholar] |
| 32. | Van Gaal LF, Mertens IL, De Block CE. Mechanisms linking obesity with cardiovascular disease. Nature 2006;444:875–80. [Google Scholar] |
Fulltext Views
2,550
PDF downloads
1,286




