Translate this page into:
Prevalence of substance use and substance use disorder in medically ill patients: A cross-sectional, hospital-based study from India
Correspondence to RAVINDRA RAO, RAKESH CHADDA; drrvrao@gmail.com; drrakeshchadda@gmail.com
[To cite: Rao R, Chadda R, Kathiresan P, Gupta R, Bhad R, Mishra AK, et al. Prevalence of substance use and substance use disorder in medically ill patients: A cross-sectional, hospital-based study from India. Natl Med J India 2024;37:131–7. DOI: 10.25259/NMJI_211_2022]
Abstract
Background
Untreated co-occurring substance use and substance use disorders (SUDs) in patients with medical conditions may be associated with unfavourable medical outcomes. Understanding the prevalence of substance use and SUDs among patients admitted to hospital for medical illness may help in developing appropriate strategies to manage SUDs in this population and improve the outcomes of medical illness. We assessed the prevalence of substance use and SUDs among patients admitted for medical illnesses and the association between substance use and medical illness.
Methods
This cross-sectional study was done in an in-patient setting in a multidisciplinary teaching medical institution in India. Using systematic sampling, adult patients admitted in various departments for at least 24 hours were interviewed using standard instruments by psychiatrists trained in the study methodology.
Results
Two hundred and ninety patients participated. Their mean (SD) age was 42.2 (15.6) years. One hundred and nine participants (37.6%) reported lifetime use of any psychoactive substance, with tobacco being the most common substance used (91, 31.4%), followed by alcohol (69, 23.8%) and cannabis (12, 4.1%). Lifetime alcohol use was significantly associated with diseases of the circulatory system. Lifetime use of any substance or of alcohol, and current use of any substance or tobacco were significantly associated with injuries, poisoning and other consequences of external causes.
Conclusions
A large proportion of patients hospitalized for medical illness reported the use of psychoactive substances or had SUDs. The use of some of these substances was also associated with injuries as well as diseases of the circulatory system.
INTRODUCTION
Substance use and substance use disorders (SUDs) are associated with complications in many spheres of the user’s life, including occurrence of various medical conditions. Untreated co-occurring SUDs in patients presenting for medical conditions may be associated with unfavourable medical outcomes, including prolonged hospital stay, readmission for health conditions and more frequent need for emergency care.1–5 Thus, it is important to study the prevalence of substance use and SUDs among patients admitted in medical facilities as it may help in developing appropriate strategies to identify and treat SUDs in the hospital setting.6,7
The prevalence of substance use and SUDs in hospital settings varies, depending on the type of health facility (primary care or hospital), hospital setting (outpatient, inpatient or emergency), across various hospital services and by patient characteristics. For example, the prevalence of alcohol use in attendees of accident and emergency services across different studies has ranged from 12% to as high as 37.5%.8–10 Similarly, a meta-analysis of alcohol use disorder in hospitals in the UK found that approximately 1 in 5 patients suffer from harmful alcohol use, while 1 in 10 patients suffer from alcohol dependence syndrome.11 The study also found that the prevalence of alcohol dependence is higher in accident and emergency services compared to general wards. Similarly, the prevalence of alcohol use and alcohol use disorder is higher in men and in younger adults than in the older ones.12
In India, a number of people use various psychoactive substances. As per a recent national survey on substance use, the prevalence of alcohol, cannabis and opioid use in those aged between 10 and 75 years was 14.6%, 2.8% and 2.1%, respectively.13 However, studies that have assessed the prevalence of substance use in general healthcare settings in the country are limited. Some of these have analysed referrals to the psychiatry department from other departments of the hospital,14,15 whereas others have focused on the use of one substance rather than on the use of all substances and SUDs.16–19 Furthermore, some studies have evaluated patients from one department rather than from all departments.20–22 It is important to assess the prevalence of various psychoactive substances and SUDs in patients admitted to hospital in different medical specialties as it may help develop appropriate strategies for screening and treating patients with SUDs in the hospital setting.
We assessed the use of psychoactive substances as well as SUDs among patients admitted to different specialties in a tertiary care hospital in India. We also assessed whether substance use was associated with the medical illness for which the patient was admitted to the hospital.
METHODS
This cross-sectional study was done in an inpatient setting of a tertiary care multidisciplinary teaching medical institution in northern India.
The hospital has about 2500 beds, including intensive care units (ICU) beds. Anticipating the prevalence of any psychoactive SUD (including tobacco use disorder) to be 10%, confidence interval 95%, 5% absolute precision and design effect 2.5, we calculated that we would require a sample size of 317.
The first step in sampling in our study was choosing the bed. In each ward, we chose a random number, after which every third bed was approached to assess whether the patient in it met the inclusion criteria, i.e. (i) age >18 years, (ii) admitted for at least 24 hours, (iii) physically fit to participate in the study, and (iv) willing to participate in the study by providing written consent. If the selected bed was empty or the patient did not meet the inclusion criteria, we approached the patient on the next selected bed. We continued to choose every third bed in this manner, till the required sample size was covered. We excluded ICU beds, as well as beds in the Paediatrics and Psychiatry ward. The ICU beds were excluded as the patient would not have been able to participate in the study comfortably. We excluded beds in the paediatric ward, since the study was limited to adults. We also excluded beds in the psychiatry ward since the focus was to assess the rates of substance use and SUD in patients with medical illnesses.
Instruments
A semi-structured questionnaire was developed to collect information about socio-demographics, medical diagnosis for which the participant was admitted and details of substance use. Questions about substance use included lifetime and current use of any psychoactive substance, type of substance used, age of onset of the substance use, predominant route of use, diagnosis of SUD (as per ICD-10), abstinence attempts and treatment received in the past. Regarding alcohol use, information on the type of alcohol consumed, lifetime morning drinking, lifetime daily drinking, driving under influence, heavy episodic drinking (defined as taking equal to or more than 6 standard drinks in an episode) was also collected. The treatment details included nature of treatment taken for substance use and number of occasions on which treatment had been taken.
We also had questions about the participant’s opinion on whether the substance use could have contributed to the current medical illness for which they were admitted, whether their substance use could modify the course or outcome of their current medical illness, whether they had informed their medical treatment team about their substance use, and whether they had received help for stopping their substance use.
The medical diagnosis was noted from the medical sheet maintained by the team treating the participant’s medical illness. The interviewer recorded the particular chapter of the 10th Revision of International Classification of Diseases (ICD-10) that included the participant’s medical diagnosis; the ICD-10 classifies medical conditions in 22 different chapters, such as chapter I titled ‘certain infections and parasitic diseases’, chapter II titled ‘neoplasms’, and so on.
Alcohol, Smoking and Substance Involvement Screening Test (ASSIST)–Hindi version was used to assess severity of alcohol use.23 Fagerström tests for Nicotine dependence for smoking (FTND) and for smokeless tobacco (FTND-ST) were used to assess the severity of nicotine dependence among current tobacco users.24–26
Study procedure
One of four psychiatrists, who had been trained on the study methodology and the data collection tools, interviewed each participant. The interviews were done from August 2019 till October 2019, in the respective wards ensuring privacy and after obtaining a written informed consent, and lasted around 30 minutes each. The data were collected and managed using REDCap electronic data capture tools.27
We obtained approval from the Ethics Committee of our institution before beginning the data collection.
Data analysis
Statistical Package for the Social Sciences (SPSS) version 21.0 (IBM Corp 2012, Armonk, NY, USA) was used for data analysis. We summarized the categorical data as frequencies and percentages, and the continuous data as mean (standard deviation, SD) or median (inter-quartile range, IQR). For ICD-10 chapters, illnesses which were present in at least 10% of the study participants at the time of interview, relationship with ever substance use, current substance use, ever tobacco use, ever alcohol use, current tobacco use and current alcohol use, were studied using chi-squared test.
RESULTS
Of the 322 patients approached, 32 were excluded (Fig. 1) and a total of 290 subjects were included in the study.
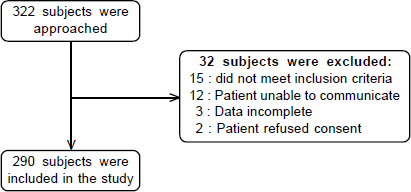
- Flow-chart depicting the inclusion of participants in the study
Sociodemographic details
The mean (SD) age of the participants was 42.2 (15.6) years. Most participants were men (170, 58.6%), married (222, 76.6%) and residing in urban areas (188, 64.8%; Table I). Most participants were unemployed (172, 59.3%).
| Item | Response | n (%) |
|---|---|---|
| Gender | Men | 170 (58.6) |
| Women | 120 (41.4) | |
| Marital status | Married | 222 (76.6) |
| Never married | 5 3 (18.3) | |
| Widow(er)/separated | 1 5 (5.1) | |
| Highest educational attainment | Professional | 4 (1.4) |
| Postgraduate | 2 8 (9.7) | |
| Graduate | 5 1 (17.6) | |
| Up to class 12 | 5 2 (17.9) | |
| Up to class 10 | 6 0 (20.7) | |
| Up to class 5 | 4 2 (14.5) | |
| Primary | 2 8 (9.7) | |
| Illiterate | 2 5 (8.6) | |
| Occupation | Highly skilled | 3 8 (13.1) |
| Skilled | 8 8 (30.3) | |
| Semi-skilled | 7 4 (25.5) | |
| Unskilled | 8 5 (29.3) | |
| Missing data | 5 (1.7) | |
| Employment status | Full time employed | 7 7 (26.6) |
| Part time employed | 1 5 (5.2) | |
| Unemployed | 172 (59.3) | |
| Not known | 2 5 (8.6) | |
| Missing | 1 (0.3) | |
| Residence | Rural | 102 (35.2) |
| Urban | 181 (62.4) | |
| Urban (Slum) | 7 (2.4) |
Details of medical illnesses
The median duration of any medical illness among the participants was 12 months (IQR: 6, 72) and the median duration of the primary medical illness for which the participant was admitted was 12 months (IQR: 3, 48). Two hundred and three (70%) participants had one medical illness, 51 (17.6%) had two medical illnesses, and the rest (36, 12.4%) had more than two illnesses. Table II provides the distribution of medical illnesses by chapters of ICD-10, with illnesses of the circulatory system (103, 35.3%) being the most common, followed by neoplasms (67, 23.1%).
| ICD-10 chapter | n (%)* | Predominant diagnosis for which admitted (only one diagnosis) (%) |
|---|---|---|
| Missing | 1 (0.3) | 1 (0.3) |
| Certain infectious and parasitic diseases | 1 3 (4.5) | 5 (1.7) |
| Neoplasms | 6 7 (23.1) | 6 2 (21.4) |
| Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism | 3 (1.0) | – |
| Endocrine, nutritional and metabolic diseases | 3 3 (11.4) | 9 (3.1) |
| Diseases of the nervous system | 1 0 (3.4) | 7 (2.4) |
| Diseases of the eye and adnexa | 1 1 (3.8) | – |
| Diseases of the ear and mastoid process | 1 (0.3) | 1 (0.3) |
| Diseases of the circulatory system | 103 (35.5) | 6 9 (23.8) |
| Diseases of the respiratory system | 8 (2.8) | 6 (2.1) |
| Diseases of the digestive system | 2 5 (8.6) | 2 0 (6.9) |
| Diseases of the skin and subcutaneous tissue | 7 (2.4) | 7 (2.4) |
| Diseases of the musculoskeletal system and connective tissue | 2 0 (6.9) | 1 7 (5.9) |
| Diseases of the genitourinary system | 2 5 (8.6) | 2 2 (7.6) |
| Pregnancy, childbirth and the puerperium | 2 (0.7) | 1 (0.3) |
| Certain conditions originating in the perinatal period | 1 (0.3) | 1 (0.3) |
| Congenital malformations, deformations and chromosomal abnormalities | 6 (2.1) | 2 (0.7) |
| Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified | 9 (3.1) | 8 (2.8) |
| Injury, poisoning and certain other consequences of external causes | 4 3 (14.8) | 4 3 (14.8) |
| External causes of morbidity and mortality | 1 (0.3) | – |
| Factors influencing health status and contact with health services | 9 (3.1) | 9 (3.1) |
Details of substance use
One hundred and nine (37.6%) participants reported having used at least one psychoactive substance at some time during their lifetime. The most common substance ever used was tobacco (91, 31.4%), followed by alcohol (69, 23.8%), cannabis (12, 4.1%) and sedatives (2, 0.7%); 56 (19.3%) participants reported having used more than one psychoactive substance in their lifetime (Table III). None of the participants reported the use of other psychoactive substances (cocaine, amphetamines, hallucinogens, inhalants or opioids) in their lifetime. None of the participants reported having used any psychoactive substance by the injectable route.
| Item | Tobacco (n=91) | Alcohol (n=69) | Cannabis (n=12) | Sedatives (n=2) |
|---|---|---|---|---|
| Mean (SD) age at onset, years | 19.42 (5.8) | 22.8 (6.4) | 21.4 (7.2) | 30 (4.2) |
| Median (IQR) duration of use, years | 28 (18, 38) | 22 (10, 34) | 23 (16, 35) | 11 (0, –) |
| Predominant substance/route of use n (%) | Smoke:51 (56) Smokeless: 40 (44) |
IMFL:31 (44.9) Beer:23 (33.3) Indian: 11 (15.9) Others: 4 (5.8) |
Bhang: 7 (58.3) Charas: 2 (16.7) Ganja:3 (25) Smoking: 5 (41.7) Oral:7 (58.3) |
– |
| Dependence syndrome (of 290) | 76 (26.2) | 15 (5.2) | 0 | 0 |
| Harmful use (of 290) | 3 (1.0) | 8 (2.8) | 1 (0.3) | 0 |
| ASSIST risk severity | ||||
| Low | 10 (11) | 6 (8.7) | 0 | 0 |
| Moderate | 53 (58.2) | 5 (7.2) | 2 (16.7) | 1 (50) |
| High | 23 (25.3) | 50 (72.5) | 10 (83.3) | 1 (50) |
| Missing data | 5 (5.5) | 8 (11.6) | 0 | 0 |
Figures in parentheses are percentages unless specified IMFL Indian made foreign liquor
Forty-nine (16.9%) participants reported current (at least once in the past three months) use of any psychoactive substance, including 47 (16.2%) of tobacco, 21 (7.2%) of alcohol, 3 (1.0%) of cannabis, and 1 (0.3%) of a sedative.
Tobacco use
Twenty-six per cent participants (n=76) fulfilled the criteria of dependence syndrome, while 3 participants fulfilled the criteria for tobacco harmful use (Table III). Among the 47 current tobacco users, nearly half (23, 49%) used tobacco only in smoking form, 19 (40.4%) only in smokeless form, and 5 (10.6%) in smoking as well as in smokeless forms. The median FTND score for smokers was 6 (IQR: 2, 7) and the median FTND–ST score for smokeless tobacco was 5 (IQR: 3, 7), with the median overall FTND score being 6 (IQR: 3, 7).
Alcohol use
Among 69 ever alcohol users, 14 (20.3%) reported having taken alcohol during daytime, and 8 (11.6%) to have consumed alcohol in morning hours; further, 21 (30.4%) reported heavy episodic drinking episodes, and 9 (13.0%) reported history of driving vehicle under alcohol intoxication. Fourteen (20.3%) of the alcohol users had history of episodes of alcohol withdrawal, and 10 (14.5%) reported physical complications due to alcohol use. Of the 290 participants, 15 (5.2%) met the criteria for lifetime diagnosis of alcohol dependence syndrome, and 8 (2.8%) of harmful use of alcohol.
Abstinence and treatment attempts
Among 109 patients reporting use of any psychoactive substance ever in their lifetime, 42 (38.5%) had made one or more major attempt at cessation, with the median number of such attempts being one (IQR: 1, 4.3). Only one participant, who had both current alcohol dependence and current nicotine dependence, reported having received formal treatment previously for substance withdrawal and for long-term management of substance use.
Participants and interviewers’ opinion about role of substance use in medical illness
One-third (37, 33.9%) of the 109 participants with lifetime psychoactive substance use believed that their substance use could have contributed to the occurrence of their medical illness. This proportion for those with current psychoactive substance use was 19 of 49 (38.8%). Nearly half of the participants with lifetime substance (55 of 109, 50.5%) or of those with current substance use (27 of 49; 55.1%) believed that their substance use (or non-use) could modify the course or outcome of their medical illness. Of the participants with lifetime substance use, 60 (55%) had reduced or discontinued substance use after the onset of their medical illness (26 [53.1%] of those with current psychoactive substance use). About two-third of participants (73, 67%) with lifetime substance use had informed their treating team about their substance use; the proportion was similar for those with current substance use (33, 67.3%). Nearly half the participants (59, 54.1%) with lifetime substance use had received information about the risks of substance use (49%, 29 of those with current substance use). However, only a few (8, 7.3%) had been offered treatment for SUDs by the treating team (including 3 of those with current substance use).
The interviewers were also asked to opine on the role of the participant’s substance use in their medical illness. The interviewers felt that substance use may have caused or have adversely influenced the risk of occurrence of medical illness in 52 (47.7%) participants with lifetime psychoactive substance use, and 25 (51%) of those with current substance use. The interviewers also felt that substance use could worsen the course or outcome of the medical illness in 88 (80.7%) participants with substance use (and 42 [85.7%] of those with current substance use). The interviewers also felt that the participants’ medical illness could complicate the treatment of substance use in 33 (30.3%) participants with lifetime substance use and 17 (34.7%) of those with current substance use.
Association between substance use and other variables
Table IV shows the association between substance use and other variables. The substance use variables considered in the bivariate analysis were lifetime and current tobacco use, lifetime and current alcohol use, and lifetime and current any substance use. Men, those with lower education attainment and those who were married had significantly higher proportion of lifetime and current use of tobacco, alcohol and any substance. Those with lifetime alcohol use were more likely to have diseases of the circulatory system. Similarly, lifetime alcohol use, lifetime use of any psychoactive substance, current tobacco use and current use of any psychoactive substance use more often had illness classified in the chapter on ‘injuries, poisoning and other consequences of external causes’ in the ICD-10.
| Variable | Category | Lifetime use | Current use | ||||
|---|---|---|---|---|---|---|---|
| Tobacco (n=91) | Alcohol (n=69) | Any substance (n=109) | Tobacco (n=47) | Alcohol (n=22) | Any substance (n=49) | ||
| Gender | Men | 81 (89) | 67 (97.1) | 98 (89.9) | 43 (91.5) | 20 (90.9) | 43 (87.8) |
| Women | 10 (11) | 2 (2.9) | 11 (10.1) | 4 (8.5) | 2 (9.1) | 6 (12.2) | |
| p value | <0.01* | <0.01* | <0.01* | <0.01* | <0.01* | <0.01* | |
| Marital status | Married | 83 (91.2) | 61 (88.4) | 98 (89.9) | 43 (91.5) | 18 (81.8) | 45 (91.8) |
| Others | 8 (8.8) | 8 (11.6) | 11 (10.1) | 4 (8.5) | 4 (18.2) | 4 (8.2) | |
| p value | <0.01* | <0.01* | <0.01* | <0.01* | 0.54 | <0.01* | |
| Educational attainment | Up to class 10 | 61 (67.0) | 40 (58.0) | 70 (64.2) | 32 (68.1) | 11 (50.0) | 33 (67.3) |
| More than class 10 | 30 (33.0) | 29 (42.0) | 39 (35.8) | 15 (31.9) | 11 (50.0) | 16 (32.7) | |
| p value | <0.01* | 0.39 | <0.01* | <0.05* | 0.74 | <0.05* | |
| Employment status | Employed | 33 (36.3) | 31 (44.9) | 41 (37.6) | 21 (44.7) | 9 (40.9) | 21 (42.9) |
| Unemployed | 58 (63.7) | 38 (55.1) | 68 (62.4) | 26 (55.3) | 13 (59.1) | 28 (57.1) | |
| p value | 0.26 | <0.05* | 0.09 | <0.05* | 0.34 | 0.07 | |
| Diseases of circulatory system (n=103) | Yes | 34 (37.4) | 32 (46.4) | 42 (38.5) | 13 (27.7) | 8 (36.4) | 15 (30.6) |
| No | 57 (62.6) | 37 (53.6) | 67 (61.5) | 34 (72.3) | 14 (63.6) | 34 (69.4) | |
| p value | 0.65 | 0.03* | 0.40 | 0.22 | 0.93 | 0.43 | |
| Neoplasms (n=67) | Yes | 25(27.5) | 12 (17.4) | 27 (24.8) | 11 (23.4) | 3 (13.6) | 12 (24.5) |
| No | 66 (72.5) | 57 (82.6) | 82 (75.2) | 36 (76.6) | 19 (86.4) | 37 (75.5) | |
| p value | (0.23) | 0.20 | 0.60 | 0.96 | 0.27 | 0.80 | |
| Endocrine, nutritional and metabolic disorders (n=33) | Yes | 13 (14.3) | 9 (13.0) | 15 (13.8) | 5 (10.6) | 3 (13.6) | 6 (12.2) |
| No | 78 (85.7) | 60 (87.0) | 94 (86.2) | 42 (89.4) | 19 (86.4) | 43 (87.8) | |
| p value | 0.29 | 0.62 | 0.32 | 0.86 | 0.73 | 0.83 | |
| Injury, poisoning and certain other consequences of external | Yes | 17 (18.7) | 16 (23.2) | 22 (20.2) | 12 (25.5) | 6 (27.3) | 12 (24.5) |
| No | 74 (81.3) | 53 (76.8) | 87 (79.8) | 35 (74.5) | 16 (72.7) | 37 (75.5) | |
| p value | 0.21 | 0.02* | 0.04* | 0.02* | 0.08 | 0.03* | |
DISCUSSION
We assessed the prevalence of use of all psychoactive substances in a tertiary care, multi-disciplinary hospital in India. We used systematic sampling to select participants to reduce selection bias. We included adult patients from all clinical disciplines in the hospital, except for those admitted in ICUs and the psychiatry ward. Psychiatrists interviewed the selected participants which helped in making a diagnosis of SUDs and in assessing whether the participants’ substance use and medical illness could affect each other.
A sizeable proportion of hospital admissions in our study had substance use, as has been documented in other studies as well.9,11,12 We found that almost one-third of the participants had used at least one psychoactive substance in their lifetime. Almost 1 in 5 participants reported using any psychoactive substance currently. As is the case with the general population in India, the prevalence of tobacco use was the highest followed by the use of alcohol and cannabis.13 The prevalence of tobacco use disorder and of alcohol use disorders in our study (of 27% and 8%, respectively) was higher than that in a general population survey in the country, i.e. the National Mental Health Survey (NMHS) of India (21% and 4.6%, respectively). Prevalence of SUD in patients admitted to hospital is often higher than that in the general population.29,30 The rates of tobacco use disorder and alcohol use disorder in our participants was similar to that seen in other studies among general medical inpatients.20,29,31–33 Thus, our study shows that it is important to screen all patients admitted to a hospital for the presence of lifetime and current use of any psychoactive substance, especially tobacco and alcohol, and SUD. In case of current use, screening instruments such as ASSIST should be used to assess the risk category of substance use for appropriate clinical decision making.
In keeping with the data from the previous general population surveys, none of our participants reported lifetime use of cocaine, amphetamines or hallucinogens.13 An interesting finding was that none of our participants reported opioid use, which was reported by 2.1% of the general population aged 10–75 years in a recent national survey,13 and a sizeable proportion of patients admitted to hospital in previous studies.34,35 Some studies, in fact, have linked higher prevalence of opioid admissions in recent years with the surge in opioid use in the community.36,37 Some other studies from India also show lower prevalence of opioid use among patients admitted to hospital with a medical illness.38,39 Studies from India have shown physical problems with opioid injecting drug use, including blocked veins, abscess and overdose episodes.40,41 Yet, opioid users are not reflected in medical admissions to hospital. Further studies are required to explore reasons for the poor utilization of hospital services by opioid users, including whether they feel discriminated against in hospitals.42,43 Presence of SUDs was strongly associated with male gender and lower education in our study. Additionally, alcohol use was also associated with injuries and diseases of the circulatory system. Unfortunately, other medical illnesses were less prevalent in our study; hence, their association with substance use could not be assessed.
Medical illness can serve as a strong motivating factor for individuals with SUDs to quit their substance use.44–46 Almost 55% participants in our study with lifetime substance use tried to reduce or stop their substance use by themselves after the onset of their medical illness. Though two-thirds of the participants had informed their treating team about their lifetime substance use, only half were informed about the risk of substance use on their medical illness. It may be possible that the medical team would not have assessed for presence of substance use in their patients as seen in other studies as well.35,47 The benefit of SUD interventions in hospitals on the course of SUD as well as in management of medical illness is well documented.6,48 The data shows that an important opportunity to counsel patients using substances is missed by the primary clinician in-charge of the medical illness. Unfortunately, many clinicians are not well versed with the diagnosis and management of SUD as the medical curriculum does not cover this topic adequately. There is a need to provide adequate training on diagnosis and management of SUD during medical training.
Despite a sizeable number of participants suffering from and reporting substance use, a minor proportion of participants with substance use were offered treatment for their substance use in our study.
Various models exist for providing psychiatry (including addiction) services in medical/surgical settings. On one end of the spectrum is the demand-driven approach such as consultation model where the primary physician detects problematic substance use in their patients and sends referrals to the hospital psychiatrist.49 At the other end exist Addict Consult Services (ACS), where a multi-disciplinary team of mental health professionals work with physicians to provide hospital care for patients with SUD.50 Studies show that ACS works much better than other consultation–liaison addiction treatment models; however, ACS is resource intensive and it may not be feasible and viable to implement ACS in India.51 The best approach for hospitals in India would be to educate the non-psychiatry medical doctors on identification and initial management of patients with SUD. Studies show that approaches such as Screening, Brief Interventions and Referral to Treatment (SBIRT) are helpful in identifying at-risk substance users and linking them to appropriate treatment for SUD.52 Such approaches can be delivered in 5–10 minutes in various medical settings ranging from primary care to emergency departments.53 Research has shown the effectiveness of brief interventions (BI) in problem substance users, especially alcohol use, delivered even by non-specialists.54–56 Unfortunately, most studies on approaches such as SBIRT are from western countries. The effectiveness of such approaches in hospital settings have not been studied in India, though the effectiveness of BI in the Indian population has been well documented.57–59
Our study has some limitations. While the sample size was enough for estimating the prevalence of SUD for all the substances combined, it was insufficient for individual substances, except tobacco. We did not include patients who were admitted for less than 24 hours, those admitted in ICU or those presenting to the emergency department, which may have affected the estimate of SUD in our study.
Conclusions
Patients admitted in hospitals have substantial prevalence of substance use and SUDs. Tobacco is the most used substance followed by alcohol use. Despite this, fewer patients receive treatment for SUD. There is a need to develop models to address substance use in patients admitted for a medical illness.
References
- Hospital length of stay variation and comorbidity of mental illness: A retrospective study of five common chronic medical conditions. BMC Health Serv Res. 2018;18:498.
- [CrossRef] [Google Scholar]
- Alcohol use and anti-retroviral adherence: Review and meta-analysis. J Acquir Immune Defic Syndr. 2009;52:180-202.
- [CrossRef] [Google Scholar]
- Alcohol consumption as a risk factor for tuberculosis: Meta-analyses and burden of disease. Eur Respir J. 2017;50:1700216.
- [CrossRef] [Google Scholar]
- Alcohol toxicity in diabetes and its complications: A double trouble? Alcohol Clin Exp Res. 2016;40:686-97.
- [CrossRef] [Google Scholar]
- Acute care hospital utilization among medical inpatients discharged with a substance use disorder diagnosis. J Addict Med. 2012;6:50-6.
- [CrossRef] [Google Scholar]
- An inpatient treatment and discharge planning protocol for alcohol dependence: efficacy in reducing 30-day readmissions and emergency department visits. J Gen Intern Med. 2015;30:365-70.
- [CrossRef] [Google Scholar]
- Managing acutely ill substance-abusing patients in an integrated day hospital outpatient program: Medical therapies, complications, and overall treatment outcomes. J Gen Intern Med. 2006;21:570-6.
- [CrossRef] [Google Scholar]
- Alcohol dependence among patients admitted to psychiatric emergency services. Gen Hosp Psychiatry. 2000;22:206-12.
- [CrossRef] [Google Scholar]
- Prevalence of alcohol related attendance at an inner city emergency department and its impact: A dual prospective and retrospective cohort study. Emerg Med J. 2016;33:187-93.
- [CrossRef] [Google Scholar]
- Violence and substance use among an injured emergency department population. Acad Emerg Med. 2003;10:764-75.
- [CrossRef] [Google Scholar]
- The prevalence of wholly attributable alcohol conditions in the United Kingdom hospital system: A systematic review, metaanalysis and metaregression. Addiction. 2019;114:1726-37.
- [CrossRef] [Google Scholar]
- From data to evidence, to action: Findings from a systematic review of hospital screening studies for high risk alcohol consumption. Drug Alcohol Depend. 2006;83:1-14.
- [CrossRef] [Google Scholar]
- Magnitude of substance use in India. Ministry of Social Justice and Empowerment Government of India;. 2019 Available at http://socialjustice.nic.in/writereaddata/UploadFile/Magnitude_Substance_Use_India_REPORT.pdf (accessed on 10 Jan 2022).
- [Google Scholar]
- Sociodemographic profile and psychiatric diagnosis of patients referred to consultation–liaison psychiatric services of general hospital psychiatric unit at a tertiary care center. J Ment Health Hum Behav. 22:45.
- [CrossRef] [Google Scholar]
- Pattern of psychiatric referrals in a tertiary care teaching hospital in southern India. J Clin Diagn Res. 2013;7:1689-91.
- [Google Scholar]
- Alcohol problems in a general hospital––a prevalence study. J Indian Med Assoc. 1997;95:505-6.
- [Google Scholar]
- Trends of tobacco consumption among women admitted to and visiting the psychiatric inpatient unit of a tertiary care center in Mumbai: A cross-sectional study. Prim Care Companion CNS Disord. 2019;21 18m02422
- [CrossRef] [Google Scholar]
- Tobacco use and subsequent cessation among hospitalized patients in Mumbai, India: A longitudinal study. Nicotine Tob Res. 2019;22:363-70.
- [CrossRef] [Google Scholar]
- Alcohol use and alcohol use disorder among male outpatients in a primary care setting in rural Puducherry. Ind Psychiatry J. 2015;24:135-9.
- [CrossRef] [Google Scholar]
- Tobacco use prevalence and smoking cessation pharmacotherapy prescription patterns among hospitalized patients by medical specialty. Nicotine Tob Res. 2019;21:631-7.
- [CrossRef] [Google Scholar]
- Premalignant and malignant lesions of oral cavity in eastern India: A hospital-based study. Eur J Cancer Prev. 2021;30:393-9.
- [CrossRef] [Google Scholar]
- The young myocardial infarction study of the western Indians: YOUTH registry. Glob Heart. 2019;14:27-33.
- [CrossRef] [Google Scholar]
- WHOQOL-Hindi: A questionnaire for assessing quality of life in health care settings in India. World Health Organization Quality of Life. Natl Med J India. 1998;11:160-5.
- [Google Scholar]
- Psychometric properties of the Fagerström test for nicotine dependence. J Bras Pneumol. 2009;35:73-82.
- [CrossRef] [Google Scholar]
- The Fagerström test for nicotine dependence: A revision of the Fagerström tolerance questionnaire. Br J Addict. 1991;86:1119-27.
- [CrossRef] [Google Scholar]
- The Fagerström test for nicotine dependence-smokeless tobacco (FTND-ST) Addict Behav. 2006;31:1716-21.
- [CrossRef] [Google Scholar]
- Research electronic data capture (REDCap)––a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377-81.
- [CrossRef] [Google Scholar]
- National Mental Health Survey of India, 2015-16 Summary. Bengaluru:National Institute of Mental Health and Neuro Sciences; 2016
- [Google Scholar]
- The prevalence and detection of substance use disorders among inpatients ages 18 to 49: An opportunity for prevention. Prev Med. 1998;27:101-10.
- [CrossRef] [Google Scholar]
- Assessment of alcohol use disorder and its associated factors among alcohol users of medical and surgical outpatients attending a specialized hospital in Gondar, Ethiopia: A cross-sectional study. Int J Ment Health Syst. 2021;15:28.
- [CrossRef] [Google Scholar]
- Alcohol abuse: Prevalence and detection in a general hospital. J R Soc Med. 2002;95:84-7.
- [CrossRef] [Google Scholar]
- The severity of unhealthy alcohol use in hospitalized medical patients. The spectrum is narrow. J Gen Intern Med. 2006;21:381-5.
- [CrossRef] [Google Scholar]
- Detection of alcohol use disorders in general hospital admissions in the United States. Arch Intern Med. 2004;164:749-56.
- [CrossRef] [Google Scholar]
- Substance use disorder detection rates among providers of general medical inpatients. J Gen Intern Med. 2021;36:668-75.
- [CrossRef] [Google Scholar]
- Addiction consultation services––Linking hospitalized patients to outpatient addiction treatment. J Subst Abuse Treat. 2017;79:1-5.
- [CrossRef] [Google Scholar]
- Hospital inpatient utilization related to opioid overuse among adults, 1993–2012 Agency for Healthcare Research and Quality; 2014. Available at www.hcup-us.ahrq.gov/reports/statbriefs/sb177-Hospitalizations-for-Opioid-Overuse.jsp (accessed on 10 Jan 2022).
- [Google Scholar]
- Increasing infectious endocarditis admissions among young people who inject drugs. Open Forum Infect Dis. 3 ofw157
- [CrossRef] [Google Scholar]
- Substance use among outdoor treatment-seeking patients with mental illness: A case–control study from a tertiary care hospital of northern India. J Educ Health Promot. 2018;7:75.
- [CrossRef] [Google Scholar]
- A profile of substance abusers using the emergency services in a tertiary care hospital in Sikkim. Indian J Psychiatry. 2006;48:243-7.
- [CrossRef] [Google Scholar]
- Rates, knowledge and risk factors of non-fatal opioid overdose among people who inject drugs in India: A community-based study. Drug Alcohol Rev. 2019;39:93-7.
- [CrossRef] [Google Scholar]
- Type of opioids injected: Does it matter? A multicentric cross-sectional study of people who inject drugs. Drug Alcohol Rev. 2015;34:97-104.
- [CrossRef] [Google Scholar]
- “Maybe if I stop the drugs, then maybe they’d care?”—hospital care experiences of people who use drugs. Harm Reduct J. 16:16.
- [CrossRef] [Google Scholar]
- The stigmatization of problem drug users: A narrative literature review. Drugs Educ Prev Policy. 2013;20:85-95.
- [CrossRef] [Google Scholar]
- Motivation to change and factors influencing motivation in alcohol dependence syndrome in a tertiary care hospital. Indian J Psychiatry. 2017;59:183-8.
- [CrossRef] [Google Scholar]
- Injury as a motivator to reduce drinking. Acad Emerg Med. 1995;2:817-25.
- [CrossRef] [Google Scholar]
- Motivation to change risky drinking and motivation to seek help for alcohol risk drinking among general hospital inpatients with problem drinking and alcohol-related diseases. Gen Hosp Psychiatry. 2010;32:86-93.
- [CrossRef] [Google Scholar]
- Attitudes, practices, and preparedness to care for patients with substance use disorder: Results from a survey of general internists. Subst Abus. 2016;37:635-41.
- [CrossRef] [Google Scholar]
- Buprenorphine treatment for hospitalized, opioid-dependent patients: A randomized clinical trial. JAMA Intern Med. 2014;174:1369-76.
- [CrossRef] [Google Scholar]
- Consultation–liaison psychiatry in India: Where to go from here? Indian J Psychiatry. 2019;61:117-24.
- [CrossRef] [Google Scholar]
- Inpatient addiction consult service: Expertise for hospitalized patients with complex addiction problems. Med Clin North Am. 2018;102:587-601.
- [CrossRef] [Google Scholar]
- A taxonomy of hospital-based addiction care models: A scoping review and key informant interviews. J Gen Intern Med. 2022;37:2821-33.
- [CrossRef] [Google Scholar]
- Screening, brief intervention, and referral to treatment (SBIRT): Toward a public health approach to the management of substance abuse. Subst Abus. 2007;28:7-30.
- [CrossRef] [Google Scholar]
- The impact of screening, brief intervention and referral for treatment in emergency department patients’ alcohol use: A 3-, 6-and 12-month follow-up. Alcohol Alcohol. 2010;45:514-19.
- [CrossRef] [Google Scholar]
- Screening, brief intervention and referral to treatment: Implications of SAMHSA’s SBIRT initiative for substance abuse policy and practice. Addiction. 2017;112(Suppl 2):110-17.
- [CrossRef] [Google Scholar]
- Sustaining screening, brief intervention and referral to treatment (SBIRT) services in health-care settings. Addiction. 2017;112(Suppl 2):92-100.
- [CrossRef] [Google Scholar]
- Implementing SBIRT (screening, brief intervention and referral to treatment) in primary care: Lessons learned from a multi-practice evaluation portfolio. Public Health Rev. 2017;38:31.
- [CrossRef] [Google Scholar]
- Brief interventions for harmful alcohol use in opioid-dependent patients on maintenance treatment with buprenorphine: A prospective study from India. Addict Disord Their Treat. 2016;15:129-35.
- [CrossRef] [Google Scholar]
- The systematic development of a mobile phone-delivered brief intervention for hazardous drinking in India. J Subst Abuse Treat. 126:108331.
- [CrossRef] [Google Scholar]
- A comparison of brief intervention versus simple advice for alcohol use disorders in a North India community-based sample followed for 3 months. Alcohol Alcohol. 2007;42:328-32.
- [CrossRef] [Google Scholar]




