Translate this page into:
Paul McMaster (4 January 1943–27 May 2024)
[To cite: Nundy S. Paul McMaster (Obituary). Natl Med J India 2024;37:162. DOI: 10.25259/NMJI_706_2024]
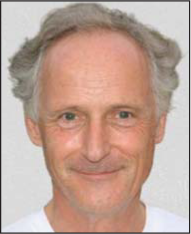
If ever there was a hero in medicine that I knew fairly well, it was Paul McMaster. Not only was he a pioneer and excelled in the surgery of liver transplantation, in 2003 he retired from the National Health Service (NHS) in the UK and spent the rest of his life working in many developing countries—Somalia, the Congo and Burundi—especially in places where there was conflict such as Syria, Sri Lanka, Afghanistan, and in Haiti during the 2010 earthquake.
Paul was born in Liverpool where his father was a general practitioner. He studied medicine and became a registrar in the Department of Surgery at Addenbrooke’s Hospital in Cambridge under the redoubtable Professor Sir Roy Calne. I was his immediate predecessor and he always blamed me for leaving a pile of patients’ discharge summaries for him to complete and also because the ward nurses used to say ‘where is that nice Indian doctor. We want him back’.
He was appointed to the faculty in Cambridge and then moved to Birmingham where he set up the second liver transplant centre in the UK with my Guy’s Hospital student colleague, the hepatologist Elwyn Elias. It became one of the largest liver transplantation programmes in Europe and has done more than 6000 transplants to date and trained more than 1000 national and international fellows, including some from India who are now household names in the field. But about that later. He did pioneering research into low-dose immunosuppression and eventually became President of the European Society of Organ Transplantation.
After leaving the NHS, he did a BA in conflict studies and then went to Rwanda and Uganda where he treated women with vesicovaginal fistulae. He then joined the wonderful organization called Medecins Sans Frontieres (MSF) (Doctors Without Borders). MSF was founded in 1971, in the aftermath of the Biafran famine of the Nigerian Civil War, by a small group of French doctors to provide medical care across national boundaries and irrespective of race, religion, creed or political affiliation. It received the Nobel Peace Prize in 1999. Paul worked in the organization and became its Surgical Director in 2012 in Amsterdam and later the UK MSF President. His field work included delivering up to 80 babies in a day, pulling out teeth and performing a below knee amputation on a conscious young girl under local anaesthesia whose leg had become gangrenous after a war injury.
When the Gastrointestinal (GI) Surgery Unit in the All India Institute of Medical Sciences (AIIMS), New Delhi was started in 1985, Peush Sahni, Girish Pande and I thought our work should include liver transplantation and so I was sent by the authorities to Cambridge and Birmingham, the leading centres in the UK, to learn about how this should be done. Both Sir Roy Calne and Paul were gracious hosts and advised us on how to go about changing the law to recognize heart-beating brain death and to stop the trading in human organs, which was rife and almost ‘legal’ in India. Paul discouraged dubious seemingly ‘related’ kidney donation procedures in Birmingham and called them as the ‘Bombay operations’! He also said that there were very few from the large numbers of Asian immigrants in Birmingham who agreed to deceased organ donation. I countered by saying that they did not want to donate as they felt that they were less likely to get an organ as compared to the rest of society. But his assessment remains true even to this date as deceased organ donation has not really taken off in India even 30 years after the passage of the Transplantation of Human Organs Act.
To start the procedure in India I helped organize that Subash Gupta and Arvinder Soin, who were AIIMS graduates and GI Surgery residents, go to Birmingham to work with Paul and after they returned they established successful liver transplantation programmes (from living donors) in Sir Ganga Ram Hospital and later in the Max and Medanta hospitals. They have now become household names in the field and internationally renowned for their work. India now has 184 liver transplant centres and in 2022 performed 3500 procedures, the third highest number in the world after the USA and China.
So we have much to be grateful for to Paul McMaster for helping start liver transplantation in India but I, personally, admire him more for his great altruism in how he gave up a comfortable life in England to travel the world to help victims of poverty and conflict in poor countries to regain their lives.
I cannot think of anyone whose life I admire more. May his soul rest in peace.




