Translate this page into:
Public health-oriented healthcare systems: Need for a modified typology
Corresponding Author:
Mathew George
Centre for Public Health, School of Health Systems Studies, Tata Institute of Social Sciences, Mumbai, Maharashtra
India
mathewg@tiss.edu
| How to cite this article: George M. Public health-oriented healthcare systems: Need for a modified typology. Natl Med J India 2019;32:171-174 |
Abstract
Healthcare systems across the world are dominated by medical care services compared to public health services. Within public health services, individual-oriented interventions dominate compared to population-based interventions perhaps due to the inherent dominance of biomedical approaches within public health. Clarity is needed between diverse approaches, methods and targets of public health as against clinical care services delivered under healthcare systems. Public health has a primary objective of prevention and promotion with the population as the target group with a societal focus, whereas the latter is curative in intent with an individualist orientation and logic and hence reductionist. The implications are important for developing nations such as India, which have a history of neglect towards ensuring public health due to the domination of policies on medical care. The healthcare system should use a modified typology that asserts its differential commitment to address both public health and medical care needs of its citizens.
Introduction
Of the various concepts of healthcare systems*, the oldest and the most widely used is that of Roemer’s[1] owing to the field of political science, where the role of state and its authority is the major focus. In this typology, the major focus has been to categorize healthcare systems based on the extent of autonomy government possesses, which ranges from the free enterprise system with minimal autonomy and responsibility with the government to the socialist system with the entire responsibility of provisioning of health services entrusted within the government. Healthcare systems are organized across nations immediately after their formation by focusing on the provisioning of medical care for citizens. This largely depends on the nature of the political system prevalent and the priority each country gives to health in relation to other concerns.[2] ‘Health service system’ and ‘healthcare system’ are terms used interchangeably to denote how a nationstate organizes its commitment and resources to deliver a range of curative and disease control measures to its citizens. The deliberations on preventive and curative services provided by each healthcare system are largely about whether they are provided in a comprehensive manner or in isolation. What is missing in this typology is whether the healthcare systems of countries have adequate public health and medical care services or are dominated by either. From a value-based framework for low- and middle- income countries (LMICs), good health systems ‘are those whose primary purpose is improving health but which may do this both through the delivery of services but also through action which impinges on other sectors that may influence health positively or negatively’.[3]
India’s Policy Context
To appreciate the extent of public health and medical care services to be delivered, clarity is required about the approaches, methods and targets along with the boundaries of the two related but distinct disciplines. This can also help in interpreting the nature of professional expertise needed for these distinct functions. This is all the more relevant at a time when the need for a ‘public health cadre’ has been recommended by the National Health Policy 2017 of India despite interchangeably using ‘public health system’ and ‘healthcare system’ to denote India’s healthcare system.[5] The implications of this distinction are important in India which neglected[6],[7] public health in its healthcare policies; these were always dominated by concerns related to the provisioning of medical care.
Engaging With the Concept of Health Systems
The concept of health systems across nations have evolved historically and are defined as all those activities whose primary purpose is to promote, restore or maintain health. Despite this, the concept of health systems is not perceived uniformly across nations. The WHO report on health systems states: ‘Beyond the boundaries of this definition are those activities whose primary purpose is something other than health—education, for example— even if these activities have a secondary, health-enhancing benefits… is outside the boundaries.‘[4] Further, the report goes on to give reasons for arriving at a narrower definition of the health system for operational purposes.
Unfortunately, nearly all the information available about health systems refers only to the provision of, and investment in, health services: that is, the healthcare system, including preventive, curative and palliative interventions, whether directed to individuals or to populations.[4]
Thus, the concept has transformed from a broader definition that included all activities that result in the promotion of health to those that are only part of a nation’s healthcare system. Another concept of health system originates from the concept of social systems where health systems are one of the subsystems of society:[8]
Health system as that aggregate of commitments and resources (human, cultural, political and material) any society devotes to, or sets aside for, or invests into the ‘health’ concern as distinguished from other concerns such as general education, defence, industrial production, communications and so on.
The advantage of the above definition is that it is situated within a societal context and hence is dynamic. It helps to judge the priority any society attributes to health systems as opposed to other subsystems within the society as this priority itself is dependent on the level of development every society enjoys. The complex societal context acknowledges multiple determinants and its engagement with population health of which healthcare systems is treated as only one. A brief review of the principles and approaches of medicine and public health will help to re-imagine a modified typology that examines public health orientation of healthcare systems across nations.
Discursive Practice of Medicine
The intimate engagement between knowing and doing actualized through the practice of medicine defines the unique character of medicine itself. An enquiry into the philosophy and principles of medical profession reveal its core function and therefore its mandate. According to the philosophers[9] of medicine,
Medicine is the cognitive art of applying science and persuasion through a complex human interaction in which the uniqueness of values and disease, and the kind of institution in which care is delivered, determine the nature of the judgements made.
This explanation situates clinical interaction as the core activity of medicine and the restoration of well-being as its goal. The centrality of clinical interaction allows medicine to take up several forms, namely, as a discipline as well as a profession. As other professions, medicine shares the dual requirements of sufficient skill and commitment to human purpose.[10] The skill calls for a theoretical knowledge of the sciences and a creative handling of symbols such as disease and experience in applying both to individuals in need. The central purpose of medicine as that of healing the sick needs to be acknowledged wherein individual characteristics such as signs, symptoms and other indications of the patient along with the central role of clinical interaction become primordial. The individualist focus, inherent in medical care is a unique feature that facilitates most of its core characteristics as a healing profession, namely diagnosis, prognosis and treatment. This uniqueness of the nature of medicine is what philosophers of medicine qualify as tekne iatrike, which is explained as a technique of healing. Tekne means knowledge of how to act according to what is the case and why it is the case.[9] Medical care services are ways of organizing those curative and rehabilitative services, following the principle of medicine, for its citizens with a view to alleviate their suffering due to diseases. Medical care services thus organized as part of healthcare systems have to follow the principle of equity as a commitment to social justice that no individual should be denied care because of their social position within society.
Contextualizing Public Health Practice
Public health, a practising profession, is emerging as an academic discipline with prevention, population and social justice as its core principles that use interdisciplinary approaches. The approaches of public health always depend on the kind of epidemiology that is used to interpret population health. The relationship between epidemiology and public health is well articulated by making clear demarcation between their roles,[11] as epidemiology is the scientific study leading to knowledge about the distribution and determinants of diseases in a population with public health as the application of this knowledge to improve population health. Epidemiology was historically an important tool for public health practice whose focus was primarily on population, which after having traversed several eras has acquired scientific status in modern times. In the process, modern epidemiology has predominantly become individualistic in its orientation thereby losing its relevance in contemporary public health practice.[12],[13] One of the ways by which contemporary epidemiology is made relevant to public health practice is by applying social theories in epidemiological enquiry by interrogating the macrosocial determinants of health along with embodiment, also known as the social epidemiology approach in public health.[14]
Biomedical Model of Public Health
Historically, there were attempts to differentiate[15] the concepts of preventive/social/community medicine and public health through its implications in public health practice but have not been engaged with adequately. The concepts of preventive/social/ community ‘medicine’ gave primacy to its activity as that of a medical sub-discipline and hence dominated by medical (therapeutic) or medically induced solutions (vaccines, prophylaxis and so on). Moreover, there are approaches within public health as if it is a medical sub-discipline resulting in interventions targeting secondary and tertiary level prevention of diseases mostly carried out by clinicians. It is assumed here that the health of individuals, when achieved at an aggregate level, can lead to population health, which is reductionist in its orientation.
Another implication of the dominance of medical orientation (community/preventive medicine) within healthcare systems is that the health policies of government predominantly offer curative solutions to public health problems targeted at individuals. Historically, the focus on oral rehydration solution as a ‘magic bullet’ for diarrhoea control across countries implies the biomedical focus on public health problems. A multi-country evaluation study on oral rehydration therapy (ORT) indicates that it could only reduce mortality due to diarrhoea and not the incidence of diarrhoea especially in situations where safe drinking water was lacking.[16] A few chronic disease control initiatives within the healthcare systems reiterate this approach. The Government of India in its programme for control of non-communicable diseases propagates early case detection and treatment of the diseases, but efforts to curb an increasing incidence of the disease is rarely focused on.[17] The dominance of this approach results in conceptualizing public health interventions as those that target individuals and sideline those that focus on social determinants of health.
Social Epidemiology in Public Health
A broader conceptualization of public health primarily targets the population, where rendering medical care is only one among those manifold public health interventions such as ensuring healthy living and working conditions, alleviating social inequalities and so on. The multi-factorial concept of health and disease in this context is in agreement with the societal concept of health systems where multiple determinants are implicit. Social epidemiology, a branch of epidemiology evolved out of a marriage between social theories and epidemiological methods, is a clear departure from the individualist approaches in epidemiology, which addresses the social context more effectively. The primary task of public health practice then is to prevent those populations from the potential illnesses they suffer by virtue of them being members of specific social groups. Populations that are more vulnerable to diseases become the primary target group. Of the various interpretations about population, the one that is statistically defined implicating its relation to the sample is the most extensively used one in the context of traditional epidemiology. Krieger’s[18] critique to this concept of population is relevant here. The relationship between the individual and the population to which one belongs become so important that a critical engagement with this relation in the context of practising public health is inevitable. To quote:
The net result was that a population’s essence—crucial to its success or failure—was conceptualized as an intrinsic property of the individuals who comprised the population; the corollary was that population means and rates were a result and an expression of innate individual characteristics.
This tendency of considering population characteristics as an inherent quality of individuals has been a serious limitation within the field of epidemiology. Drawing inferences on individual characteristics based on population characteristics is strongly critiqued by several scholars both as a form of methodological individualism[19] and also among those engaged with multilevel analysis as forms of fallacies, of which ecological being one.[20],[21] This aspect of reductionism and therefore individualism as an approach is inherent in epidemiology; Krieger attributes this to inappropriate application of chemistry’s ‘law of mass action’, which says that the way chemicals react in smaller quantities will be similar when they are even in larger quantities.[18]
Any effort towards knowledge building in the field of public health has to be in tune with the logic of its area of enquiry, namely the population. Thus, public health practice and therefore public health services of a nation need to conceptualize health behaviour like any other human behaviour as an outcome of their living and working conditions, which in turn is dependent on the social, political, economic and ecological context within which the society is constituted and hence can be understood using the tools of social scientists. The fundamental role of social analysis in epidemiology is articulated by Kaplan[22] as ‘that the problems of disease and the distribution of disease in populations over time and space can be understood from a social perspective only or that such information is in some sense more fundamental than other types of information about disease determinants’. In other words, any attempt to deliver public health services should adopt the population perspective to become successful, whether it is as part of the healthcare systems or in isolation.
Public Health-Oriented Healthcare Systems
At a time, when global health discourse is dominated by health systems,[4] which represents only the country’s healthcare systems, a revised typology which not only examines the authority of government but also the adequacy of medical care and public health services will be more appropriate and relevant. [Figure - 1] shows the disproportionate delivery of medical care and public health services across nations’ healthcare systems belonging to welfare state health systems. This is because in most LMICs the situations are such that healthcare systems are mostly dominated by medical care services with very little or sheer absence of public health services. This is not to say that medical care services offered under these healthcare systems are adequate. For instance, in India (A) the public health services are grossly inadequate compared to the medical care service provision as there are a range of public health problems that fail to have any public health response from the healthcare system. On the other extreme are the Scandinavian countries that ensure a better balance between medical care and public health services delivered as part of their healthcare systems (D) and have achieved their threshold level. The extent of medical care and public health services rendered as part of a country’s healthcare system can vary irrespective of the fact that they have a free enterprise, welfare state or socialist healthcare systems. Every country can benchmark its desired threshold level as a target to be attained. This threshold level for medical care and public health services can be based on the epidemiological situation of a nation and the public health problems it encounters. In other words, the very judgement whether the country’s healthcare should be dominated by medical care or public health services is a question of priority, which in turn is dependent on the ethics of public health practice that should follow the principles of social justice. A detailed discussion on this problem of prioritizing in the context of universal health coverage is given elsewhere.[23]
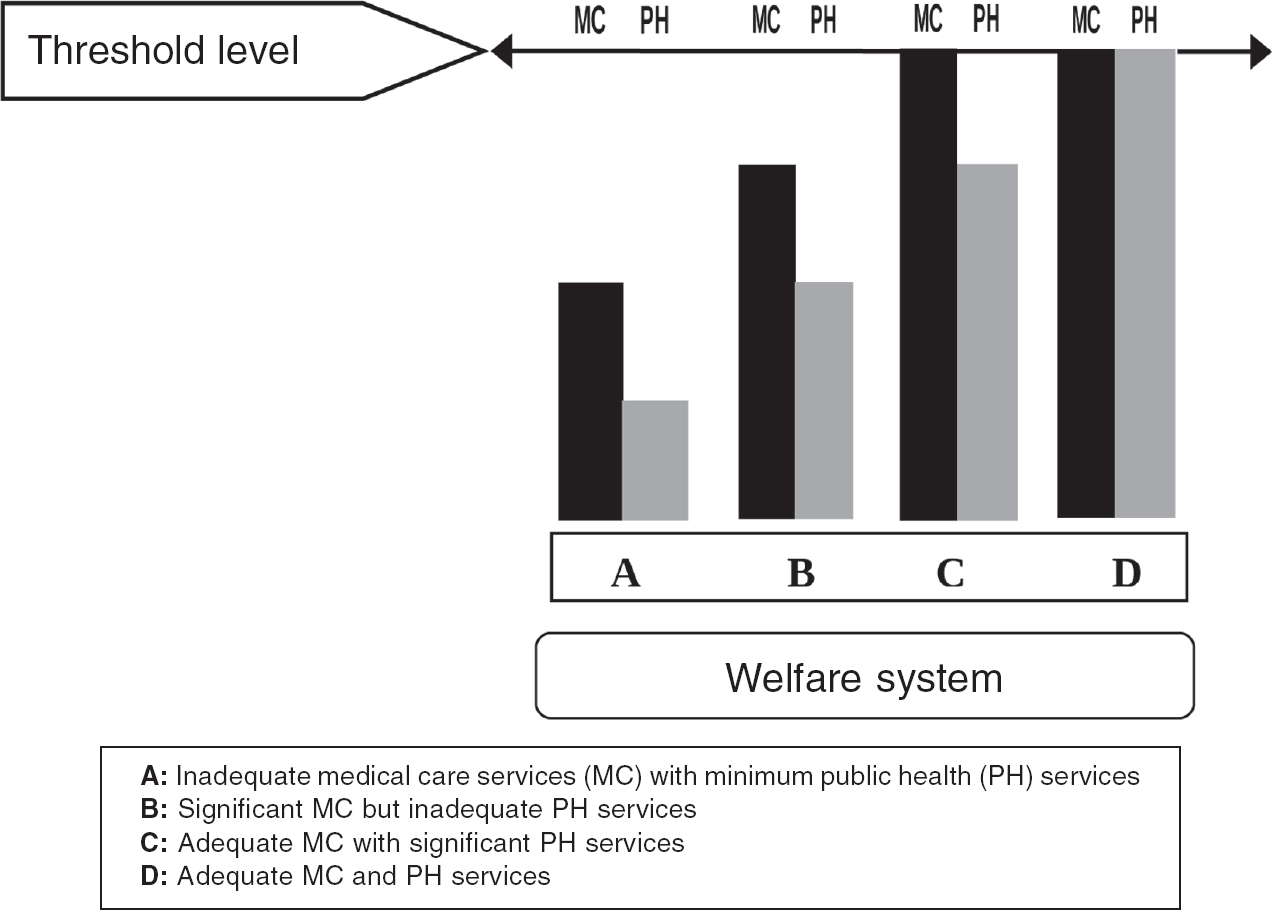 |
| Figure 1: Modified typology showing public health orientation of healthcare systems |
Public health-oriented healthcare systems created by bringing in architectural correction to the existing healthcare systems can strengthen public health across nations by developing mechanisms for ensuring essential public health functions. This will provide opportunities for public health professionals to perform their primary responsibility of routine monitoring of those determinants of population health, thus reducing susceptibility to specific diseases. Failure to acknowledge the social context of disease outcomes might lead to more and more individualistic approaches to public health problems, which in turn could offer greater opportunity for commercial interests within a capitalist system. This is because biomedical approaches being individualist in approach could possibly lead to solutions that are also individually oriented, which becomes the ‘ideal’ environment for developing commodities for individual consumption in the name of public (population) health.
Conclusion
The healthcare system of a nation represents its commitment to the health of its people. Historically, most nations developed healthcare by giving prominence to provisioning of medical care services, thus failing to provide adequate public health services and constraining opportunities for public health practice. Further, the dominance of community medicine-based approaches within public health has resulted in individual-oriented interventions failing to provide benefits to a population. This is reflected by national health programmes and strategies adopted for disease control in most developing countries.[24],[25] One way to ensure population-based approaches in public health practice is by making the healthcare system sensitive to the inadequacies in the offered public health services. A public health-oriented modified typology of a healthcare system is a step towards this direction. Any inadequacy in terms of its capacity to respond to either public health or medical care needs of its people is a concern. These services have to be complementary in nature as there are specific public health needs which acquire priority over medical care needs and vice versa. These decisions are strictly contextual for nations and can be guided only by the ethical principles of social justice. The focus towards public health services becomes so crucial at a time when major concerns in healthcare revolve around the cost of providing medical care. Only if nations acknowledge their need to have adequate public health services as part of healthcare delivery, will there be opportunities for authentic public health practice which can improve population health.
Conflicts of interest. None declared
| 1. | Roemer MI. National health systems of the world. Volume 2. The issues. Oxford:Oxford University Press; 1993. [Google Scholar] |
| 2. | Roemer MI. Health departments and medical care: A world scanning. Am J Public Health Nations Health 1960;50:154-60. [Google Scholar] |
| 3. | Collin C, Green A. Valuing health systems: A framework for low and middle income countries. New Delhi:Sage India; 2014:55. [Google Scholar] |
| 4. | World Health Organization. The world health report2000: Health systems: Improving performance. Geneva:WHO; 2000:5-6. [Google Scholar] |
| 5. | Government of India. National health policy. New Delhi:Ministry of Health and Family Welfare; 2017:1-28. [Google Scholar] |
| 6. | Gupta MD. Public health in India: Dangerous neglect. Econ Polit Wkly 2005;40: 5159-65. [Google Scholar] |
| 7. | George M. Viewpoint: Re-instating a ‘public health’ system under universal health care in India. J Public Health Policy 2015;36:15-23. [Google Scholar] |
| 8. | Field MG. The concept of the ‘health system’ at the macrosociological level. Soc Sci Med 1973;7:763-85. [Google Scholar] |
| 9. | Pellegrino ED, Thomasma DC. A philosophical basis of medical practice: Toward a philosophy and ethic of the healing professions. Oxford:Oxford University Press; 1981:69. [Google Scholar] |
| 10. | Freidson E. The professions of medicine: A study of the sociology of applied knowledge. New York:Dodd, Mead; 1970. [Google Scholar] |
| 11. | Savitz DA, Poole C, Miller WC. Reassessing the role of epidemiology in public health. Am J Public Health 1999;89:1158-61. [Google Scholar] |
| 12. | Pearce N. Traditional epidemiology, modern epidemiology, and public health. Am J Public Health 1996;86:678-83. [Google Scholar] |
| 13. | Shy CM. The failure of academic epidemiology: Witness for the prosecution. Am J Epidemiol 1997;145:479-84. [Google Scholar] |
| 14. | Wemrell M, Merlo J, Mulinari S, Hornborg AC. Contemporary epidemiology: A review of critical discussions within the discipline and a call for further dialogue with social theory. Sociol Compass 2016;10:153-71. [Google Scholar] |
| 15. | The distinction between public health and community/social/preventive medicine. J Public Health Policy 1985;6:435-9. [Google Scholar] |
| 16. | Victora CG, Bryce J, Fontaine O, Monasch R. Reducing deaths from diarrhoea through oral rehydration therapy. Bull World Health Organ 2000;78:1246-55. [Google Scholar] |
| 17. | Patel V, Chatterji S, Chisholm D, Ebrahim S, Gopalakrishna G, Mathers C, et al. Chronic diseases and injuries in India. Lancet 2011;377:413-28. [Google Scholar] |
| 18. | Krieger N. Who and what is a ‘population’? Historical debates, current controversies, and implications for understanding ‘population health’ and rectifying health inequities. Milbank Q 2012;90:634-81. [Google Scholar] |
| 19. | Yadavendu VK. Social construction of health: Changing paradigms. Econ Polit Wkly 2001;36:2784-95. [Google Scholar] |
| 20. | Susser M. The logic in ecological: I. The logic of analysis. Am J Public Health 1994; 84:825-9. [Google Scholar] |
| 21. | Diez-Roux AV. Bringing context back into epidemiology: Variables and fallacies in multilevel analysis. Am J Public Health 1998;88:216-22. [Google Scholar] |
| 22. | Kaplan GA. What’s wrong with social epidemiology, and how can we make it better? Epidemiol Rev 2004;26:124-35. [Google Scholar] |
| 23. | George M. Being fair in universal health coverage: Prioritize public health services for low- and middle-income countries. Am J Public Health 2016;106:830-1. [Google Scholar] |
| 24. | Unger JP, De Paepe P, Green A. A code of best practice for disease control programmes to avoid damaging health care services in developing countries. Int J Health Plann Manage 2003; 18 Suppl 1 :S27-39. [Google Scholar] |
| 25. | Banerji D. Health andfamilyplanning services in India:An epidemiological, socio- cultural and political analysis and a perspective. New Delhi:Lok Paksh; 1985. [Google Scholar] |
Fulltext Views
2,993
PDF downloads
1,181




