Translate this page into:
Septic arthritis in a newborn
[To cite: Dubepuria A, Behera P, Khare C. Septic arthritis in a newborn (Correspondence). Natl Med J India 2023;36:401. DOI: 10.25259/NMJI_1098_2022]
A preterm newborn infant (36 weeks, weight 2500 g) developed fever, excessive crying and decreased movements of the left lower limb on day 10 of life. The infant was admitted in a primary care hospital for suspected sepsis. However, with fever persisting and an evolving left knee swelling, the infant was referred to us while on day 5 of intravenous antibiotics. We found the newborn to be febrile, the left knee to be affected with frank signs of septic arthritis and high inflammatory markers (C-reactive protein [CRP] 58 mg/dl). A joint effusion on an ultrasound and X-ray suggested of periosteal reaction around the distal femur extending to the distal femoral physis with a partial loss of the lateral femoral condyle (Fig. 1a). A surgical debridement drained 20 ml of pus. Intraoperatively, a part of the lateral femoral condyle was found to be de-vitalized and lying separate from the rest of the femur (Fig. 1b). The infant improved after debridement of the joint, as shown1 by decreased inflammatory markers (CRP 3.8 mg/dl within 3 days of surgery). The infant received amoxicillin–clavulanate for 4 weeks based on the sensitivity pattern of Staphylococcus aureus that grew on blood culture (methicillin-sensitive).
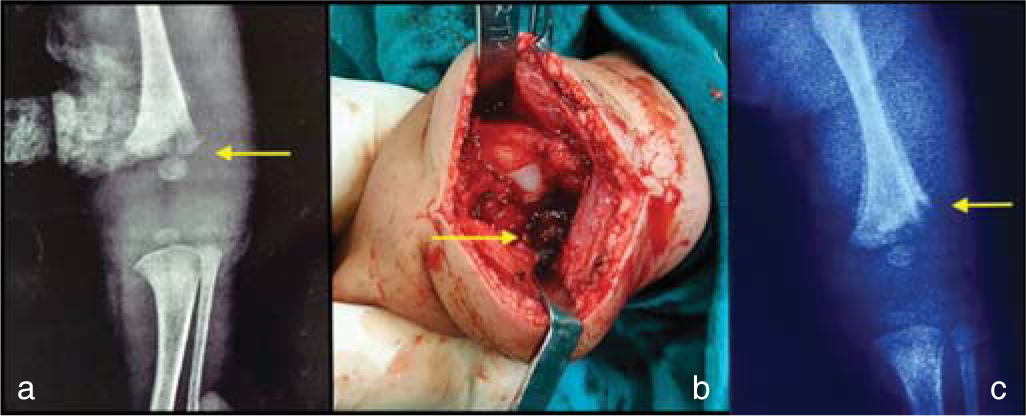
- (a) Preoperative antero-posterior X-ray of the left knee showing a lucent zone (yellow arrow); (b) intraoperative image demonstrates an intact medial condyle and a deficient lateral femoral condyle (yellow arrow); (c) postoperative (10 days) antero-posterior X-ray showing the now absent lateral femoral condyle (yellow arrow)
Devastating joint damage in neonatal septic arthritis continues to be a concern in low-resource settings.1–3 It is complicated by numerous uncertainties and knowledge gaps. First, a major burden of preterm and low-birth weight newborns in low- to middle-income settings are predisposed to septic arthritis; an inherent risk in infancy.2 Second, subtle signs of joint inflammation evoke less suspicion in the newborn nursery, especially in preterm infants, until optimal inflammatory signs appear. Screening of a joint by an ultrasound and/or X-ray is less informative as an abnormality is indicative of an evolved disease and does not rule out complications per se; an abnormal joint ultrasound was noted in only 60% of septic arthritis in one report.2,3 So, a ‘definitive indication to intervene’ based on clinical or radiological tests is often late and suboptimal to prevent joint complications as seen in our patient. Third, recent reports suggest continued controversy regarding timing and outcome of surgery. Surgical drainage of the joint is the mainstay of treatment in neonatal septic arthritis as it decreases the bacterial load and intra-articular pressure, thereby decreasing the risk of complications. However, there is no consensus on whether all patients with septic arthritis must undergo surgery.3 There is agreement on unfavourable joint outcomes in the presence of an abnormal X-ray or substantial joint effusion on ultrasound at admission. The complication of unilateral femoral condyle loss is postulated to cause vascular ischaemia due to the compartment syndrome in the presence of infrapatellar synovial septae.4,5 Disturbance in the growth of long bones resulting in angular deformity or limb length discrepancy is a sequelae of septic arthritis in infancy.5–10 Such an event does not have an obvious solution for every affected child and attempts must be made to avoid this complication. Clinicians caring for a newborn must be aware of subtle signs of neonatal septic arthritis and seek an early opinion from their orthopaedic colleagues.
References
- Septic arthritis of the knee in children: A critical analysis review. JBJS Rev. 2020;8:e0069.
- [CrossRef] [PubMed] [Google Scholar]
- Neonatal septic arthritis: Indian perspective. Eur J Rheumatol. 2020;7:S72-S77.
- [CrossRef] [PubMed] [Google Scholar]
- Delayed treatment of septic arthritis in the neonate: A review of 52 cases. Medicine (Baltimore). 2016;95:e5682.
- [CrossRef] [PubMed] [Google Scholar]
- Developments in diagnosis and treatment of paediatric septic arthritis. World J Orthop. 2022;13:122-30.
- [CrossRef] [PubMed] [Google Scholar]
- Loss of a condyle of the femur or tibia following septic arthritis in infancy: Problems of management and testing of a hypothesis of pathogenesis. J Child Orthop. 2012;6:319-25.
- [CrossRef] [PubMed] [Google Scholar]
- Disturbed epiphysial growth at the knee after osteomyelitis in infancy. J Bone Joint Surg Br. 1970;52:692-703.
- [CrossRef] [PubMed] [Google Scholar]
- Growth disturbance after osteomyelitis of femoral condyles in infants. Acta Orthop Scand. 1984;55:1-13.
- [CrossRef] [PubMed] [Google Scholar]
- Partial destruction of the distal femoral epiphysis as a consequence of osteomyelitis: Regeneration after transplantation of a bone graft. J Pediatr Orthop. 1985;5:731-3.
- [CrossRef] [PubMed] [Google Scholar]
- "Missing" femoral condyle: An unusual sequela to neonatal osteomyelitis and septic arthritis. Radiology. 1986;161:359-61.
- [CrossRef] [PubMed] [Google Scholar]
- Sequelae from septic arthritis of the knee during the first two years of life. J Pediatr Orthop. 1994;14:745-51.
- [CrossRef] [PubMed] [Google Scholar]




