Translate this page into:
Patient safety at a public hospital in southern India: A hospital administration perspective using a mixed methods approach
2 Department of Hospital Administration, Nizam’s Institute of Medical Sciences, Hyderabad, Telangana, India
Corresponding Author:
Laxmitej Wundavalli
Department of Hospital Administration, All India Institute of Medical Sciences, Ansari Nagar, New Delhi 110029
India
tej.wundavalli@gmail.com
| How to cite this article: Wundavalli L, Bulkapuram S G, Bhaskar N L, Satyanarayana N. Patient safety at a public hospital in southern India: A hospital administration perspective using a mixed methods approach. Natl Med J India 2018;31:39-43 |
Abstract
Background Patient safety cannot be considered in isolation when organizational factors, both active and latent, influence patient outcomes.Methods We did a cross-sectional mixed methods study using a convergent parallel design at a tertiary care public sector hospital in Hyderabad, Telangana (i) to qualitatively investigate the nature and determinants of patient safety incidents occurring in the hospital; (ii) to quantify the perception of hospital staff regarding factors affecting patient safety from an organizational perspective; and (iii) to triangulate the results to highlight areas in need of improvement.
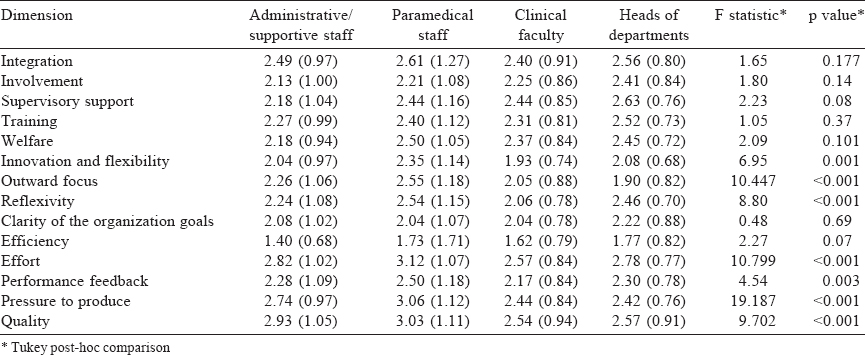
Results The most common factors affecting patient safety were situational factors, working conditions and latent organizational factors including communication systems. Despite the relatively poor knowledge of paramedical staff regarding patient safety incidents, they perceived innovation and flexibility, outward focus, reflexivity, quality, pressure to produce, performance feedback and effort to be significantly higher compared to the heads of departments and clinical faculty. The strength of the dimensions: integration, involvement, training, welfare, supervisory support in the hospital was weak as perceived by all categories of staff.
Conclusion There is a need to build team work, improve trust and communication between various departments, invest more in training, and provide supervisory support along with structural and process improvements in issues such as drug procurement and developing patient-friendly physical environment.
Introduction
The present concepts of patient safety place the prime responsibility for most adverse events on deficiencies in system design, organization and operation rather than on negligence or poor performance of individual providers or products.[1] In order to make healthcare safer, organizational systems must be redesigned to make commission of errors more difficult.[2],[3] The Swiss cheese model[4] is an example of how systems may be designed to prevent adverse events at various levels. An interdisciplinary approach to patient safety begins with an organizational structure committed to cooperation and communication, and one that welcomes and encourages positive change.[5]
The aspect of organizational safety culture that may be visible or measurable is sometimes referred to as the safety ‘climate’, which includes management systems, safety systems, and individual attitudes and perceptions. ‘Safety climate can be regarded as the surface features of the safety culture discerned from the workforce attitudes and perceptions at a given point in time. It is a snapshot of the state of safety providing an indicator of the underlying safety culture of the work group, plan or organization’.[6] However, domain-specific studies such as ‘safety climate’ studies ignore the broader context in which the organizational climate operates. It is likely that organizational characteristics reinforce one another and that the total effect is greater than the sum of the individual dimensions.
For example, communication (failures), an important dimension of organizational climate, has been reported to be responsible for over 60% of the causes of sentinel events reported to the Joint Commission on Accreditation of Healthcare Organizations.[7] Lack of feedback has been found to be a major barrier to reporting for doctors and nurses.[8]
In India, measuring quality and quality improvement initiatives in a majority of hospitals and nearly all public hospitals is still ‘work in progress’. Though the process of accreditation is being actively pursued by the private sector, even these processes miss intangible but important elements such as communication. Often on the pretext of high patient load in public hospitals, nontechnical but critical elements such as communication, team factors, supervisory support and training related to factors affecting patient safety are ignored despite hospitals investing substantially in technical equipment. There is no established database to inform the context of patient safety incidents in public hospitals.
We aimed (i) to qualitatively investigate the nature and determinants of patient safety incidents that occurred in a hospital; (ii) to quantitatively assess the perception of hospital staff regarding various factors affecting patient safety using a standardized instrument (Organizational Climate Measure [OCM]);[9] (iii) to study the differences in perception between core clinical staff and paramedical/support staff; and (iv) to integrate the results to inform both faculty and staff regarding their perceptions within and among themselves to set targets for patient safety.
Methods
Study design
We did a cross-sectional mixed methods study using a convergent parallel design. The qualitative study retrospectively investigated the nature and determinants of patient safety incidents that occurred in the hospital reported by clinical faculty, residents, hospital administrators, paramedical personnel and patients or their attendants. We also did a quantitative study using OCM.[9]
Study setting
The study was done at a tertiary care, public sector, teaching hospital in Hyderabad, Telangana, India. The hospital had 985 beds with an average bed occupancy of 85%. There were 29 outpatient departments, 18 inpatient departments of which 9 were broad specialties, in addition to 8 supportive service departments. The hospital had 10 operation theatres, 9 intensive care units, 23 wards and private rooms, and a well-equipped emergency medicine department. It had a clientele of around 110 organizations and catered to about 250 000 outpatients and about 35 000 inpatients annually. It performed 9000 major operations, 8000 minor operations and about 3000 emergency operations annually.
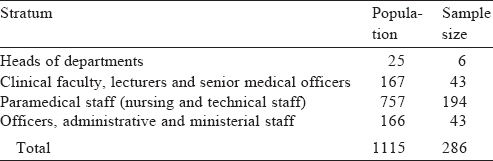
Sample size
We collected patient safety incidents during the 6 months before the study. Events that were directly related to the patient’ s clinical status were excluded. The population for the quantitative aspect comprised 1115 permanent employees who had been working for a minimum of 3 years in the institution. Residents, nursing students, class IV employees and security personnel were excluded from the study. The required sample size was calculated as 286.[10] The margin of error chosen was 5%, confidence level 95% and response distribution was assumed at 50%. Probability stratified sampling technique was used to calculate sample size for each of the four strata [Table - 1].
Tools
The information of patient safety incidents was obtained through rounds of hospital administrators, complaints from staff, complaints from patients, interviews with nursing staff, and reports obtained by hospital administrators. Wherever possible, qualitative interviews were held based on a single question framed using the patient safety incident definition proposed by the National Patient Safety Agency, National Health Service, UK.[11] The participant was asked to describe any unexpected or unintended event(s) that had either caused or could have caused harm to a patient while in the hospital. Prompts were given, if required, to elucidate an incident that someone had been involved in, incidents that someone may have witnessed, incidents that caused no harm or minimal harm, incidents with a more serious outcome, or near misses. A root-cause analysis of each incident was done by qualified hospital administrators and the factor(s) responsible for each incident noted. All factors were classified using the Yorkshire contributory factors framework under either communication systems, individual factors, physical environment, equipment and supplies, design of equipment and supplies, staff workload, support from central functions and supervision and so on [Figure - 1].[12]
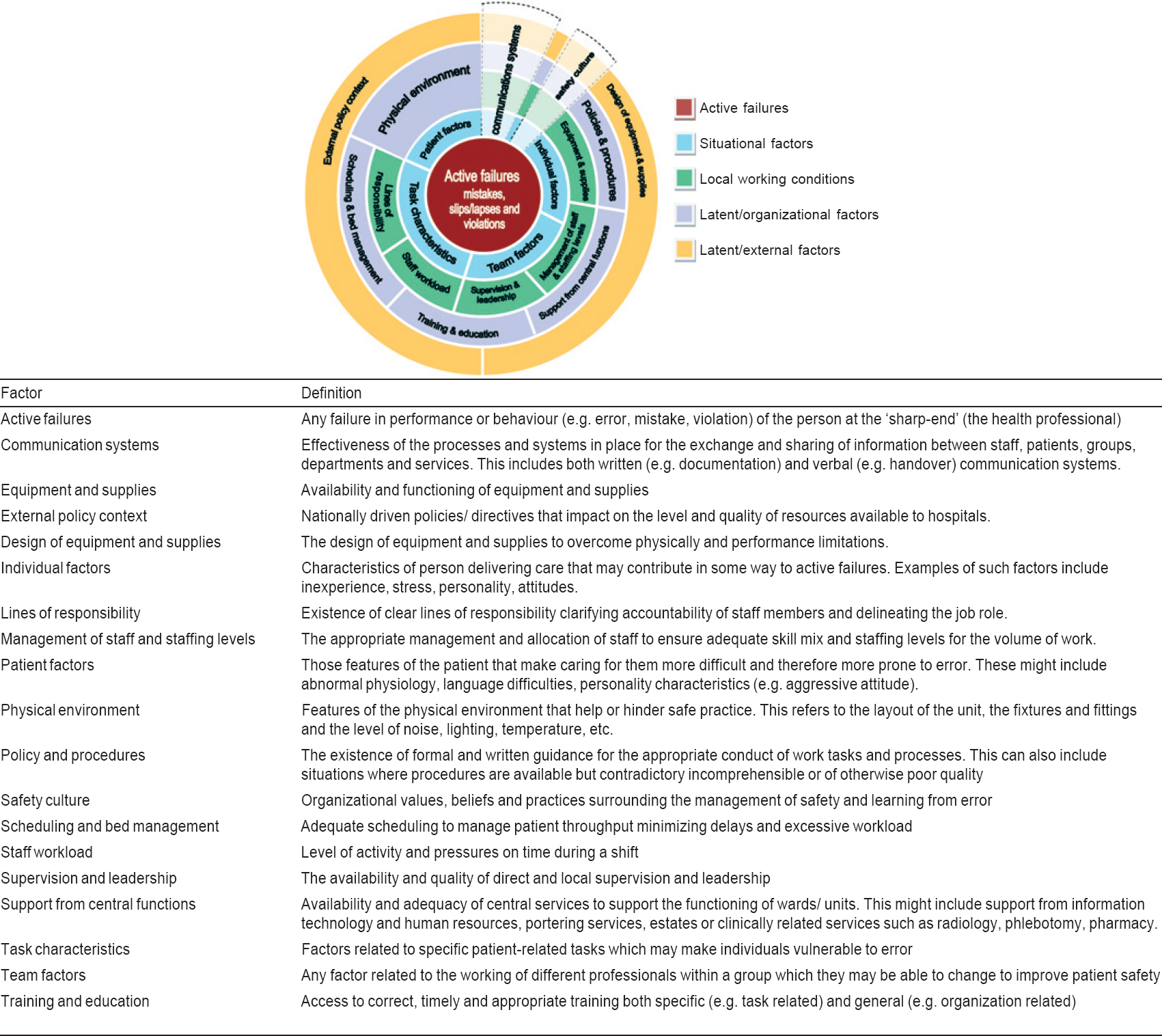 |
| Figure 1: Yorkshire contributory factors framework[12] |
Quantitatively, the perception of staff was captured using OCM, a standardized instrument, developed by Patterson et al.[9] Of the 17 dimensions of the OCM, 14 were selected as they were felt to be directly or indirectly responsible for a potential patient safety event, as were also found from the results of the qualitative component of the study. Quantitative data were analysed using Microsoft Excel for descriptive statistics.
A one-way ANOVA was used to test for differences in perception with respect to each dimension among the four categories of staff. Tukey post-hoc analyses were done if statistically significant differences (p<0.05) were found in perceptions among the staff.
Ethical approval was obtained from the Institutional Ethics Committee before the start of the study and informed consent obtained from the participants.
Results
Qualitative study
Forty patient safety incidents were documented which included near misses, adverse events and sentinel events. Medication administration errors were the commonest (30%, n=12), followed by non-availability of medicines (25%, n=10) and falls (7.5%, n=3). Other miscellaneous events (32.5%, n=11) included improper documentation of patient identity and transportation of patient’s blood sample leading to repeat phlebotomies and lack of beds especially in neurosurgery and urology, which led to patients being sent to other areas such as the emergency, medical superintendent’s office or the hospital administrator without briefing the patient/attendant. The hospital administrator reported patient complaints occurring solely due to lack of communication between departments. Non-availability of biomedical waste yellow bags led to a mandatory critical incident reporting which was due to delay in both external and internal lead times in procurement of yellow bags.
Of the total events, 5% (n=2) were sentinel events (those that led to death of a patient but were not due to core clinical reasons), of which one was due to the physical environment and the other due to an individual factor.
Medication administration errors were mostly due to individual factors (experience) and communication systems (hand-offs, documentation in case sheet or labelling) as per the Yorkshire contributory factors framework. In three incidents, interruptions led to lack of documentation in the case sheet. This led to clinical errors in the form of a missed dose and wrong doses. The sources of interruption were phone and the physician who called the nurse for some instructions. However, no adverse events occurred due to this. Five (40%) of the medical administration errors could also be traced to inadequate training and supervisory support.
Non-availability of medicines was usually due to supply issues (out of stock, medicine not being under rate contract list, procurement held up due to issues such as transport licence or the drug due to being a non-moving category item was not available).
Communication systems contribution to these incidents
The third most common cause was falls, which were due to equipment and supplies (absence of hand rails in toilet and faulty bedrails). Two adverse events were reported due to falls and both occurred in elderly patients.
As per the Yorkshire contributory factors framework, the factors found to affect patient safety were due to (i) communication systems; (ii) individual factors; (iii) physical environment; (iv) equipment and supplies; (v) design of equipment and supplies; (vi) staff workload; and (vii) support from central functions and supervision. In addition, we observed the following:
- The nursing staff, especially, were not able to describe any patient safety incident spontaneously. All of them sought more information as to what would constitute a patient safety event.
- All events were reported only after anonymity was assured except for the complaints.
- None of the respondents reported events from their own professional category voluntarily. For example, an event was reported by a doctor when the line of responsibility would either be on a nurse, technician or an administrative staff and vice versa.
- No near misses were reported spontaneously.
Quantitative component of the study
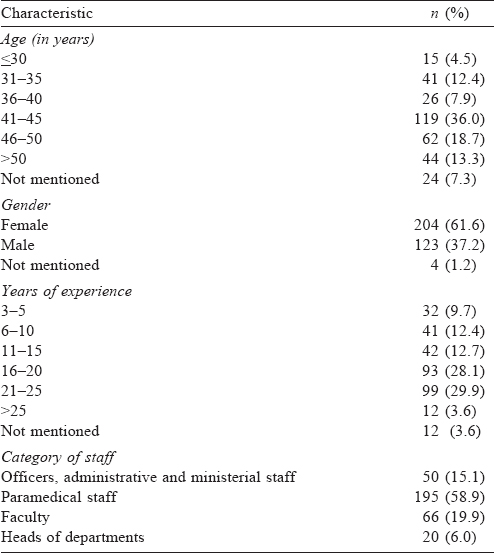
Of the 450 questionnaires that were distributed, we received completed ones from 331 employees. There were no significant differences in perception of the various dimensions or factors when job designation, years of experience or age of the respondents were considered [Table - 2] and [Table - 3].
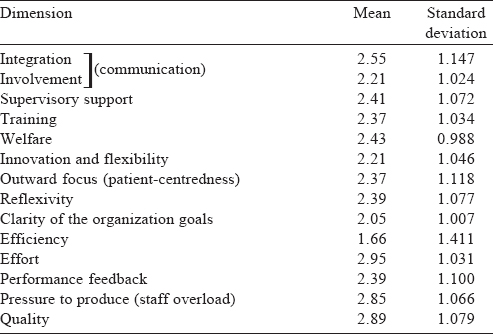
Tukey post-hoc analyses showed that paramedical staff generally had a better perception of the dimensions that were significantly different between the four categories of staff [Table - 4].
Discussion
The qualitative aspect of our study highlights that communication systems contributed to most incidents directly or indirectly. This is an already recognized threat to patient safety.[14],[15],[16],[17] The knowledge of staff regarding patient safety incidents was poor and an unexpressed ‘blame culture’ was observed; both are recognized road blocks in improving patient safety.[18]
There was no critical incident reporting system at the institute level. Some departments evaluated patient safety incidents within their respective units as a closed group, thereby losing the opportunity to disseminate important information. This could be due to fears of blame, punishment, litigation and being habituated to working in silos. Further, these departmental incidents are core clinical events rather than events that could have occurred due to organizational factors.
The maximum and minimum scores possible are 4 and 1, respectively, for each question of the quantitative tool. If the overall score veers towards 4 or 1, it indicates agreement among all respondents and means that the dimension is strong in that particular direction. For example, if the mean scores are towards 4, it indicates strength in a positive sense of perception and if the score is towards 1, it also indicates strength, but in a negative sense of perception. If the scores hover in between, it indicates poor agreement among the respondents and means that the strength is weak. Both higher strength in a negative sense of perception or weak strength reflect the need for intervention and improvement in that particular dimension.
The weak strength of critical dimensions such as involvement and integration is of concern as many patients require consultations from more than one department owing to multiple comorbid conditions. Also, all respondents were permanent employees with at least 3 years of experience in the hospital. This underscores the need to disseminate the hospital’s policies, procedures and goals among all the staff even more rigorously. Even if communication processes were good in a particular unit or department, the same was lost if it involved other departments at the holistic level affecting patient’s experience. Often, issues had to be resolved by individuals rather than by existing systems in the hospital. Studies note that teams that described the communication processes in clear terms were more efficient in completing critical tasks than teams that were ambiguous in their communication.[19] Also, asymmetrical power relations in interdisciplinary teams have been found to influence the interaction and inhibit safety.[16]
The paramedical staff scored higher on outward focus, quality and reflexivity. However, the qualitative component of our study revealed that knowledge of the paramedical staff was poor with respect to patient safety events. The higher perception should be a cause for concern as it fosters false complacence when, in reality, greater and corrective efforts might be needed.
There is a need to educate and train staff and students regarding recognition and reporting of patient safety incidents. Recent studies have highlighted the importance and success of patient safety education programmes to bring about major changes in knowledge, skills and behaviour along with quality improvements.[20] However, it has also been emphasized that training should lead to demonstrable patient benefit, which is again both difficult to implement and measure, and requires further research.[21] In this regard, the absence of a common incident reporting system was identified as an important barrier to acting proactively and evolving as a learning organization. To start with, efforts should start in a top-down approach and underscore the need for blame-free reflection and analysis of events.
The qualitative study identified communication systems as the common factor in all reported events. The quantitative aspect revealed that strength of communication critical dimensions such as integration and involvement was weak. The nature of relationships between and among different departments was found to be particularly poor. Ineffective communication has been identified as a major cause of critical incidents even in public hospitals in Australia.[22] Communication and team work have been recognized to influence patient safety.[23] Guidance should be taken from studies that have mentioned in detail strategies that may be used in this regard.[24]
The climate of the organization was also weak with respect to supervisory support and training, both have been recognized as factors affecting patient safety. There is a need to replace the fragmented approach with teamwork along with inclusion of patients in their care.
The ratings of the dimension ‘pressure to produce’ in nursing staff was higher reflecting the need to study the level of stress among nursing staff and take appropriate warranted steps.
Despite the risk of bias, the respondents scored high on the dimension effort which gives an optimistic outlook, reflecting employees’ willingness to work hard to achieve goals and should be harnessed to orient staff towards the goals and mission of the hospital.
Overall, our study identifies situational factors, working conditions and latent organizational failures that are preventable and should be addressed by hospital administrators. There is a need to take reformative steps to address the issues of trust, team work and engagement between different departments at all levels of employees.
The limitations of our study are that our list of patient safety incidents was not exhaustive and that we excluded residents from the quantitative study. The reason for exclusion was that being a floating population with varying months of experience in the institution, they may confound the results as most of them get exposed to the hospital’s policies and procedures gradually.
Conclusion
We found that there is a low awareness among health workers of patient safety incidents and there is no robust mechanism for reporting such incidents. The ‘blame culture’ may be responsible for this. There is a need to institute a patient safety reporting incident system with training of all categories of staff in patient safety and quality improvements in a collaborative and sustainable manner.
Acknowledgement
We are grateful to Mr Jeremy Dawson, Senior Lecturer in Health Management, Institute of Work Psychology/School of Health and Related Research, University of Sheffield, UK, for giving permission to use the Organisational Climate Measure (OCM).
Conflicts of interest: None declared
| 1. | Promoting patient safety at health care institutions. Report and documentation of the technical discussions held in conjunction with the 43rd Meeting of CCPDM WHO/ SEARO, New Delhi, 14-16 June 2006. Available at www.searo.who.int/LinkFiles/Quality_and_safety_in_health_care_HS-22 7-Promoting_Patient_Safety_at_Health_Care.pdf (accessed on 15 Sep 2015). [Google Scholar] |
| 2. | Beurhaus PI. Follow-up conversation with Lucian Leape on errors and adverse events in health care. Nurs Outlook 2001;49:73-7. [Google Scholar] |
| 3. | Berwick DM. Taking action to improve safety: How to increase the odds of success. In: American Association for the Advancement of Science, Annenberg Center for the Health Sciences, National Patient Safety Foundation. Proceedings of enhancing patient safety and reducing errors in health care: 8–10November 1998. Chicago, Illinois:National Patient Safety Foundation; 1999. [Google Scholar] |
| 4. | Reason J. Human error. New York:Cambridge University Press; 1990. [Google Scholar] |
| 5. | Classen DC, Kilbridge PM. The roles and responsibility of physicians to improve patient safety within health care delivery systems. Acad Med 2002;77:963-72. [Google Scholar] |
| 6. | Flin R, Mearns K, O’Connor P, Bryden R. Measuring safety climate: Identifying common features. Saf Sci 2000;34:177-92. [Google Scholar] |
| 7. | Joint Commission on Accreditation of Healthcare Organizations. Sentinel event statistics. Available at www.jcaho.org/accredited+organizations/sentinel+event/sentinel+event+statistics.htm (accessed on 11 Sep 2015). [Google Scholar] |
| 8. | Benn J, Koutantji M, Wallace L, Spurgeon P, Rejman M, Healey A, et al. Feedback from incident reporting: Information and action to improve patient safety. Qual Saf Health Care 2009;18:11-21. [Google Scholar] |
| 9. | Patterson MG, West MA, Shackleton VJ, Dawson JF, Lawthom R, Maitlis S, et al. Validating the organizational climate measure: Links to managerial practices, productivity and innovation. J Organiz Behav 2005;26:379-408. [Google Scholar] |
| 10. | Sample size calculator. Available at www.raosoft.com/samplesize.html(accessed on 10 Mar 2013). [Google Scholar] |
| 11. | What is a patient safety incident? National Patient Safety Agency. Available at www.npsa.nhs.uk/nrls/reporting/what-is-a-patient-safety-incident/ (accessed on 10 Mar 2013). [Google Scholar] |
| 12. | Lawton R, McEachan RR, Giles SJ, Sirriyeh R, Watt IS, Wright J. Development of an evidence-based framework of factors contributing to patient safety incidents in hospital settings: A systematic review. BMJ Qual Saf 2012;21:369-80. [Google Scholar] |
| 13. | Westbrook JI, Woods A, Rob MI, Dunsmuir WT, Day RO. Association of interruptions with an increased risk and severity of medication administration errors. Arch Intern Med 2010;170:683-90. [Google Scholar] |
| 14. | Wilson RM, Runciman WB, Gibberd RW, Harrison BT, Newby L, Hamilton JD. The quality in Australian health care study. Med J Aust 1995;163:458-71. [Google Scholar] |
| 15. | Lingard L, Espin S, Whyte S, Regehr G, Baker GR, Reznick R, et al. Communication failures in the operating room: An observational classification of recurrent types and effects. Qual Saf Health Care 2004;13:330-4. [Google Scholar] |
| 16. | Sutcliffe KM, Lewton E, Rosenthal MM. Communication failures: An insidious contributor to medical mishaps. Acad Med 2004;79:186-94. [Google Scholar] |
| 17. | Department of Health. An organisation with a memory. Report of an Expert Group on Learning from Adverse Events in the NHS. London:Her Majesty’s Stationery Office; 2000. [Google Scholar] |
| 18. | Hoffman JR, Kanzaria HK. Intolerance of error and culture of blame drive medical excess. BMJ 2014;349:g5702. [Google Scholar] |
| 19. | Siassakos D, Bristowe K, Draycott TJ, Angouri J, Hambly H, Winter C, et al. Clinical efficiency in a simulated emergency and relationship to team behaviours: A multisite cross-sectional study. BJOG 2011;118:596-607. [Google Scholar] |
| 20. | Ahmed M, Arora S, Tiew S, Hayden J, Sevdalis N, Vincent C, et al. Building a safer foundation: The lessons learnt patient safety training programme. BMJ Qual Saf 2014;23:78-86. [Google Scholar] |
| 21. | Kirkman MA, Sevdalis N, Arora S, Baker P, Vincent C, Ahmed M. The outcomes of recent patient safety education interventions for trainee physicians and medical students: A systematic review. BMJ Open 2015;5:e007705. [Google Scholar] |
| 22. | Scheeres H, Slade D, Manidis M, Mcgregor J, Matthiessen C. Communicating in hospital emergency departments. Sydney:University of Technology and Macquarie University; 2008. Available at www.ameprc.mq.edu.au/docs/prospect_journal/volume_23_no_2/Communicating.pdf (accessed on 11 Mar 2014). [Google Scholar] |
| 23. | Dedy NJ, Bonrath EM, Zevin B, Grantcharov TP. Teaching nontechnical skills in surgical residency: A systematic review of current approaches and outcomes. Surgery 2013;154:1000-8. [Google Scholar] |
| 24. | Dingley C, Daugherty K, Derieg MK, Persing R. Improving patient safety through provider communication strategy enhancements. In: Henriksen K, Battles JB, Keyes MA, Grady ML (eds). Advances in patient safety: New directions and alternative approaches. Vol. 3: Performance and tools. Rockville, MD:Agency for Healthcare Research and Quality (US); 2008. Available at www.ncbi.nlm.nih.gov/books/NBK43663/ (accessed on 15 Sep 2015). [Google Scholar] |
Fulltext Views
3,082
PDF downloads
10,303




