Translate this page into:
Preparing medical students with congenital colour vision deficiency for safe practice
Corresponding Author:
Upreet Dhaliwal
Department of Ophthalmology, University College of Medical Sciences and Guru Teg Bahadur Hospital, Dilshad Garden, Delhi 110095
India
upreetdhaliwal@yahoo.com
| How to cite this article: Dhingra R, Rohatgi J, Dhaliwal U. Preparing medical students with congenital colour vision deficiency for safe practice. Natl Med J India 2017;30:30-35 |
Abstract
Background. Colour vision of candidates is tested in many medical colleges in India at the time of admission to undergraduate courses; however, there are no guidelines, and therefore no counselling, on how students with congenital colour vision deficiency (CCVD) should negotiate the medical course, and how best they can practise safely after graduation. Problems in interpreting coloured signs may lead to misdiagnosis. This study aimed to explore difficulties during clinical work that requires colour discrimination, and to offer suggestions on safe practice based on the findings and a review of the literature.
Methods. We did a cross-sectional study after obtaining institutional ethical clearance and written informed consent. Thirty volunteer medical students with CCVD (≥3 errors on Ishihara chart) were matched with 30 volunteers from their own batch who made no errors. All participants interpreted colour-dependent clinical and laboratory photographs.
Results. Students with CCVD made more errors (range 5–26; mean [SD] 13.17 [5.873] out of 75 items in 35 colour-dependent photographs) than colour-normal students (range 2–13; mean [SD] 5.53 [3.037], p<0.001). The nature of the errors suggested that medical students with CCVD could have problems in learning histology, pathology, haematology, microbiology, dermatology, paediatrics, medicine, biochemistry and during ophthalmoscopy.
Conclusions. Screening at the time of admission will make students aware of their CCVD status and, through conscious practice thereafter, they may understand their limitations. Faculty could guide and prepare such students for safe practice.
Introduction
Colour discrimination is important in medicine, particularly in biochemistry, microbiology and pathology, and for detection of clinical signs.[1],[2],[3],[4] Medical students with congenital colour vision deficiency (CCVD) may have difficulties leading to mis-diagnosis.[1],[5] Currently, though new entrants to the medical courses in India are screened for colour vision deficiency, no further action is taken to guide those who have the deficiency. We believe this is unethical—to label them but offer no counselling. There are no data on problems during practice in India, nor are there safe practice guidelines for doctors with CCVD. We examined difficulties faced by medical students during laboratory and clinical work that depended on colour discrimination. Based on the findings and taking help of the literature, we offer suggestions on how such students can ensure safe practice.
Methods
This cross-sectional, observational study was done from December 2011 to March 2013. Images representing clinical presentations where colour is an important aid to diagnosis were collected from the internet (non-profit, educational purpose; Creative Commons license). Five colour-normal volunteer medical students, and three colour-normal faculty from ophthalmology and pathology (those not involved in the study) pilot-tested the images and helped exclude unclear or ambiguous images. We started with 53 and eventually included 36 images.
At the start of the study, a total of 650 (578 men) medical students were studying at our institution. Of the 322 postgraduate students, 189 were men. The reported prevalence of CCVD is 6%–8% among men owing to their X-linked recessive inheritance, and only 0.4% among women. Using a prevalence of 7% among men, we expected to detect 53 colour vision deficient individuals. Assuming a consent rate of 40%–50%, we set a sample size of 30. In case we did not find the requisite number of students with CCVD, we planned to extend the study to the new batch of students in the following year.
After obtaining clearance from the institutional review board and written informed consent from the study subjects, undergraduate and postgraduate medical students were screened with the 38-plate edition Ishihara chart. The test was done in a separate room where non-participants were not allowed. For the purpose of screening, students were contacted at least three times in the lecture hall after their lectures or in the wards; those who were not available after three attempts were called telephonically for screening. Those who still could not be contacted were considered not to have volunteered and were not screened.
As per standard protocol, students who made three or more errors were considered colour vision deficient; they were invited to volunteer for the study. To control for degree of exposure to, and degree of experience with, laboratory and clinical work, an equal number of undergraduate students from the same batch and postgraduate students from the same postgraduate department and same batch, who made no errors on Ishihara testing, were invited to volunteer as controls. Students with CCVD underwent torch light and ophthalmoscopic examination to exclude ocular conditions known to cause acquired colour vision deficiency (chorio-retinal or optic nerve disease in any eye). The names, identities and clinical data of students with CCVD were kept confidential.
Students with CCVD as well as controls were asked to independently (albeit in the presence of one of the authors) interpret the colour-dependent clinical and laboratory photographs and respond in writing to 1–4 questions for each image; where required, an image showing the normal was provided as an inset. The questions were: indicate if the photograph is within normal limits (yes, no, don't know); describe, in terms of colour, any abnormality that you see; identify and outline areas of abnormality on a transparent overlay; and record your self-reported degree of confidence in your response (very confident to low confidence). In all, 35 photographs generated 75 items requiring their response. Each error they made was given a count of one and total errors were recorded. In addition, they had to count the number of acid-fast bacilli (AFB) in a fixed area on a slide stained with Ziehl–Neelsen stain.
When the proportion of students with CCVD and those who were colour normal who made the error was the same, and the confidence also comparable for both groups, the error was considered not to be related to CCVD. However, when considerably more students with CCVD made errors than controls from the same batch, we assumed that the errors were related to the CCVD.
SPSS version 17 was used for statistical analysis. Chi-square test was used to compare the proportion of cases and controls who made errors in assessing individual coloured clinical photographs, and the proportions with high levels of confidence. Student unpaired t-test was used to compare cases with controls for mean number of AFB counted by them.
Results
Of the 1177 students available during the period of the study, 1022 (86.3%) were screened (Ishihara chart); 35 (3.4%), all men, were found to have CCVD; 30 consented to participate in the study and an equal number of controls were enrolled. Both the study and control groups had 4 postgraduate students each. Most students with CCVD (24/30; 80%) reported that they were first diagnosed to be colour vision deficient after admission to the medical course. While students with CCVD misread 18–30 slides on Ishihara testing (mean [SD]: 24.6 [3.53]), controls made no errors.
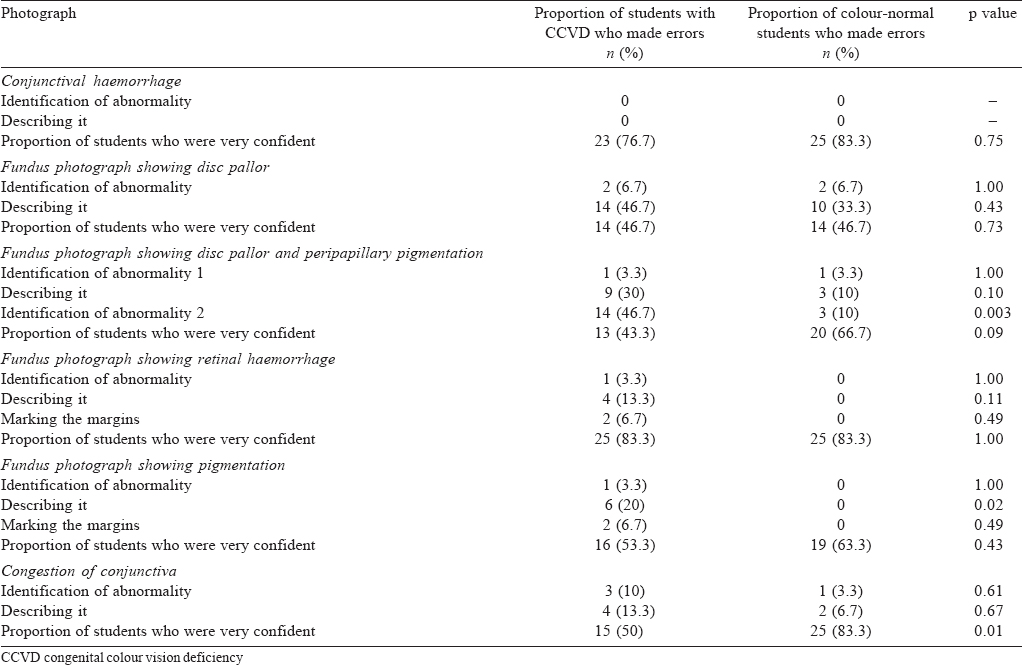
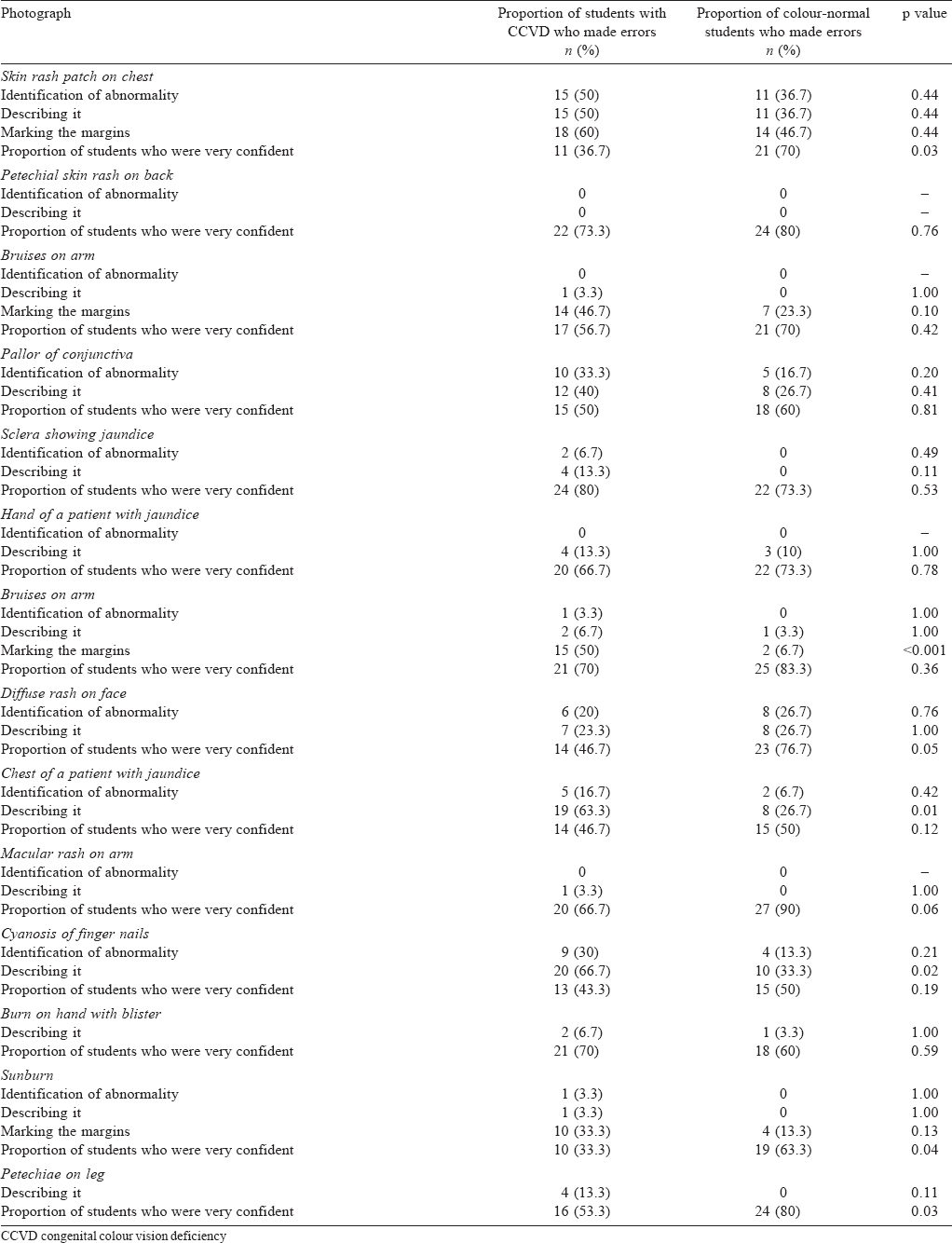
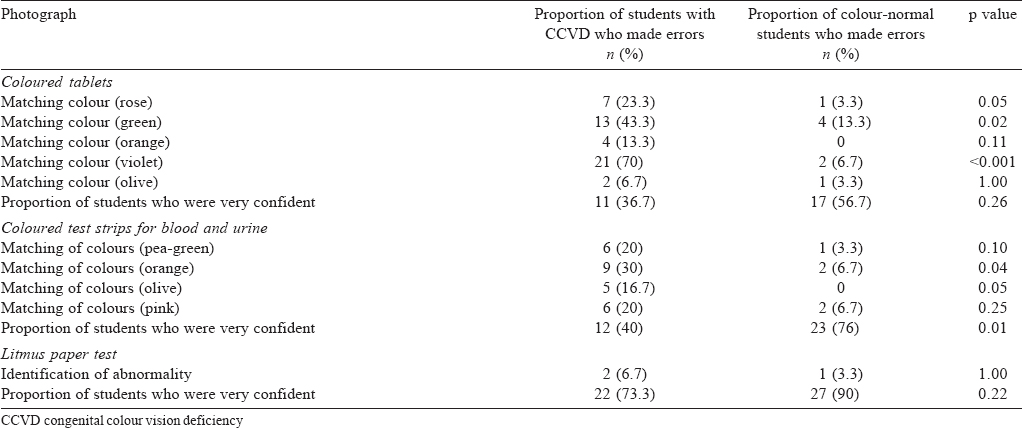
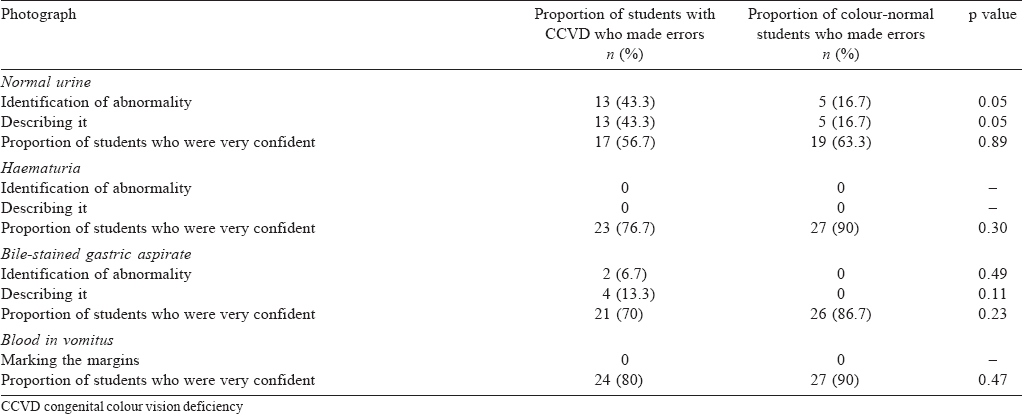
Students with CCVD made 5–26 errors out of 75 items in 35 colour-dependent photographs (mean [ SD] 13.17 [5.87]), whereas colour-normal students made 2–13 errors (mean [ SD] 5.53 [3.04]; p<0.001). Overall, students were very confident of their findings during objective testing regardless of whether they had CCVD or were colour-normal [Table - 1], [Table - 2], [Table - 3], [Table - 4], [Table - 5], [Table - 6]. In the case of pictures displaying congestion of conjunctiva, skin rash, sunburn, petechiae, Congo red staining, and test strips for blood and urine, we found that significantly fewer students with CCVD were confident of their findings.
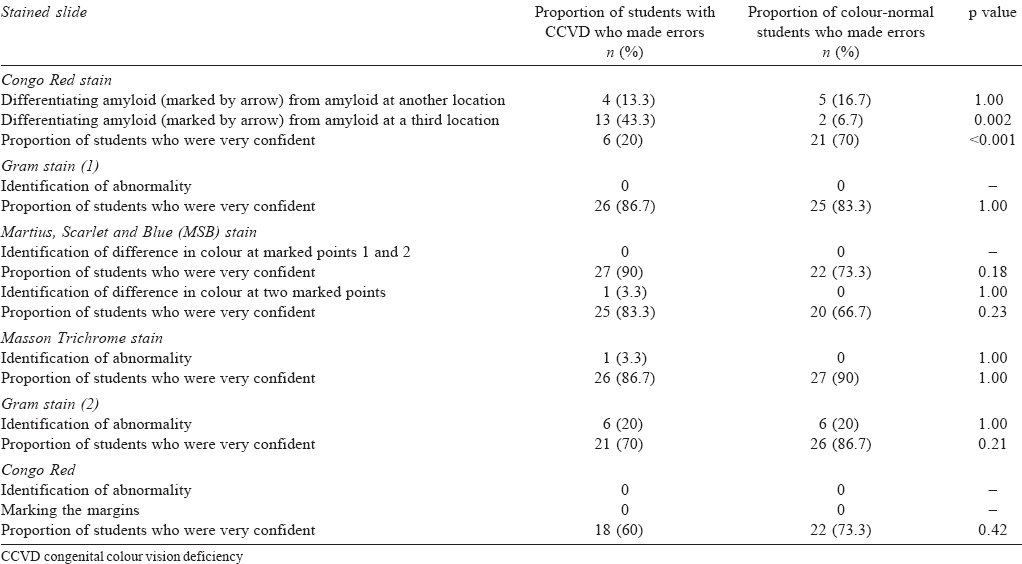

There was a significant difference between the number of AFB (Ziehl–Neelsen staining) counted by students with CCVD (5.3 [4.04]; range 0–24) compared to colour-normal controls (7.8 [0.89]; range 6–10; p=0.02). There was no difference in the confidence level (0.33). Only one student with CCVD counted 8 bacilli correctly compared to 15 colour-normal students.
Discussion
The prevalence of CCVD among our students, at 3.42%, was lower than that reported from the general population (6%–8%).[1],[6] The reason could be either because there are only a limited number of students in our institution, or since most students were screened for CCVD at the time of admission, those with a positive diagnosis chose other (non-medical) streams of education.
On objective testing, students with CCVD and those who were colour normal made errors in interpretation of coloured signs. Some areas of concern revealed by the study are discussed below.
In the specialty of ophthalmology, though they were able to detect the presence of an abnormality on fundus photographs, students with CCVD could not decipher the colour. Contrast difference between pigmented and surrounding non-pigmented areas can assist in defining abnormal areas; however, for correct description of colour, the perception of colour needs to be normal.[7] For the specialty of otorhinolaryngology, they appeared to have little difficulty; as has been reported by other researchers.[8],[9],[10] When assessed for the colour of medicinal tablets and for colour changes in colorimetric tests, students with CCVD had difficulty with green and orange colours. Such errors made during practice could result in drug over-dosage and/or side-effects, and in diagnostic mismanagement.[11] Though they managed to decipher most photographs depicting body fluids, in the photograph of normal urine, significantly more students with CCVD diagnosed it as abnormal. False-positive results could adversely impact patient management.[9] Ziehl–Neelsen staining of AFB threw up some interesting findings; only 1 student with CCVD was able to count the exact number of bacilli correctly compared to nearly half the colour-normal controls. Moreover, while most students counted fewer bacilli, one student with CCVD over-counted almost three-times more bacilli. These situations could result in a false-negative or false-positive diagnosis.[9]
Based on our findings, augmented by evidence from the literature, we suggest ways in which a medical practitioner with CCVD could practise safely. If she wishes to become an ophthalmologist, she could work in anterior segment mainly, while for retinal evaluations, she could have peers to corroborate her findings.[7],[8],[10] Persons with CCVD should avoid working with drugs available in loose form. They should, instead, rely only on strips where they can read the name and strength of the drug. With respect to colorimetry, studies have shown that with the chromaticity of charts currently in use, there is usually no problem in detecting whether or not glucose is present. Errors may occur only during quantitative testing;[11] therefore, to prevent errors or reduce their significance, digital instruments could be used. Where changes in colour of the skin or body fluids are concerned, we suggest caution during practice; a colour-normal colleague could be asked to corroborate the findings before giving an opinion. Our students with CCVD had difficulties in pathology and bacteriology. Researchers argue that CCVD should not impact the work in pathology as much of it relies on morphology and arrangement of cells.[12] Moreover, a magenta filter has been found to help.[13] Based on the nature of errors we found, perhaps practitioners with CCVD could adopt safe practice through peer-corroboration of findings where special stains are involved.[8],[10]
Confidence levels during objective assessment deserve special mention. For some photographs, students with CCVD recorded significantly lower confidence levels even though the diagnosis was correct. Students with low confidence should be encouraged to consult others to corroborate their findings. Over time, this practice could reinforce their diagnostic skills and improve their confidence level.[8],[10]
In most cases, however, the errors were associated with a high level of self-reported confidence. The photographs where this happened were related to skin colour changes, pigmentation of ocular fundus, and coloured medication (particularly green colour). Practitioners with CCVD who are confident about their judgement are less likely to take precautions or take help from others and could potentially mismanage patients. To prevent mishaps, after getting evaluated for their particular degree and type of deficiency, they should strive to become better aware of their limitations, if any, and find ways to deal with them so as to ensure patient safety.[1]
Our study had some limitations. Photographs of colour-dependent signs were used instead of real clinical situations. In addition, all tests were done under standard illumination, while such good illumination may not be present in real-life situations. Further, history was not provided; additional clues can be gleaned from a careful history. We also did not provide other findings that could have helped in the diagnosis. Although our results show that students with CCVD face difficulties in some of the colour-dependent tasks, it cannot be extrapolated that it would lead to wrong diagnosis or mismanagement of patients. Only on further longitudinal research can we determine whether self-reported difficulties will translate into problems during clinical practice. Because the number of postgraduate students recruited in our study were few (4; 13.3%), we did not attempt to compare the number of errors they made with the errors made by undergraduate students. Thus, we cannot comment on whether postgraduate students—since they have spent more time in clinics and laboratories than undergraduate students—learn to understand and compensate for the CCVD and thus make fewer errors in practice. Further research could be done in this area.
Based on our results, we anticipate that medical students with CCVD could have problems with the use of special stains in the fields of histology, pathology, haematology and microbiology; with respect to colour changes in skin and mucosa in dermatology, paediatrics and medicine; in biochemistry, with respect to colorimetric tests; and in fundus examination. Researchers have found that persons with CCVD use other cues to avoid making mistakes. They focus harder on history-taking; use brightness and contrast to differentiate colours; observe closely, or use touch for skin rashes; and many ask for help.[5],[10] We should recommend these practices to our students soon after we diagnose them at admission. We do not suggest concessions for students with CCVD during formative or summative assessments; however, during training, teachers could give them several opportunities to practise and also advise them on non-colour-dependent cues that could aid correct diagnosis.
In India, CCVD is not a contraindication for joining the medical profession; thus, the issues related to CCVD in medical practitioners in India have never been debated. In the West, people with colour vision deficiency are not debarred from training in a specialty of choice.[5] Since the anomaly in colour vision is extremely variable, no two individuals will have the same level of difficulty so each one must be considered on an individual basis. We would have liked to evaluate the effect of type of and severity of colour blindness on performance; however, we used the Ishihara chart to screen students for colour vision deficiency. This chart, though universally used for screening purposes, is not reliable to grade the severity of colour vision or classify its type. The recommended method to grade and classify CCVD is to use Farnsworth Panel D-15 or Farnsworth–Munsell 100-hue tests;[14] however, these are expensive and not available to us. Whereas the Ishihara chart is widely available in medical institutions across India, the Farnsworth Panel D-15 and Farnsworth–Munsell 100-hue tests are available at only a few, select centres because of their high cost.
We recommend that students who are admitted to a medical course should be screened at the time of admission, not to discourage them from taking the course, but to make them aware of the type and severity of the colour vision deficiency. They should, thereafter, undergo counselling to know their limitations, if any. They will then be in a much stronger position to acknowledge the problems they have, be ready to seek advice, and be better equipped to find ways to overcome difficulties to practise safely.
| 1. | Spalding JA. Colour vision deficiency in the medical profession. Br J Gen Pract 1999;49:469–75. [Google Scholar] |
| 2. | Reiss MJ, Labowitz DA, Forman S, Wormser GP. Impact of color blindness on recognition of blood in body fluids. Arch Intern Med 2001; 161:461–5. [Google Scholar] |
| 3. | Rigby HS, Warren BF, Diamond J, Carter C, Bradfield JW. Colour perception in pathologists : The Farnsworth-Munsell 100-hue test. J Clin Pathol 1991;44:745–8. [Google Scholar] |
| 4. | Poole CJ, Hill DJ, Christie JL, Birch J. Deficient colour vision and interpretation of histopathology slides: Cross sectional study. BMJ 1997;315:1279–81. [Google Scholar] |
| 5. | Spalding JA. Medical students and congenital colour vision deficiency: Unnoticed problems and the case for screening. Occup Med (Lond) 1999;49:247–52. [Google Scholar] |
| 6. | Simunovic MP. Colour vision deficiency. Eye (Lond) 2010;24:747–55. [Google Scholar] |
| 7. | Cockburn DM. Confessions of a colour blind optometrist. Clin Exp Optom 2004;87:350–2. [Google Scholar] |
| 8. | Campbell JL, Spalding JAB, Mir FA. The description of physical signs of illness in photographs by physicians with abnormal colour vision. Clin Exp Optom 2004;87:,334–8. [Google Scholar] |
| 9. | Campbell JL, Griffin L, Spalding JAB, Mir FA. The effect of abnormal colour vision on the ability to identify and outline coloured clinical signs and to count stained bacilli in sputum. Clin Exp Optom 2005;88:376–81. [Google Scholar] |
| 10. | Campbell JL, Spalding AJ, Mir FA, Birch J. Doctors and the assessment of clinical photographs—does colour blindness matter? Br J Gen Pract 1999;49:459–61. [Google Scholar] |
| 11. | Campbell JL, Spalding JA, Mir FA, Birch J. Doctors and the assessment of blood glucose testing sticks: Does colour blindness matter? Br J Gen Pract 2000;50: 393–5. [Google Scholar] |
| 12. | Goudie RB. Colour deficient vision should not prevent a career in histopathology. BMJ 1998;316:1750. [Google Scholar] |
| 13. | Olson IA. The use of colour filters by students with congenital colour defects in the learning of histology. Med Biol Illus 1971;21:52–3. [Google Scholar] |
| 14. | Pandey N, Chandrakar AK, Garg ML. Tests for color vision deficiency: Is it time to revise the standards? Indian J Ophthalmol 2015;63:752–3. [Google Scholar] |
Fulltext Views
4,567
PDF downloads
1,574




