Translate this page into:
Prevalence and determinants of sleep disorders in a community in rural southern India
2 Department of Preventive and Social Medicine, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry 605006, India
3 Department of Neurology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry 605006, India
4 Centre for Operational Research (COR), International Union against Tuberculosis and Lung Diseases, Paris, France
Corresponding Author:
Kariyarath Cheriyath Premarajan
Department of Preventive and Social Medicine, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry 605006
India
kcpremarajan@yahoo.com
| How to cite this article: Ramaswamy G, Premarajan KC, Kar SS, Narayan SK, Thekkur P. Prevalence and determinants of sleep disorders in a community in rural southern India. Natl Med J India 2020;33:132-136 |
Abstract
Background. We assessed the prevalence of sleep disorders among people above 15 years of age from a rural area of Puducherry, south India.Methods. We did a community-based cross-sectional study among people residing in four service area villages of a rural primary health centre in Puducherry, India. Probability sampling techniques were used to select participants. The Pittsburgh Sleep Quality Index was administered to detect sleep disorders among the participants. The data were entered and analysed using EpiData entry 3.1 and Stata 12 software, respectively. Association between various individual factors and sleep disorders was assessed using generalized linear models adjusting for clustering at the household level and expressed as prevalence ratio with 95% confidence interval (CI).
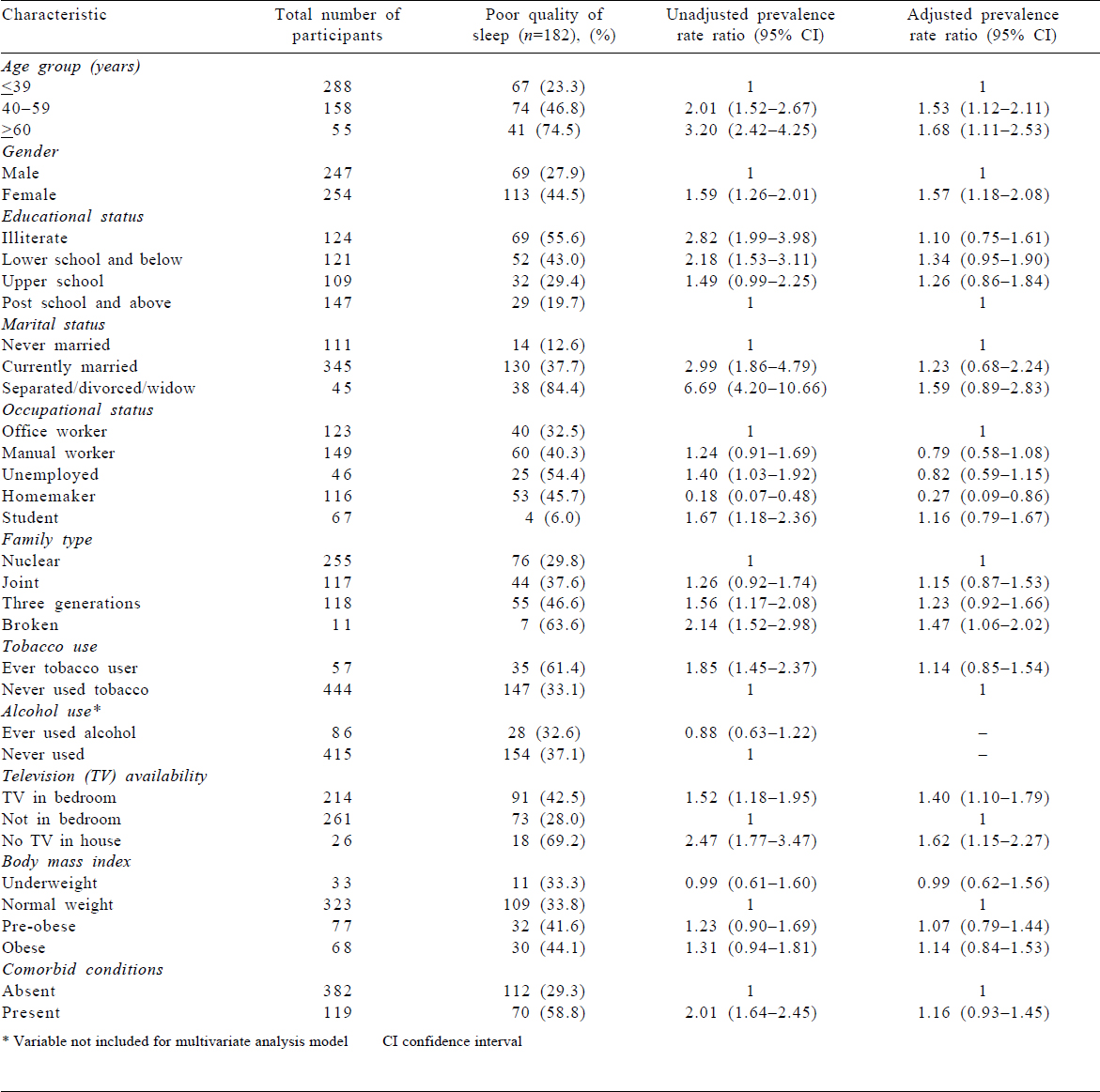
Results. The mean (SD) age of the 501 participants was 38.3 (15.4) years. Poor quality of sleep was present in 36.3% (95% CI 32.2%–40.6%). In multivariate generalized linear model, age >60 years (adjusted prevalence rate ratio [aPRR] 1.68; 95% CI 1.11–2.53), female sex (aPRR 1.57; 95% CI 1.18–2.08), living in a broken family (aPRR 1.47; 95% CI 1.06–2.02) and having a television in their sleeping room (aPRR 1.40; 95% CI 1.40–1.79) were independently associated with poor quality of sleep.
Conclusions. A high prevalence suggests that sleep disorders are a problem in the rural community too. Capacity building among the existing health workforce to identify and treat sleep disorders and health education activities focusing on sleep hygiene among the general public are needed to tackle sleep disorders in the community.
Introduction
Sleep disorder is an emerging public health problem.[1] Any deficiency in either quality or quantity of sleep is considered a sleep disorder. The International Classification of Diseases-10 classifies sleep disorders into six symptoms based on major categories, namely insomnia, hypersomnia, sleep-related breathing disorders, parasomnia, circadian rhythm sleep disorders and sleep-related movement disorders.[2] It is estimated that globally 25%–30% of adults suffer with at least one of the sleep disorders.[3],[4],[5],[6] The study on global ageing and adult health and Collaborative Research on Ageing in Europe reported that 9.2% of individuals aged 50 years and above had some sleep problems.[7] Panda et al. in a hospital-based study among apparently healthy individuals reported that 20%–34.4% of Indians in the southern part of the country suffer from sleep disorders.[8]
Sleep disorder over short duration leads to difficulty in concentration, flawed judgement, poor memory, psychological stress and deficient problem-solving skills. This condition in the long run leads to the development of various non-communicable diseases such as hypertension, diabetes mellitus, cardiovascular diseases, kidney disease and suicidal tendencies.[9] Apart from effects on their own life, accidents related to drivers with sleep disturbance endanger others’ lives too.[10]
Although sleep disorder has proven adverse effects on health, there is a lack of advocacy for prioritizing sleep disorders as an emerging public health problem in developing countries. This is mainly due to paucity of the literature on the burden of sleep disorders in countries. Although community-based studies on sleep disorders in Canada, Brazil and China have estimated the burden of sleep disorders, these estimates may not be applicable to India.[3],[4],[5],[11],[12] In India, research on the burden of sleep disorders has been restricted primarily to specific groups such as students or patients with Parkinson disease or renal failure.[13],[14] To the best of our knowledge, there are no published community-based studies available on the burden of sleep disorders from rural India.
We, therefore, did a community-based cross-sectional study among people above 15 years of age residing in a rural area of Puducherry, south India (i) to determine the prevalence of sleep disorders using the validated Pittsburgh Sleep Quality Index (PSQI) scale, and (ii) to identify the sociodemographic and behavioural characteristics associated with sleep disorders.
Methods
Study design and setting
A community-based cross-sectional analytical study was carried out in the service area of a selected primary health centre (PHC) located 15 km from Puducherry, a Union Territory of India. The PHC functions under the tertiary care teaching institute located in the city of Puducherry and caters to the healthcare needs of 10 087 individuals spread over four villages—Ramanathapuram Thondamanatham, Pillayarkuppam and Thutipet.
Study population
The study was done among individuals aged >15 years and residing for >6 months in the service area of the selected PHC. We excluded individuals with well-known secondary causes of dyssomnia due to hepatic, renal, respiratory and cardiac failure. Pregnant females were also excluded from the study.
Sample size and sampling technique
The minimum sample size was calculated to be 500 individuals using OpenEpi software. The sample size was calculated assuming the prevalence of sleep disorder to be 18% based on a previous study,[8] absolute precision of 5%, confidence level of 95%, non-response rate of 10% and design effect of 1.5 to adjust for clustering at the household level. The number of individuals to be studied in each village of the service area was decided through proportionate to size sampling. The proportionate to size weights were based on the proportion of individuals >15 years of age in each village. Based on prior knowledge on household size (each house with at least three individuals >15 years of age) in the study villages, the number of houses to be included for study from each village was calculated. The houses were selected using systematic random sampling and right-hand rule was followed during the survey. All individuals >15 years of age in the selected houses were included in the study.
Study tool and study procedure
A pre-tested and semi-structured interview schedule was prepared to capture the sociodemographic details, chronic disease status and television watching characteristics of the study participants. Behavioural factors such as tobacco and alcohol use were captured as per the WHO STEPwise approach to surveillance questionnaire.[15] To capture sleep disorders among the participants, PSQI was used after obtaining permission from copyright holders.[16] The questionnaire was translated into Tamil and back-translated to English and pre-tested before the conduct of the study.
Data collection was done from January 2014 to December 2014. After obtaining informed consent, face-to-face interview was conducted in adequate privacy. The height, weight, waist and hip circumference were measured according to STEPS anthropometric measurement guidelines. Eligible individuals were considered as non-responders when the investigator failed to interview even after making two additional visits.
Operational definitions
Individuals with Global PSQI score of >5 were considered to have poor quality of sleep or sleep disorder.[16]
Data entry and statistical analysis
Data were entered using EpiData data entry software version 3.1 and analysis was done using Stata 12 software. Prevalence of sleep disorder was expressed as percentage with 95% confidence interval (CI). The association between the individual’s characteristics and poor quality of sleep was assessed using generalized linear models with Poisson distribution and log link function adjusting for clustering at the household level. Variables with p<0.1 in the bivariate model were included for the multivariate generalized linear models to assess the independent effect of study participants’ characteristics. As the prevalence of poor quality of sleep was >10% in the study population, prevalence ratio with 95% CI was used to express the association in both bivariate and multivariate model. The calculated prevalence ratios in both bivariate and multivariate models were adjusted for anticipated clustering at the household level.
Ethical approval
The scientific approval for the conduct of the study was obtained from JIPMER Scientific Advisory Committee and ethical approval for the study was obtained from the Institute Ethics Committee. All the procedures carried out in this study adhered to ICMR’s Ethical guidelines for biomedical research on human participants (2006).
Results
Five hundred and one individuals were included in the study with response rate of 98%. The mean (SD) age of the participants was 38.3 (15.4) years with 254 (50.7%) females. The majority of study participants were from a nuclear family (50.9%) and 194 (38.8%) were in class IV of socioeconomic status according to the Modified BG Prasad’s classification.
Of the 501 participants, 86 (17%) had consumed alcohol and 57 (11%) had consumed tobacco at least once. Almost 23% of participants had at least one chronic disease condition such as diabetes mellitus, hypertension, cardiovascular disease or arthritis, and of them 29% had two or more concomitant chronic disease conditions. More than half (52%) of the study participants had abdominal obesity [Table - 1].
Quality of sleep
The prevalence of poor quality of sleep among the study participants was 36.3% (95% CI 32.2%–40.6%). The median (interquartile range) Global PSQI score of the participants was 4 (2–8). None of the study participants were diagnosed with any form of sleep disorders before the study.
Sleep pattern [Table - 2]

The mean (SD) hours spent in bedtime by the study participants was 7.6 (1.4) hours, whereas the actual mean (SD) hours of sleeping were 6.4 (1.5) hours. The time taken to fall asleep (sleep latency) ranged from 5 minutes to 4 hours. Short duration of sleep (<6 hours/day) was reported by 92 (18.4%) participants (36 [14.6%] males and 56 [22.0%] females). A similar proportion of study participants reported sleep latency of >30 minutes/day. None of the participants were using any form of medication for sleeping. Those who had short sleep duration had 4.2 times (95% CI for prevalence ratio 3.47–5.00) higher chance of poor quality of sleep compared to those who slept for at least 6 hours a day.
Factors associated with poor quality of sleep
After adjusting for other variables, individuals >40–59 years (adjusted prevalence rate ratio [aPRR] 1.53; 95% CI 1.12–2.11), geriatric age group (aPRR 1.68; 95% CI 1.11–2.53), female sex (aPRR 1.57; 95% CI 1.18–2.08), living in a broken family (aPRR 1.47; 95% CI 1.06–2.02), non-availability of television at home (aPRR 1.62; 95% CI 1.15–2.27), television in bedroom (aPRR 1.40; 95% CI 1.40–1.79) were found to have a significantly higher association with poor quality of sleep. Homemakers were less likely to have (aPRR 0.27; 95% CI 0.09–0.86) poor quality of sleep compared to those who worked in the office.
Discussion
We found that over one-third of our study participants had a poor quality of sleep. The individual-level characteristics such as age >40 years, female sex, being homemaker, living in a broken family were independently associated with having poor quality of sleep.
The prevalence of poor quality of sleep from various community-based studies ranges from 26% to 46.6%.[3],[4],[17],[18],[19],[20] The study from an urban community of Pennsylvania (30%) and Iran (37%) showed almost similar prevalence as in our study.[3],[19] The community-based study done in China showed relatively lower prevalence of 26%.[4] The Chinese study had excluded individuals with chronic comorbid conditions such as hypertension, diabetes, cardiovascular disease and any form of chronic pain. Apart from sociobehavioural, ethnic and cultural differences, even inclusion of individuals with chronic morbid conditions might have resulted in a higher prevalence of sleep disorder in our study compared to that of Lou et al. At least one of four individuals had any one chronic morbid condition in our study.[4] Panda et al. reported poor quality of sleep (6%) among apparently healthy people accompanying patients consulting the neurology outpatient department in Bengaluru. This difference in prevalence maybe due to the inclusion of only healthy individuals aged 15–55 years in the Bengaluru study who cannot form a true representative sample of a rural or urban community. Furthermore, the study participants were predominantly (58%) males.[8]
The study reported around 20% individuals with subjective poor quality of sleep, sleep latency of >30 minutes and <6 hours of sleep per day. Community-based studies conducted in other parts of the world reported 6%–25% of the study participants had <6 hours of sleep.[20],[21]
Our study showed that advancing age and female sex were associated with poor quality of sleep. The results are consistent with the results of studies by Luo et al.[22] and Lou et al.[5], albeit the latter study reported an inverse relationship with male gender and sleep quality. Apart from hormonal disturbances which may result in mood swings and sleep disturbances, social inequities and societal expectations of the community from females may also be a potential reason for relatively higher prevalence of poor quality of sleep among females. Biological plausibility of the association of female sex with poor quality of sleep needs to be explored further. An interesting association of homemakers with lower chance of poor quality of sleep was observed in our study. Studies conducted in other parts of the world reported varied associations with different types of occupation and sleep disorders.[23] The study did not show any independent association of behavioural factors (tobacco and alcohol), obesity or comorbid conditions with poor quality of sleep. Studies conducted elsewhere provide varied results.[4],[18],[22] The difference in sociocultural, ethnic, lifestyle, behavioural factors, cut-off values used for classifi-cation of obesity, inclusion criteria adopted by the studies and methods followed during analysis maybe the reason for the differences observed between the studies.[4],[5],[13],[19],[24]
In our study, participants who had a television in the bedroom reported poor quality of sleep. This was because of late night use of television by the partners. An interesting observation was that some people who did not have a television in their home also had a significantly higher chance for poor quality of sleep. On subfactor analysis, these individuals were predominantly elderly or living alone. Depressive moods may be the cause of poor sleep in such persons and a positive influence that television plays in combating loneliness and depression needs to be explored in the management of insomnia in the elderly and among those living alone.
The proportion of tobacco users (11%) was relatively less compared to the national data on tobacco users (28.6%).[25] However, our study had higher reported prevalence of tobacco and alcohol use from a similar study setting (5%).[26] The results have to be interpreted with caution as the social desirability bias may be a factor for such a difference.
The strengths of our study include a large representative sample with probability sampling from a rural population of India. The study tool used was linguistically validated to the need of the community. The single investigator who was well-versed in the local language, Tamil, was involved in data collection and hence avoided the inter-observer bias during interview of the study participants. The association between the participant’s factors and sleep disorders were expressed as prevalence rate with adjustment for clustering at the household level which thereby avoided overestimation of the strength of association.
The study has a few limitations. The sleep disorder identified among the study participants was not confirmed with polysomnographic evaluation. With the compromised sensitivity and specificity of the study tool, there may be slight difference in the true prevalence compared to apparent prevalence of sleep disorders as assessed in the study. The causal effect of sociodemographic and behavioural factors with sleep disorder cannot be established which is the inherent defect in cross-sectional studies. In addition, the psychological stress of the individuals was not assessed in our study, which may be a cause for sleep disorders.
With a high burden of sleep disorder, there is a need to develop a public health strategy to effectively screen all adults for sleep disorders and conduct community-level awareness campaign regarding sleep hygiene. Targeted intervention on sleep disorders for the high-risk groups such as the elderly, those with a low education status, currently married and those who live in a broken family can be carried out to reduce the burden of sleep disorders. Task shifting and involvement of grassroot workers have to be tried to do such activities to overcome a limited workforce in resource-constrained settings. The influence of electronic and communication devices on individuals sleep has to be explored further.
Conclusions
One of three individuals screened in a rural community of southern India were found to have poor quality of sleep. Advancing age, female sex, living in broken family, having a television in the bedroom and not having a television at home were independently associated with poor quality sleep. Creating awareness about sleep disorders, screening among the above-mentioned risk groups and diagnosing sleep disorders early are crucial to tackle this unmet public health issue. There is a dire need in healthcare systems in developing countries to focus on a potential pandemic of sleep disorder which is a risk factor for several non-communicable disorders.
Acknowledgements
We would like to acknowledge the authors and copyright holders (MapiTrust) of PSQI for their support and permission for the conduct of this research. We would also like to acknowledge the PHC medical officer, staff and village leaders for their cooperation and support for this study.
Conflicts of interest. None declared
| 1. | Stranges S, Tigbe W, Gómez-Olivé FX, Thorogood M, Kandala NB. Sleep problems: An emerging global epidemic? Findings from the INDEPTH WHO-SAGE study among more than 40,000 older adults from 8 countries across Africa and Asia. Sleep 2012;35:1173–81. [Google Scholar] |
| 2. | Sleep Disorders–ICD-10 Codes and Names. American Sleep Association. Available at www.sleepassociation.org/sleep-disorders-icd-10–codes-names/ (accessed 11 Jan 2016). [Google Scholar] |
| 3. | Asghari A, Farhadi M, Kamrava SK, Ghalehbaghi B, Nojomi M. Subjective sleep quality in urban population. Arch Iran Med 2012;15:95–8. [Google Scholar] |
| 4. | Lou P, Chen P, Zhang L, Zhang P, Chang G, Zhang N, et al. Interaction of sleep quality and sleep duration on impaired fasting glucose: A population-based cross-sectional survey in China. BMJ Open 2014;4:e004436. [Google Scholar] |
| 5. | Lou P, Chen P, Zhang L, Zhang P, Yu J, Zhang N, et al. Relation of sleep quality and sleep duration to type 2 diabetes: A population-based cross-sectional survey. BMJ Open 2012;2 pii:e000956. [Google Scholar] |
| 6. | Léger D, Partinen M, Hirshkowitz M, Chokroverty S, Hedner J; EQUINOX (Evaluation of daytime QUality Impairment by Nocturnal awakenings in Outpatient’s eXperience) Survey Investigators, et al. Characteristics of insomnia in a primary care setting: EQUINOX survey of 5293 insomniacs from 10 countries. Sleep Med 2010;11:987–98. [Google Scholar] |
| 7. | Koyanagi A, Garin N, Olaya B, Ayuso-Mateos JL, Chatterji S, Leonardi M, et al. Chronic conditions and sleep problems among adults aged 50 years or over in nine countries: A multi-country study. PLoS One 2014;9:e114742. [Google Scholar] |
| 8. | Panda S, Taly AB, Sinha S, Gururaj G, Girish N, Nagaraja D, et al. Sleep-related disorders among a healthy population in South India. Neurol India 2012;60:68–74. [Google Scholar] |
| 9. | Determinants of shortened, disrupted, and mistimed sleep and associated metabolic health consequences in healthy humans. Available at www.diabetes.diabetes journals.org/content/64/4/1073.long (accessed on 11 Jan 2016). [Google Scholar] |
| 10. | Facts and Stats: Drowsy Driving – Stay Alert, Arrive Alive. Available at www.drowsydriving.org/about/facts-and-stats/ (accessed on 11 Jan 2016). [Google Scholar] |
| 11. | von Schantz M, Taporoski TP, Horimoto AR, Duarte NE, Vallada H, Krieger JE, et al. Distribution and heritability of diurnal preference (chronotype) in a rural Brazilian family-based cohort, the Baependi study. Sci Rep 2015;5:9214. [Google Scholar] |
| 12. | Pahwa P, Karunanayake CP, Hagel L, Gjevre JA, Rennie D, Lawson J, et al. Prevalence of High Epworth Sleepiness Scale scores in a rural population. Can Respir J 2012;19:e10–14. [Google Scholar] |
| 13. | Giri P, Baviskar M, Phalke D. Study of sleep habits and sleep problems among medical students of Pravara Institute of Medical Sciences Loni, Western Maharashtra, India. Ann Med Health Sci Res 2013;3:51–4. [Google Scholar] |
| 14. | Shah N, Bang A, Bhagat A. Indian research on sleep disorders. Indian J Psychiatry 2010;52:S255–S259. [Google Scholar] |
| 15. | World Health Organization. The STEPS Instrument and Support Materials. World Health Organization. Available at www.who.int/chp/steps/instrument/en/ (accessed on 13 Jan 2016). [Google Scholar] |
| 16. | Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193–213. [Google Scholar] |
| 17. | Tai SY, Wang WF, Yang YH. Current status of sleep quality in Taiwan: A nationwide walk-in survey. Ann Gen Psychiatry 2015;14:36. [Google Scholar] |
| 18. | Wong WS, Fielding R. Prevalence of insomnia among Chinese adults in Hong Kong: A population-based study. J Sleep Res 2011;20:117–26. [Google Scholar] |
| 19. | Jennings JR, Muldoon MF, Hall M, Buysse DJ, Manuck SB. Self-reported sleep quality is associated with the metabolic syndrome. Sleep 2007;30:219–23. [Google Scholar] |
| 20. | Carroll JE, Irwin MR, Stein Merkin S, Seeman TE. Sleep and multisystem biological risk: A population-based study. PLoS One 2015;10:e0118467. [Google Scholar] |
| 21. | Lu K, Chen J, Wu S, Chen J, Hu D. Interaction of sleep duration and sleep quality on hypertension prevalence in adult Chinese males. J Epidemiol 2015;25:415–22. [Google Scholar] |
| 22. | Luo J, Zhu G, Zhao Q, Guo Q, Meng H, Hong Z, et al. Prevalence and risk factors of poor sleep quality among Chinese elderly in an urban community: Results from the Shanghai aging study. PLoS One 2013;8:e81261. [Google Scholar] |
| 23. | Sun W, Yu Y, Yuan J, Li C, Liu T, Lin D, et al. Sleep duration and quality among different occupations – China national study. PLoS One 2015;10:e0117700. [Google Scholar] |
| 24. | Ebrahimi MH, Sadeghi M, Dehghani M, Niiat KS. Sleep habits and road traffic accident risk for Iranian occupational drivers. Int J Occup Med Environ Health 2015;28:305–12. [Google Scholar] |
| 25. | Centers for Disease Control. Global Adult Tobacco Survey GATS Objectives GATS 2 Highlights: India Fact Sheet; 2016. Available at www.who.int/tobacco/ surveillance/survey/gats/GATS_India_2016–17_FactSheet.pdf (accessed on 12 Aug 2018). [Google Scholar] |
| 26. | Bharati DR, Pal R, Kar S, Rekha R, Yamuna TV, Basu M, et al. Prevalence and determinants of diabetes mellitus in Puducherry, South India. J Pharm Bioallied Sci 2011;3:513–18. [Google Scholar] |
Fulltext Views
5,520
PDF downloads
2,773




