Translate this page into:
Publication misconduct: Perceptions of participants of a faculty development programme
2 Department of Paediatrics, Guru Gobind Singh Medical College, Faridkot, Punjab, India
3 Department of Paediatrics, Christian Medical College, Ludhiana, Punjab, India
4 Department of Paediatrics and Medical Education, Christian Medical College, Ludhiana, Punjab, India
Corresponding Author:
Suman P Singh
Department of Microbiology, Pramukhswami Medical College, Karamsad, Gujarat
India
sumanps@charutarhealth.org
| How to cite this article: Singh SP, Dhir SK, Sharma M, Singh T. Publication misconduct: Perceptions of participants of a faculty development programme. Natl Med J India 2018;31:169-171 |
Abstract
Background. Publication misconduct is a commonly reported finding among researchers from various backgrounds including those from the medical sciences. The reasons for such events are diverse and people address them differently.Methods. The opinions and experiences of 72 medical educators enrolled in an online discussion forum for faculty development were analysed to ascertain possible reasons and ways to address publication misconduct.
Results. Of the 50 educators who participated in the discussion, 46 had one or more experiences of publication misconduct to share. Twelve participants felt that almost all kinds of publication misconduct, i.e. fabrication and falsification of data, plagiarism and authorship issues were a universal phenomenon. In the experience of majority of the participants, publication misconduct was common and often no action was taken. Lack of knowledge and awareness among teachers and students, personal gains, pressure for professional advancement and lack of monitoring and control were identified as the reasons for such misconduct. Several solutions were offered by the participants to address the problem, the most common was to have a formal training programme along with stringent monitoring and control mechanisms at the institutional level.
Conclusion. Publication misconduct occurs and people indulge in it for a variety of reasons. Institutional-level policies may be able to address some of these.
Introduction
Scientific publications by the Indian medical fraternity are no more a matter of aptitude, interest and choice as career progression is now linked to publishing of papers.[1],[2] The promotion and publication policies have been debated and critiqued with the concern that there could be a surge in unethical publication practices as well as publication of papers in ‘predatory’ or ‘fake’ journals.[2],[3],[4] Academic achievement if measured by the number of publications can lead to a pressure to publish. Along with a lack of resources and expertise, financial gains particularly in clinical trials can lead to publication or research misconduct.[5],[6]
The Office of Research Integrity (ORI), USA, defines research misconduct as ‘fabrication, falsification or plagiarism in proposing, performing or reviewing research, or in reporting research results '.[7]
The Indian Council of Medical Research (ICMR) in their ethical guidelines for biomedical research on human participants has also described ‘misconduct in research’.[8] Failure to take ethical permission and salami slicing are some issues that have not been included in these guidelines.
Publication misconduct (PM), with an incidence of 0.02% to 72%, is one of the most common reasons for retraction of published work.[6],[9],[10],[11],[12],[13] It is difficult to find the true incidence of PM in the scientific community and different approaches have been adopted by various researchers for its assessment.[5],[6],[l4]
In India, gift authorship, data fabrication and plagiarism are some common forms of misconduct.[15],[16] We share the perceptions and experiences of medical educators from various parts of India, enrolled in an online teaching learning programme on various issues of PM.
Methods
Faculty development (FD) programmes in India have taken initiatives to train faculty in various aspects of medical education including research. One such initiative uses distance-learning platform interspersed with contact sessions through identified centres for FD. Christian Medical College Ludhiana (CMCL) is one such centre. A total of 72 participants from various medical colleges of India were enrolled in this programme at CMCL in 2014–15. In this course, medical educators discuss one topic of relevance each month. The topic is divided into various subtopics and is moderated by a team of participants under faculty mentors. It is conducted using Google groups by creating specific threads.
‘Scientific paper writing and writing for grants’ was one such topic. The topic was divided into three subtopics, namely, ‘The initial steps,' ‘The nitty-gritty’ and ‘The bad apples’ for discussion. Each subtopic was discussed in separate threads one after another and focused on various aspects involved in the planning and writing of scientific papers as well as PM.
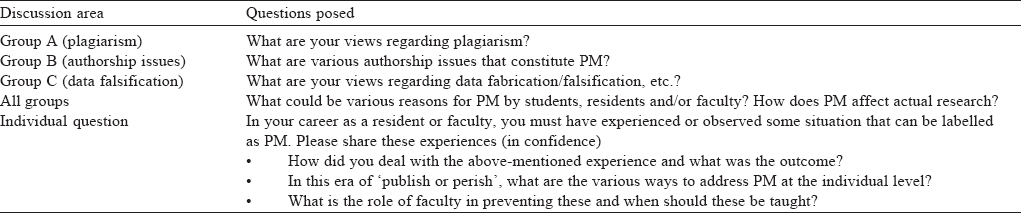
During the subtopic of ‘The bad apples’, the participants discussed various issues of PM. Both group and individual activities were conducted, and specific questions were asked in each activity [Table - 1].
The responses from the participants were noted from the mails and were coded as per specific questions. The coded data were further compiled in related themes and analysed. We present the online discussion about PM and were exempted review by the Institutional Human Research Ethics Committee.
Results
Of the 72 enrolled participants, 50 were involved in the discussion. There were 248 conversations with sharing of personal experiences and other responses.
When personal experiences of 50 participants were analysed, 46 (92%) had an experience to share and 6 acknowledged being involved in PM. Twelve (24%) participants felt that all kinds of PM were ‘a kind of universal phenomenon’. Nine (18%) participants had experienced that junior faculty and postgraduate students were exploited by seniors to a variable extent. In their experience, juniors were made to do the actual work, compile data but then were deprived of authorship. However, this was not the case always as one of the senior participants in spite of contribution in research work was deprived of authorship by junior faculty. Eight participants (16%) felt that gifting authorship was a trend and senior faculty usually take advantage. Gifting authorship to relatives, particularly spouses and developing publication partnerships was commonly observed. Doing research work without ethical approval and salami slicing were reported by three participants each.
In the majority of participants’ experience, PM was considered as ‘normal’ and accepted silently or with frustration. The reasons given were junior position, lack of courage, support, evidence, clarity and/or awareness about what must/can be done. However, all the participants had not accepted PM silently and had reported it to higher authorities (6 participants), confronted the involved persons directly (5 participants), had retracted the article (4 participants), seen disciplinary action (1 participant) and removed the person from the authors’ list (1 participant). Five of the participants also resolved not to tolerate the same in the future.
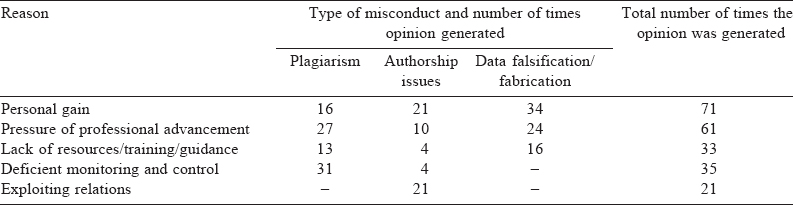
The reasons for PM by the faculty and students were thought to be variable [Table - 2]. Some key reasons given were:
- For undergraduate students: Lack of awareness or innocence, lack of knowledge of research guidelines, lack of mentors or bad role models. Competition for good grades in time-bound assignments and easy access to others ' work due to technological advancements.
- For postgraduate students: Lack of research training, unclear institutional policy or guidelines, lack of formal and effective mentoring, inability to balance work pressure and academic requirements such as thesis, seminars and presentations.
- For faculty : Research incompetence and lack of aptitude, publication pressure due to its link with promotion, competition with colleagues, pressure to enhance their resume for getting scholarships and grants.
Participants believed that all forms of PM have a direct influence on the credibility and authenticity of true research and it is a crime against humanity (particularly in medicine).
Various suggestions by participants to address the issue of PM included sensitization, orientation and training programmes for faculty and students (50 participants), to have a formal curriculum for undergraduate/postgraduate students (7 participants), effective role modelling by faculty (18 participants), having robust individual/institutional value system (16 participants), clear guidelines and institutional policy (13 participants), developing monitoring mechanisms (10 participants), active role of ethics committee and a conducive institutional environment (8 participants), effective mentoring and strict action against offenders (6) and use of software and technology to catch the offender (4).
Discussion
The Medical Council of India defines what constitutes professional misconduct and the regulations framed by the ICMR need to be followed for research purposes.[17] Scientific misconduct, a part of academic dishonesty, is present in the Indian education system including medical education.[18],[19]
Dhingra et al. reported 65% gift authorship, 56% fabrication/ falsification of data, 53% plagiarism and 33.5% credit not being given to those who deserve to be authors.[15] This makes PM common among Indian doctors, as is also evident from the opinion expressed by our participants.
The main reasons for PM among the Indian medical fraternity are reported to be intense competition, pressure to publish, insufficient facilities, inadequate funds, lack of statutory controls and policies to deal with scientic misconduct, academic ignorance due to lack of knowledge and training about research methodology, research ethics, publication guidelines and scientic writing.[5],[20] Our participants also shared similar opinions and felt lack of knowledge and awareness to be the most common reason; thus there is a need for formal curriculum and training both for students and faculty. They also identified personal value systems (54%) and institutional culture (32%) as important factors in PM.
The Committee on Publication Ethics (COPE) has issued guidelines to detect scientific misconduct, and editorial boards of medical journals are in a position to detect PM but may not always have the resources, expertise or will to do so.[21],[22] Along with these guidelines, our participants felt the need for an institutional policy that is communicated to all stakeholders. Plagiarism, the most common malady afflicting the Indian system, can be prevented to some extent by the use of software available to journal editors and reviewers, but involves cost and the method is not foolproof. Thus our study participants felt the need to put budgetary allocations by institutions for such software, use of e-case record forms and more authority to institutional research and ethics review boards.[5],[15],[16]
Fang et al. in their review of retraction of published articles found that 67.4% of retractions were due to PM and the retraction rates have increased 10- to 19-fold over a decade.[12]
In spite of being common, such events are rarely reported due to lack of awareness about what can be done in such an event, though COPE flow charts can guide actions in specific events.[21] Rejecting the manuscript, censuring the author, informing institutional authorities about PM and retracting the article are some measures adopted by journals, but these steps may not always be easy to implement.[16] In a study by Singh and Guram, 67% of participants wanted that retraction of the plagiarised article alone should be adequate punishment.[5] Other actions include disciplinary action by the institution, withdrawal of gains due to publication if any, for example, promotion.[5]
In a systematic review, the action taken was reported in 12%– 55% of cases.[10] Direct confrontation with the researcher (55.5%) was the most common. Other actions were: reporting to relevant persons/organizations, disciplinary action by the dean, reporting to institutional review board, discussion with colleague, etc. Our participants reported to the higher authorities (12%), direct confrontation (10%), article retraction (8%), and disciplinary action by one; 12% of participants also felt the need for zero tolerance with strict disciplinary action against PM.
Such academic misconduct must be recognized and controlled by awareness, objective check methods and stringent punishment.[5],[11] Efforts to address the issue of PM have been made in various countries by creating organizations such as the ORI in America and COPE in the UK, Grant organizations in Canada, and ICMR guidelines in India.[8],[22],[23] The International Committee of Medical Journal Editors (ICJME) has laid down authorship criteria based on credit and accountability, which have been adopted by the ICMR as well as journal editors in India. In spite of this, specific guidelines and stringent actions that must be taken in case of scientific misconduct are lacking in India. In its Guidelines on Code of Conduct for Research Scientists, the ICMR mentions that unethical practices such as fabrication, falsification and plagiarism should be avoided.[24] The phrase ‘should be avoided’ does not convey the gravity of the issue.
The limitations of our study are: a small sample size, the lack of a structured questionnaire to gather data and inability to generalize the results because of including only medical educators. However, we hope the experiences and opinions of medical educators can be useful in controlling PM.
At an individual level, the most common factor that can prevent PM is gaining knowledge about various aspects of PM and adhering to moral values. Overall institutional culture should be conducive for research to prevent PM. All participants believed that creating awareness about various acts and their consequences for students and faculty will play a crucial role in preventing such acts.
The problem of PM is real, the reasons why people indulge in PM are variable and ways to address them are not straightforward. The ‘bad apples’ must be identified before they impact the credibility of the scientific data beyond repair.
Conflicts of interest. None declared
| 1. | Circular-03.09.2015-TEQ-Promot1on-Publication.pdf. Available at www.mciindia">www.mciindia. org/circulars/Circular-03.09.2015-TEQ-Promotion-Publication.pdf< (accessed on 30 May 2017). [Google Scholar] |
| 2. | Bavdekar SB, Tullu MS. Research publications for academic career advancement: An idea whose time has come. But is this the right way? J Postgrad Med 2016;62: 1-3. [Google Scholar] |
| 3. | Bandewar SV, Pai SA. Regressive trend: MCI’s approach to assessment of medical teachers’ performance. Indian J Med Ethics 2015;12:192-5. [Google Scholar] |
| 4. | Aggarwal R, Gogtay N, Kumar R, Sahni P, Indian Association of Medical Journal Editors. The revised guidelines of the Medical Council of India for academic promotions: Need for a rethink. Indian Pediatr 2016;53:23-6. [Google Scholar] |
| 5. | Singh HP, Guram N. Knowledge and attitude of dental professionals of North India toward plagiarism. N Am J Med Sci 2014;6:6-11. [Google Scholar] |
| 6. | Lock S. Fraud in medical research. Issues Med Ethics 1997;5:112-14. [Google Scholar] |
| 7. | Definition of research misconduct. ORI—The Office of Research Integrity. Available at www.ori.hhs.gov/definition-misconduct">www.ori.hhs.gov/definition-misconduct (accessed on 30 Nov 2016). [Google Scholar] |
| 8. | ICMR Ethical Guidelines for Biomedical Research. Available at www. icmr. nic. in/ ethical_guidelines.pdf (accessed on 30 Nov 2016). [Google Scholar] |
| 9. | Lafollette MC. The evolution of the ‘scientific misconduct’ issue: An historical overview. Proc Soc Exp Biol Med 2000;224:211-15. [Google Scholar] |
| 10. | Fanelli D. How many scientists fabricate and falsify research? A systematic review and meta-analysis of survey data. PLoS One 2009;4:e5738. [Google Scholar] |
| 11. | Damineni RS, Sardiwal KK, Waghle SR, Dakshyani MB. A comprehensive comparative analysis of articles retracted in 2012 and 2013 from the scholarly literature. J Int Soc Prev Community Dent 2015;5:19-23. [Google Scholar] |
| 12. | Fang FC, Steen RG, Casadevall A. Misconduct accounts for the majority ofretracted scientific publications. Proc Natl Acad Sci USA 2012;109:17028-33. [Google Scholar] |
| 13. | Steen RG, Casadevall A, Fang FC. Why has the number of scientific retractions increased? PLoS One 2013;8:e68397. [Google Scholar] |
| 14. | Elia N, von Elm E, Chatagner A, Pöpping DM, Tramèr MR. How do authors of systematic reviews deal with research malpractice and misconduct in original studies? A cross-sectional analysis of systematic reviews and survey of their authors. BMJ Open 2016;6:e010442. [Google Scholar] |
| 15. | Dhingra D, Mishra D. Publication misconduct among medical professionals in India. Indian J Med Ethics 2014;11:104-7. [Google Scholar] |
| 16. | Eldawlatly A, Shafer SL. Caveat lector. Saudi J Anaesth 2012;6:99-101. [Google Scholar] |
| 17. | Code of Medical Ethics Regulations; 2002. Available at www.mciindia">www.mciindia.org/ RulesandRegulations/CodeofMedicalEthicsRegulations2002.aspx (accessed on 30 May 2017). [Google Scholar] |
| 18. | Gitanjali B. Academic dishonesty in Indian medical colleges. J Postgrad Med 2004;50:281-4. [Google Scholar] |
| 19. | MacAskill A, Stecklow S, Miglani S. Broken health: Rampant fraud plagues Indian medical schools. Reuters. Available at www.reuters.com/investigates/special-report/india-medicine-education">www.reuters.com/investigates/special-report/india-medicine-education (accessed on 30 May 2017). [Google Scholar] |
| 20. | Juyal D, Thawani V, Thaledi S. Rise of academic plagiarism in India: Reasons, solutions and resolution. Lung India 2015;32:542-3. [Google Scholar] |
| 21. | Schoenherr JR. Scientific integrity in research methods. Front Psychol 2015;6:1562. [Google Scholar] |
| 22. | Marcovitch H. Committee on publication ethics flow charts on suspected publication misconduct. Maturitas 2009;62:207. [Google Scholar] |
| 23. | Committee on Publication Ethics: COPE, Promoting Integrity in Research Publication. Available at www.publicationethics.org/">www.publicationethics.org/ (accessed on 30 May 2017). [Google Scholar] |
| 24. | Revised_Code_of_conduct_for_Researchers_–Code of Conduct for Research Scientists Engaged in the Field of Life Sciences.pdf. Available at www.icmr.nic.in/guidelinescoe%20of%20conduct%20for%20research%20scientists%20">www.icmr.nic.in/guidelinescoe%20of%20conduct%20for%20research%20scientists%20 engaged%20i n%20the%20field%20of%20life%20sciences.pdf (accessed on 30 May 2017). [Google Scholar] |
Fulltext Views
5,393
PDF downloads
12,310




