Translate this page into:
Perception of medical interns towards the skills they acquired
2 Department of Pharmacology and University Department of Medical Education, Sri Devaraj Urs Medical College, Sri Devaraj Urs Academy of Higher Education and Research, Kolar, Karnataka, India
Corresponding Author:
Sarala Narayana
Department of Pharmacology and University Department of Medical Education, Sri Devaraj Urs Medical College, Sri Devaraj Urs Academy of Higher Education and Research, Kolar, Karnataka
India
n_sarala@rediffmail.com
| How to cite this article: Lella M, Narayana S, Chinnaiyan S. Perception of medical interns towards the skills they acquired. Natl Med J India 2020;33:236-238 |
Abstract
Background. The undergraduate medical course in India is for five-and-a-half years. Every medical student has to undergo compulsory rotating residential internship for 12 months. During this period, interns acquire skills under supervision. The literature shows they have limited experience and confidence in performing basic and emergency procedures. We assessed interns’ perception of their experience and competence.Methods. We did a questionnaire-based cross-sectional study among medical students after they had completed their internship to reflect on their experience and competence in various procedural skills. A questionnaire (25 questions) based on knowledge and skills was piloted by 15 interns and was reliable (Cronbach alpha 0.9). The Likert scale ranged from never observed to performed independently under supervision.
Results. Seventy-eight of 80 interns responded; 51 were females (65.3%). Three-quarters of interns felt they could independently carry out venous blood sample collection, arterial blood gas interpretation, Pap smear specimen collection and digital rectal examination, but only half felt that they could do a lumbar puncture, cervical dilatation and collection of throat swab. Parenteral drug administration, catheterization, nasogastric tube insertion and cardiopulmonary resuscitation were done confidently by over 90%, but vaginal delivery and application of a plaster slab required assistance. The majority said that they had observed drainage of abscess, excision of sebaceous cyst and endotracheal tube intubation.
Conclusion. Most interns felt that they were competent in performing simple surgical tasks independently. However, conducting a vaginal delivery and endotracheal tube intubation were tasks that needed more support.
Introduction
The undergraduate medical course in India has three phases— preclinical (12 months), paraclinical (18 months) and clinical (24 months) with internship for 1 year.[1] The Medical Council of India (MCI) guidelines recommend 1 year of internship in various departments such as community medicine, surgery, orthopaedics, medicine, obstetrics and gynaecology (OBG), paediatrics, otorhinolaryngology (ENT), ophthalmology and casualty. Every medical student after passing the final Bachelor of Medicine and Bachelor of Surgery (MBBS) examination has to undergo compulsory rotating residential internship for a period of 12 months so as to be eligible for the award of the MBBS degree. The MCI describes internship as ‘a phase of training wherein a graduate is expected to conduct the actual practice of medical and healthcare and acquire skills under supervision so that he/she may become capable of functioning independently’.[2]
It has been shown that medical graduates have limited experience and confidence in performing basic and emergency procedures at the end of the internship.[3],[4] Some residents begin postgraduate training without sufficient experience in procedural skills. We did this study among medical interns to find out the skills they acquired during their internship by asking them to reflect on their experience and competence.
Methods
We did a questionnaire-based cross-sectional study from February to March 2015. The protocol was approved by the Institutional Ethics Committee, and all medical interns who were willing to participate in the study were included after obtaining written informed consent.
A questionnaire consisting of 25 items was prepared based on the knowledge and skills listed in the intern’s log book. The questionnaire was pretested by conducting a pilot study with 15 interns and the internal consistency was found to be reliable (Cronbach alpha 0.9). After 1 year of internship, the interns were asked to give their opinion in terms of their experience and competence in various procedural skills such as emergency, diagnostic and therapeutic procedures.
The Likert scale was used to assess the level of competence, and it was scored as never observed, observed but not performed, performed with assistance and performed independently but under strict supervision of the consultant. Data were analysed using descriptive statistics.
Results
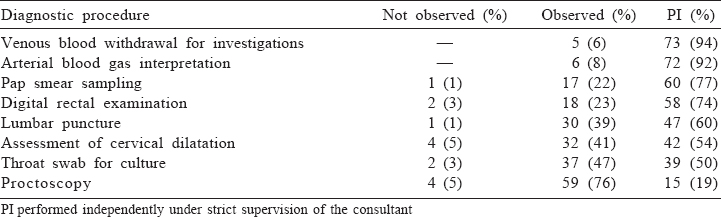
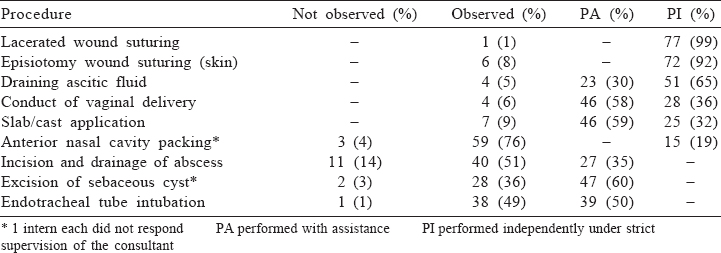
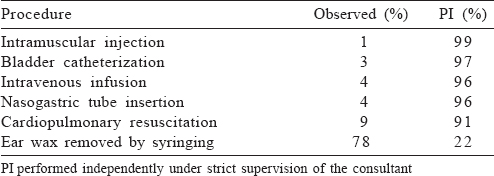
The questionnaire was distributed to 80 interns; 78 filled questionnaires were received (response rate 97.5%). There were 27 males (34.7%) and 51 females (65.3%). The diagnostic procedures performed independently by over 50% of the interns were drawing venous blood, arterial blood gas interpretation, taking a sample for Pap smear, digital rectal examination, lumbar puncture and assessment of cervical dilatation [Table - 1] to [Table - 3].
Discussion
This study aimed to assess competence in procedural skills among medical interns at the end of their internship training. More than 75% of interns perceived that they could carry out diagnostic procedures such as venous blood sample collection, arterial blood gas interpretation, Pap smear specimen collection and digital rectal examination independently but under strict supervision, whereas lumbar puncture, assessment of cervical dilatation and collection of throat swab were accomplished only by 50% [Table - 1].
For the basic therapeutic interventions such as parenteral administration of drugs, catheterization, nasogastric tube insertion and cardiopulmonary resuscitation (CPR), a major procedure, which a basic doctor at the primary health centre should be able to carry out, 90% of our interns expressed that they were confident in performing independently under strict supervision of the consultant [Table - 3], but for some of the procedures (conduct of vaginal delivery and slab/cast application), they required assistance [Table - 2]. This could be first because our students, when in 7th term, have hands-on training in Basic Life Support, and before joining internship, they have hands-on training in both Basic Life Support and Advance Life Support in the skills laboratory. Second, interns get more number of chances to perform CPR because they encounter the situation frequently when posted in medicine, surgery, obstetrics and gynaecology, casualty and anaesthesia. However, chances for proctoscopy and slab application are only when posted in surgery and orthopaedics, respectively, and so fewer encounters could be another reason. ENT procedures such as packing of anterior nasal cavity and removal of ear wax through syringing were observed by nearly 75% of interns [Table - 2] and [Table - 3].
Palappallil has shown that 70%–100% of trained interns were confident of urethral catheterization, femoral vein puncture, Ryles tube insertion, 61% in conduct of normal labour and 51% in intravenous (i.v.) cannulation; they were somewhat confident or undecided about the rest of the skills.[5] In another study, when interns were asked to express to whether internship training had helped them to master clinical skills such as i.v. injection and catheterization, 8.4% of interns strongly agreed, 25% agreed, 41.6% were neutral and 25% disagreed.[6]
A majority of interns expressed that surgical skills such as incision and drainage of abscess, excision of sebaceous cyst and endotracheal tube intubation were observed or performed with assistance from their consultants. In a study, interns were assessed, by direct observation, in the skill of endotracheal tube intubation on mannequin and it was reported that 22% of interns completed all steps correctly in the first attempt, 62% in the second attempt, whereas 16% required a third attempt to correctly complete all the steps. The authors concluded that training for endotracheal tube intubation should be carried out at the beginning of internship before they go for clinical practice and repeated during their rotation, so they can retain their competency and can perform whenever required.[7]
More than 80% of interns perceived that emergency procedures could be handled independently under strict supervision whereas for surgical and obstetric skills only 65% were confident. A study reported that 8.4% of interns strongly agreed with and 91.4% disagreed that they could handle medical emergencies effectively.[6] Another study among final year medical students has shown that they lack confidence in procedures, particularly related to surgical interventions.[8]
A study evaluated the proficiency of 70 interns in using pressurized metered dose inhaler (pMDI), pMDI with a spacer, rotahaler, turbuhaler, and nebulizer and observed that their proficiency in using different inhaler devices was poor. It is essential to provide adequate training to medical graduates in the usage of inhaler devices so that there is proper management of patients with asthma and chronic obstructive pulmonary disease.[9] This is one of the important skills to be learnt and performed by our interns because, in the present scenario, many patients use nebulizers at home.
Limitations
Our study documented the self-assessed experience and competence of interns and they were not evaluated while performing any procedure, which could have given a better assessment of their skills. The opinion of their consultants or unit chiefs may also give us a better picture of their ability to perform various skills. Bandura advocates the principle of self-efficacy, which is an individual’s judgement of his or her capabilities to perform a particular skill successfully.[10]
Conclusion
In this study most interns expressed that they were competent in performing basic surgical skills independently under supervision; however, more attention needs to be given to skills such as conduct of vaginal delivery, abscess drainage and endotracheal tube intubation as these are skills necessary for managing a patient when they work in rural healthcare centres.
Conflicts of interest. None declared
| 1. | Giri PA, Parhar GS. Internship: A transition from a medical student to a doctor. Int J Biomed Adv Res 2012;3:753–5. [Google Scholar] |
| 2. | Medical Council of India. Salient features of regulations on graduate medical education. New Delhi:MCI; 1997. Available from: http://www.mciindia.org/ Rules-and- Regulation/GME_REGULATIONS (accessed on 14 Mar 2019). [Google Scholar] |
| 3. | House AK, House J. Improving basic surgical skills for final year medical students: The value of a rural weekend. Aust N Z J Surg 2000;70:344–7. [Google Scholar] |
| 4. | Kelly MH, Campbell LM, Murray TS. Clinical skills assessment. Br J Gen Pract 1999;49:447–50. [Google Scholar] |
| 5. | Palappallil DS. Self-reported training assessment of medical interns and fresh graduates of a tertiary care centre. Int J Sci Rep 2015;1:127–33. [Google Scholar] |
| 6. | Goyal RC, Khapre MP, Mathur MV, Mudey AB, Tankhiwale SR. Medical internship training programme in a medical college—Voice of internees: Mixed model research. South East Asian J Med Educ 2015;9:28–32. [Google Scholar] |
| 7. | Makwana HD, Suthar NN, Gajjar MP, Thakor AV. Developing competency in interns for endotracheal intubation: An educational article. Int J Appl Basic Med Res 2016;6:201–4. [Google Scholar] |
| 8. | Gazibara T, Nurkovic S, Maric G, Kurtagic I, Kovacevic N, Kisic-Tepavcevic D, et al. Ready to work or not quite? Self-perception of practical skills among medical students from Serbia ahead of graduation. Croat Med J 2015;56:375–82. [Google Scholar] |
| 9. | Kshatriya RM, Khara NV, Paliwal RP, Patel SN. Evaluation of proficiency in using different inhaler devices among intern doctors. J Family Med Prim Care 2016;5:362–6. [Google Scholar] |
| 10. | Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol Rev 1977;84:191–215. [Google Scholar] |
Fulltext Views
3,471
PDF downloads
1,716




