Translate this page into:
Smartphone fundus photography by a physician in medical emergencies: An analytical cross-sectional study of 182 patients
Correspondence to S. DEEPAK AMALNATH; drdeepakmddm@yahoo.co.in
[To cite: Pradeep R, Amalnath SD, Kasturi N. Smartphone fundus photography by a physician in medical emergencies: An analytical cross-sectional study of 182 patients. Natl Med J India 2023;36:291–4. DOI: 10.25259/NMJI_208_21]
Abstract
Background
Fundus examination is an integral part of the clinical evaluation of patients with medical emergencies. It is done at the bedside using a portable direct ophthalmoscope. Smartphone fundus photography (SFP) is a novel technique of retinal imaging. We evaluated the use of SFP by a physician in medical emergencies and compared it with direct ophthalmoscopy (DO) findings of the ophthalmologist.
Methods
We did a prospective study on patients admitted with medical emergencies with an indication for fundus examination. The SFP was done by the physician, and its findings were noted. These were compared with the DO findings of the ophthalmologist.
Results
Of the 182 patients studied, 111 (61%) had fundus findings by SFP and 95 (52.5%) by DO. Papilloedema (21.4%), haemorrhages (20%) and Roth spots (12.5%) were most common. DO missed early papilloedema and findings in the peripheral retina.
Conclusions
SFP is as effective as DO, in detecting retinal findings in patients with medical emergencies and can be performed at the bedside by the physician.
INTRODUCTION
Examination of the ocular fundus is an essential part of clinical evaluation as it gives vital clues to the diagnosis and severity of the patient’s illness. The retina is the only portion of the central nervous system which can be seen from the outside. Likewise, the retina is the only location where the vasculature (arteries, veins and capillaries) can be seen from the outside. Thus, it provides an excellent window to assess any end-organ damage and staging of chronic diseases such as diabetes and hypertension. The role of fundoscopy in medical emergencies is in detecting papilloedema in the presence of raised intracranial pressure, which is a contraindication for lumbar puncture.
Furthermore, a fundoscopic examination can discover pathological process, which is not otherwise evident, for instance in recognizing endocarditis, disseminated candidaemia, choroidal tubercles, cytomegalovirus infection, etc. Even though fundus examination is critical, it is often neglected in routine practice because it is time-consuming, needs expertise and, if not done correctly, can miss findings of clinical importance. Usually, the trained physician or ophthalmologist performs fundus examination for medical emergencies using a portable hand-held direct ophthalmoscope (DO).
Other techniques of analysing the fundus are by slit-lamp biomicroscopy using +78D or +90D lens, indirect ophthalmoscopy and fundus photography using a specialized fundus camera. These cannot be done by a physician as a bedside procedure.
Smartphone fundus photography (SFP) is a novel technique based on the principle of indirect ophthalmoscopy where fundus photograph is taken by a smartphone and a 20D lens.1 SFP allows for a bedside fundus examination by a nonophthalmologist and is relatively easy to master. Commercial adaptors are available to align the lens with the smartphone. The adaptor can be made of readily available materials such as insulation tapes and polyvinyl chloride pipes (DIYretCAM – do it yourself retinal camera). One end of the adaptor is attached to a 20D lens, and the smartphone is attached to the other side. The flashlight in the smartphone acts as a light source. These images can be saved and sent to the ophthalmologist for expert opinion, stored and retrieved at the time of follow-up.
SFP currently plays a vital role in outreach programmes where there is a lack of clinicians or limited availability of traditional fundus cameras.1 It is commonly used in ophthalmology for screening conditions such as diabetic retinopathy, glaucoma and retinopathy of prematurity.2 However, the use of SFP in medical conditions by physicians, especially in medical emergencies, has not been evaluated. We assessed the role of SFP by physicians as a bedside technique in medical emergencies.
METHODS
We did a prospective observational study on patients admitted in the emergency medical wards at a tertiary care centre from January 2019 to June 2020. Approval of the institute ethics committee was obtained. The inclusion criteria were patients above 18 years of age with any indication for fundus evaluation such as altered sensorium (Glasgow Coma Scale <9), indication for lumbar puncture (to rule out papilloedema), bleeding manifestations and fever of more than 1 week or unknown origin (suspected tuberculosis, infective endocarditis, HIV, etc.). Patients with prior eye surgeries, glaucoma suspects (shallow anterior chamber) and allergy to tropicamide eye drops were excluded. All consecutive patients fulfilling inclusion criteria were included after obtaining written informed consent. The smartphone used in our study was GOOGLE PIXEL 2, which has a 12.2-megapixel camera with light-emitting diode flash. Cardboard adaptor was made as per the method published by Raju et al.,3 to hold a 20D lens. The initial evaluation and fundus photographs were taken by observer 1 (physician). The picture was sent by WhatsApp mobile application and cross-checked by observer 2 (ophthalmologist). Direct ophthalmoscopy (DO) was performed by observer 3 (duty ophthalmology senior resident). Time taken for both techniques was noted. The findings of observers 1 and 2 were compared. The compiled results of observers 1 and 2 were labelled as findings by SFP, and it was compared with observer 3’s findings, i.e. DO findings.
Statistical methods
The normalcy of all the data was assessed using Kolmogorov– Smirnov test. As there was an overlap in findings, percentage calculation was not possible. Statistics were analysed using IBM Statistical Product and Service Solutions (SPSS) version 20. The interobserver concordance for each area in the fundus was calculated separately by kappa statistic. The inter-rater reliability index was then rated based on the Cohen kappa inter-rater reliability index.
RESULTS
A total of 182 patients were included in the study, of which 106 were men (58.2%) and 76 were women (41.8%). Comorbid conditions such as diabetes and hypertension were present in 43.9% of patients. Other comorbid conditions included hypothyroidism (5 patients), systemic lupus erythematosus (2 patients) and HIV (4 patients). The most common indication for fundus examination was a fever of unknown origin, followed by altered sensorium.
Smartphone fundus photography
Fundus findings were present in 111 (61%) patients (Table I and Figs 1 and 2). Papilloedema was the most common (39 patients), followed by retinal haemorrhages and Roth spots. Choroid tubercles were present in 6 patients.
Observer 1 missed seven findings (papilloedema 3, Roth spots 1, vessel abnormalities 3 and choroid tubercles 1), which were identified by observer 2 on evaluating the photos.
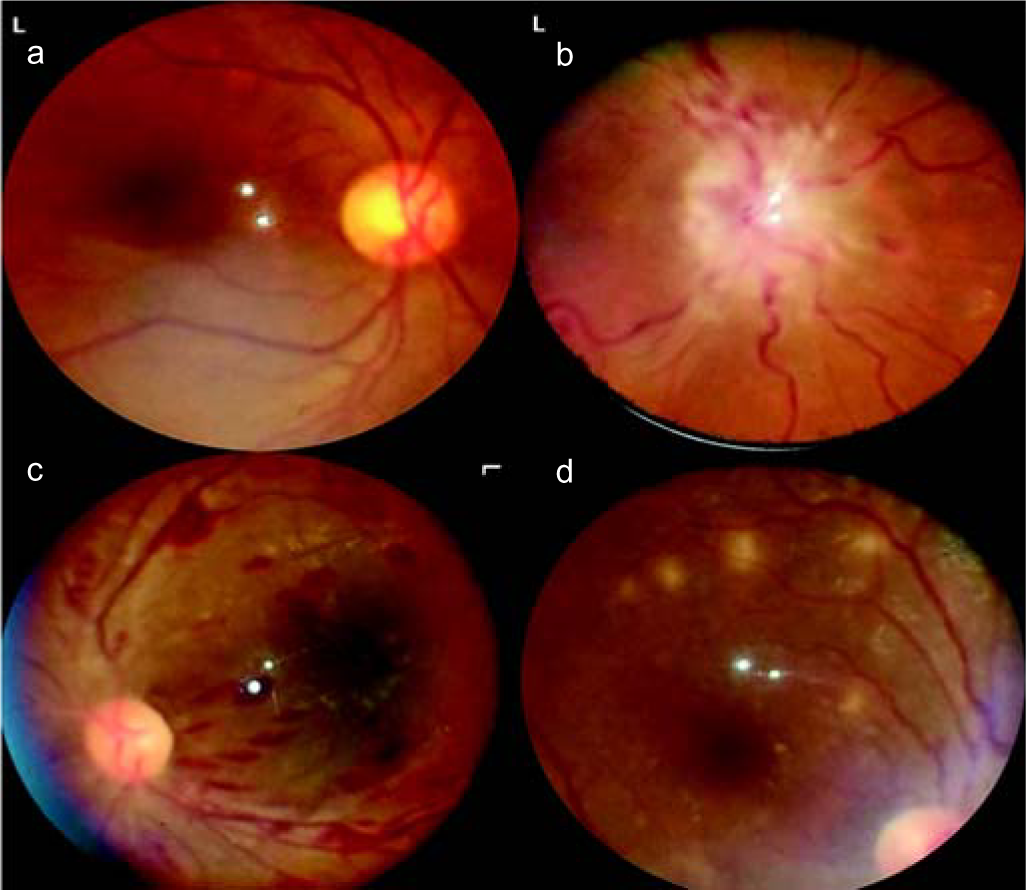
- (a) Normal fundus; (b) established papilloedema in malignant hypertension; (c) Roth spots in acute leukaemia; (d) multiple choroid tubercles in miliary tuberculosis
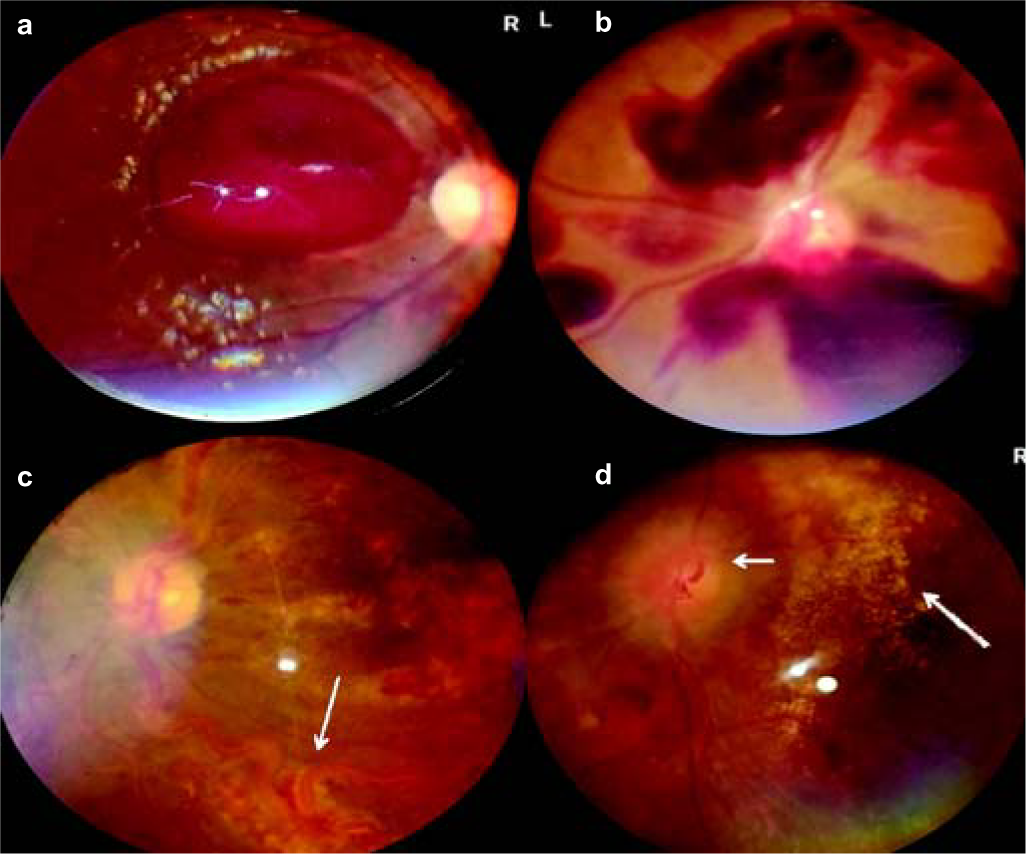
- (a) Subhyaloid haemorrhage in aplastic anaemia; (b) extensive retinal bleeds in acute leukaemia; (c) frosted branch angiitis in cytomegalovirus retinitis; (d) macular star (long arrow) and papilloedema (short arrow) in malignant hypertension
| Finding | Smartphone fundus photography (%) | Direct ophthalmoscopy (%) | K coefficient | Interpretation |
|---|---|---|---|---|
| Papilloedema | 39 (21.4) | 33 (18.3) | 0.896 | Strong agreement |
| Pallor | 6 (3.2) | 4 (2.1) | 0.795 | Moderate agreement |
| Cupping | 1 (0.5) | 1 (0.5) | 1.000 | Perfect agreement |
| Optic disc atrophy | 3 (1.6) | 3 (1.6) | 1.000 | Perfect agreement |
| Disc bleed | 2 (1.0) | 2 (1.0) | 1.000 | Perfect agreement |
| Roth spots | 23 (12.6) | 17 (9.4) | 0.832 | Strong agreement |
| Superficial/deep haemorrhages | 37 (20.3) | 35 (19.2) | 0.965 | Almost perfect agreement |
| Cotton wool spots | 14 (7.6) | 14 (7.6) | 1.000 | Perfect agreement |
| Hard exudates | 16 (8.7) | 16 (8.7) | 1.000 | Perfect agreement |
| Choroid tubercles | 6 (3.2) | 4 (2.1) | 0.795 | Moderate agreement |
| Vessel abnormalities | 16 (8.7) | 15 (8.2) | 0.931 | Almost perfect agreement |
| Macular star | 9 (4.9) | 9 (4.9) | 1.000 | Perfect agreement |
| Macular oedema | 2 (1.0) | 2 (1.0) | 1.000 | Perfect agreement |
| Macular haemorrhage | 5 (2.7) | 5 (2.7) | 1.000 | Perfect agreement |
| Macular atrophy | 1 (0.5) | 1 (0.5) | 1.000 | Perfect agreement |
| Mean k coefficient | 0.946 | Almost perfect agreement |
Comparison with findings of DO
Of the 111 patients, DO missed 19 findings (early papilloedema 6, Roth spots 6, disc pallor 2, retinal haemorrhages 2, choroid tubercles 2, retinal vessel abnormality 1). The overall agreement between the two techniques was almost perfect (kappa coefficient 0.946).
Other findings
Diabetic retinopathy was present in 7 of the 50 people with diabetes, hypertensive retinopathy in 9 of 33 persons with hypertension (grade 3 in 3 and grade 4 in 6) and 2 patients had HIV retinopathy and SLE retinopathy, respectively. All of them were identified by both techniques.
SFP took an average of 4.83 minutes less than DO (23.19 v. 28.05 minutes, p<0.01).
Cataract and other artefacts
Cataract was present in 42 patients. The SFP method took 2 minutes more compared to those without cataracts (23.01 v. 25.14 minutes, p<0.01). Furthermore, the images were less clear compared to those without a cataract. Excessive tears, photophobia and scratches in the lens were other causes of artefacts in the fundus photos (Fig. 3).
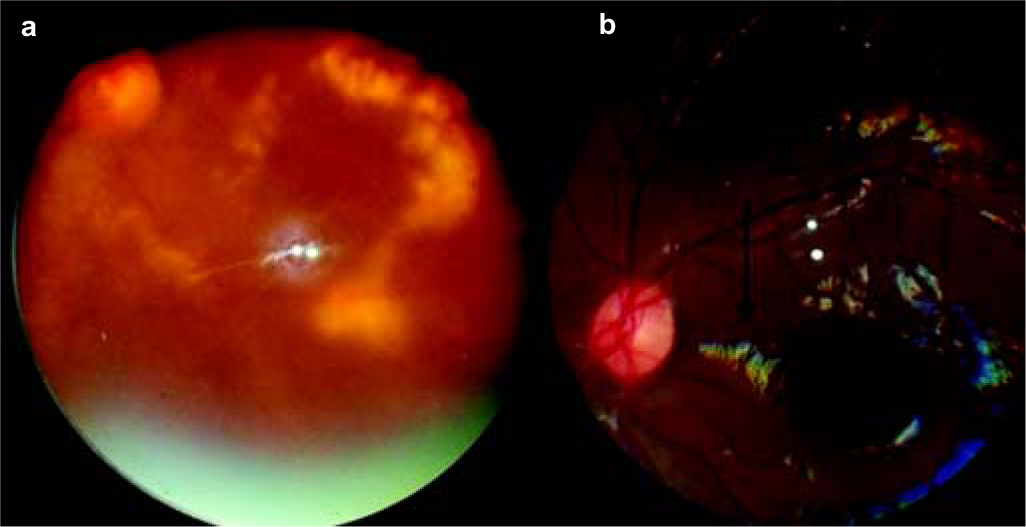
- (a) Blurred picture of diabetic retinopathy, due to cataract;(b) excessive tears mimicking macular lesions
DISCUSSION
Only a few studies have analysed the role of fundus examination in emergency settings. The FOTO-ED study enrolled 350 patients who attended the emergency department and had an indication for fundus evaluation such as headache and neurological deficits.4 Fundus photographs taken by a fundus camera were compared to DO reports of the emergency physician. However, only 14% of the patients had their fundus evaluated by emergency physicians. Of these 350 patients, 13% had significant retinal findings, and all were missed by the emergency physicians. This study showed the importance of fundus examination in medical emergencies.
Many ophthalmological studies have shown the reliability of SFP as a tool to identify common eye disorders such as optic disc cupping for glaucoma, screening for diabetes and retinopathy of prematurity.5–9 However, the fundus photos were taken by nurses and technicians in the community as well as in hospitals. These studies have shown the accuracy of SFP compared to other methods such as hand-held fundus cameras.
We could find only one study that compared DO with a smartphone fundoscopy in medical emergencies. Muiesan et al. studied patients with acute hypertension.10 The fundus pictures were taken by a medical student and cross-checked with an ophthalmologist. This study used a non-mydriatic D-EYE system. Nineteen of 52 patients (36.5%) had important fundus findings, while DO did not identify any finding. In our study, 27.2% of the patients with hypertension had grade 3 or 4 changes.
In our study, fundus findings were present in 61% compared to 13% in the FOTO-ED study.6 DO missed early papilloedema, which was identified by SFP. Findings in the retinal periphery such as haemorrhages, Roth spots and choroid tubercles were identified better by SFP compared to DO. The advantages include storing the images for further follow-up and an easy method to get a second opinion from ophthalmologists. Furthermore, the need to go close to the patient during the DO method is not required in SFP since the photograph is taken at 30–40 cm, thereby reducing the risk of airborne infections to the physician. Although the non-mydriatic D-EYE system does not need pupillary dilatation, it cannot adequately visualize the periphery of the fundus and works only on the iPhone series while the method used in our study can be used in any mobile phone.
The limitations of our study include a wide range of indications for fundus photography and different observers used for various techniques. It is possible that some findings were missed by both DO and SFP. Comparison of these two within DO or wide-angled fundus cameras would have been ideal.
Conclusion
Fundus examination by SFP by a physician is a low-cost alternative to DO, offering vital clues regarding the underlying disease process in patients with medical emergencies that correlates well with the findings of an ophthalmologist.
ACKNOWLEDGEMENTS
We thank Drs Biju Raju, N.S.D. Raju, John Davis Akkara and Avinash Pathengay for their guidance in making the adapter.
Conflicts of interest
None declared
References
- Smartphone assisted fundus fundoscopy/photography. Curr Ophthalmol Rep. 2008;6:46-52.
- [CrossRef] [Google Scholar]
- Fundus photography in the 21st century-A review of recent technological advances and their implications for worldwide healthcare. Telemed J E Health. 2016;22:198-208.
- [CrossRef] [PubMed] [Google Scholar]
- Do it yourself smartphone fundus camera-DIYretCAM. Indian J Ophthalmol. 2016;64:663-7.
- [CrossRef] [PubMed] [Google Scholar]
- Feasibility of non-mydriatic ocular fundus photography in the emergency department: Phase I of the FOTO-ED study. Acad Emerg Med. 2011;18:928.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical validation of a smartphone-based adapter for optic disc imaging in Kenya. JAMA Ophthalmol. 2016;134:151-8.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic accuracy of community-based diabetic retinopathy screening with an offline artificial intelligence system on a smartphone. JAMA Ophthalmol. 2019;137:1182-8.
- [CrossRef] [PubMed] [Google Scholar]
- Non-contact smartphone-based fundus imaging compared to conventional fundus imaging: A low-cost alternative for retinopathy of prematurity screening and documentation. Sci Rep. 2019;9:19711.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of nonmydriatic digital retinal imaging versus dilated ophthalmic examination for nondiabetic eye disease in persons with diabetes. Ophthalmology. 2006;113:833-40.
- [CrossRef] [PubMed] [Google Scholar]
- Smartphone-based fundus imaging-where are we now? Asia Pac J Ophthalmol (Phila). 2020;9:308-14.
- [CrossRef] [PubMed] [Google Scholar]
- Ocular fundus photography with a smartphone device in acute hypertension. J Hypertens. 2017;35:1660-5.
- [CrossRef] [PubMed] [Google Scholar]




