Translate this page into:
Status and trend of acute encephalitis syndrome and Japanese encephalitis in Bihar, India
2 Department of Community Medicine, ESIC Medical College, Sanat Nagar, Hyderabad, India
3 State Programme Officer (Malaria), Chief Malaria Office, Patna, Bihar, India
4 Maternal Health Specialist, Bihar Technical Support Programme, Care India, Patna, Bihar, India
Corresponding Author:
P M Pisudde
Department of Community Medicine, ESIC Medical College, Sanat Nagar, Hyderabad
India
drpravinpisudde@gmail.com
| How to cite this article: Kumar P, Pisudde P M, Sarthi P P, Sharma M P, Keshri V R. Status and trend of acute encephalitis syndrome and Japanese encephalitis in Bihar, India. Natl Med J India 2017;30:317-320 |
Abstract
Background. Acute encephalitis syndrome (AES) is a clinical condition, of which the most common cause is Japanese encephalitis (JE). Though there is deficiency of data on AES and JE from Bihar, the state ranks third in the reporting of JE cases after Uttar Pradesh and Assam. We aimed to assess the status and trends of AES and JE cases in Bihar and to know the status of the disease in the districts.Methods. We collected monthly epidemiological data for AES and JE for the period 2009–2014.
Results. A total of 4400 cases (733 cases/year) with an average case fatality rate (CFR) of 30% for AES for the entire study period. A total of 396 cases of JE were reported with approximately 14% CFR. The disease peaks were during the start and end of the Indian summer and monsoon months for AES and JE, respectively. Districts such as Patna, Jehanabad, Nawada, Gaya and East Champaran reported the maximum number of AES and JE cases with annual incidence rates of 4.7–25.0 and 0.546–1.78 per 100 000 population, respectively.
Conclusion. Since 2009, the incidence of AES and JE cases has been increasing in Bihar.
Introduction
Acute encephalitis syndrome (AES) is a multifactorial clinical condition, the most common cause being Japanese encephalitis (JE). JE is a vector-borne viral disease caused by the JE virus of group B arbovirus (Flavivirus) and is transmitted to humans by the Culicine mosquito. JE affects the central nervous system (CNS), and can cause serious complications and death. The case fatality rate (CFR) is high and those who survive may suffer from neurological sequelae such as convulsions, episodic headache, autonomic disturbance, abnormal behaviour, mood disorder, intellectual deficit, paresis, incoordination of movements, jerky limb movements, speech disorder, cranial nerve palsy, gaze palsy, parkinsonian features, impaired hearing, etc.[1] An estimated 25% of affected children die from the disease, and among those who survive, 30%–40% suffer from physical and mental impairment. Children suffer the highest attack rate due to lack of cumulative immunity from natural infections.[2] JE was first recognized in Japan in 1924. Since the late 1960s, the extent of epidemics in Japan and China has steadily declined. It is estimated that 3 billion people are at risk, and the disease has spread to new territories.[3]
According to WHO, JE is endemic in large parts of the Asia and Pacific regions, especially in the South Asian and Western Pacific regions. According to WHO statistics, 3187 cases of JE were reported in 2013 from all over the world; of these, 42% were from countries in the South-East Asia region, and of these 80% were from India.[4] According to a systematic review by Campbell in 2011, India falls in the medium-to-high incidence areas with an expanding vaccination programme and shares its place with Sri Lanka, Thailand and Vietnam. The population of these endemic areas is about 538.1 million.[5] A fatality rate of 3 0%–50% has been attributed to JE in southern and eastern Asia.[6]
The first case of JE was reported in India in 1955 from Vellore, Tamil Nadu and the first major outbreak was reported in 1973 from Burdwan district of West Bengal. Since then, in India, AES and JE have been reported from 171 districts of 19 states. In India, the JE virus has been isolated from more than 15 species of mosquitos belonging to genera Culex, Aedes and Anopheles; Culex tritaeniorhynchus and Culex vishnui are considered the main vectors.[7] A major outbreak of JE was reported from eastern Uttar Pradesh (UP) during 2005 with more than 6000 cases and 1500 deaths. This led to the introduction of the JE vaccine in endemic areas. Bihar, which is adjacent to eastern UP, has also reported a rise in the number of patients with AES and JE with periodic epidemics in some districts, including Muzaffarpur district.[8]
The outbreaks of JE in Gorakhpur and Basti divisions in eastern UP during 2005, led to the development of surveillance guidelines for AES and JE by the National Vector Borne Disease Control Programme (NVBDCP). These guidelines required JE to be reported as an AES and after confirmation from the sentinel sites, a line-list of JE cases needed to be drawn and sent in prescribed formats.[9]
There is deficiency of data on AES and JE from Bihar. We aimed to ascertain the status and trends of AES and JE in Bihar to suggest measures for prevention and control.
Methods
The Bihar plain is divided into two unequal halves by the river Ganga which flows from west to east. With a population of 10.38 crore (103.8 million), 17% of the state population is in the 0–6 years age group. The literacy rate of Bihar is 63.8% and decadal growth is 25%. Bihar, consisting of 38 districts, is a complex state for healthcare services in terms of resources and accessibility.[10]
The NVBDCP follows the case definition of JE based on a syndromic approach. Epidemiological surveillance is done for AES, and suspected JE cases are reported as follows: ‘Clinically, a case of AES is defined as a person of any age, at any time of year with the acute onset of fever and a change in mental status (including symptoms such as confusion, disorientation, coma, or inability to talk) and/or new onset of seizures (excluding simple febrile seizures). Other early clinical findings may include an increase in irritability, somnolence or abnormal behaviour greater than that seen with usual febrile illness.’ Continuous surveillance of the disease is done through the Integrated Disease Surveillance Project (IDSP).[11] JE surveillance aims to identify patients with AES and subsequently confirm JE virus infection using IgM ELISA (enzyme-linked immunosorbent assay).[2] Laboratory confirmation of suspected cases of JE is done at identified sentinel laboratories, where the preferred test for diagnosis of JE is the IgM Capture ELISA. The samples are initially processed in district sentinel laboratories. Samples are then sent for confirmation to designated national laboratories.[12]
The cases are reported by health workers to district health authorities. In-charge nodal officers from the district regularly visit facilities reporting AES cases for validation of the reported data. At the state level, reports are received from the districts according to the status of the disease, i.e. daily reports during outbreaks, weekly reports during the transmission period and monthly reports in the inter-epidemic period. The districts are monitored for regular reporting. The data are then merged at the state level, collated and immediately transmitted through specified proformas.[12] We collected the monthly epidemiological data of AES and JE for the period 2009–2014. We accessed the data with permission from the state health authorities.
We estimated the trends of AES and JE cases, burden of AES and JE in terms of morbidity and mortality, annual incidence rate (number of cases per 100 000 population) and CFR (proportion of deaths against the total number of cases reported per year).
Results
A total of 4400 cases of AES were reported between 2009 and 2014, an average of 733 cases per year. There were 1309 deaths reported with an average CFR of about 3 0%. There were 396 cases of JE and 56 deaths during the study period [Table - 1]. The CFR for confirmed JE cases was about 14%.
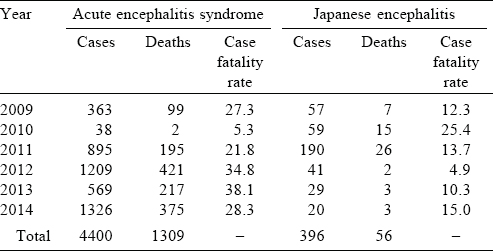
From 2009 to 2014, AES cases started to appear in April–May, reached a peak during June and declined from October [Figure - 1]. A similar pattern is seen each year. Two peaks are seen, one in June and another in September and October. The maximum number of cases and the highest peak was in 2014. The trend of JE (confirmed) cases over the years mirrored the trend in AES cases [Figure - 2].
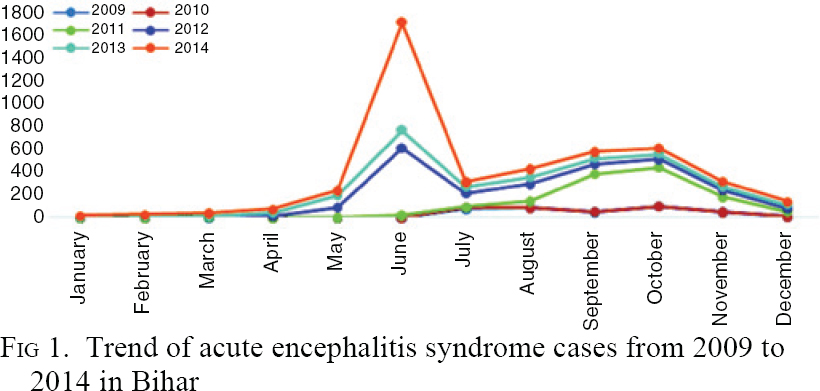 |
| Figure 1: Trend of acute encephalitis syndrome cases from 2009 to 2014 in Bihar |
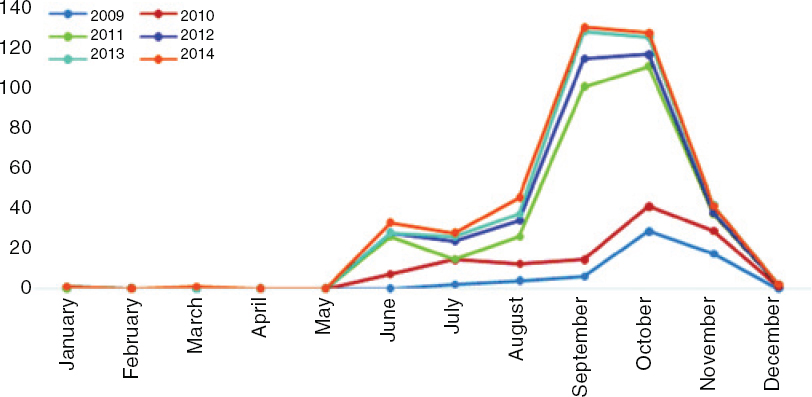 |
| Figure 2: Trend of Japanese encephalitis (confirmed) cases from 2009 to 2014 in Bihar |
The districts of Patna, Nalanda, Jehenabad, Nawada, Gaya, Aurangabad, Vaishali, Muzaffarpur, Sheohar and East Champaran had the highest annual incidence rate (4.7–25 per 100 000 population) for AES [Figure - 3]. District such as Saran, Siwan, Bhojpur, Buxar, West Champaran, Jamui and Sitamarhi had a lower annual incidence rate of 2.2 to 4.73 per 100 000 population and fall in the third quartile. Districts such as Kaimur, Darbhanga, Madhubani and others were in the first quartile and added little to the pool of AES cases.
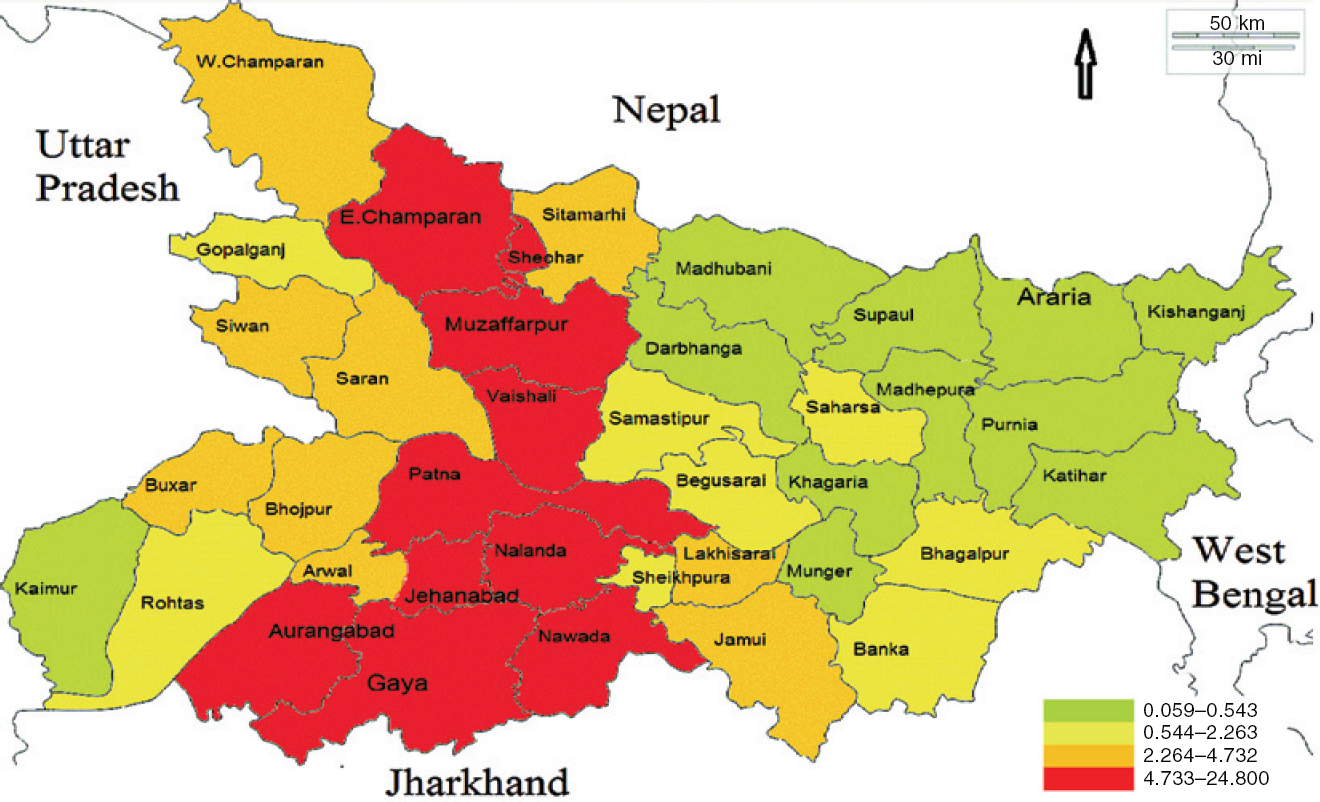 |
| Figure 3: A map showing district-wise distribution in Bihar of cases with acute encephalitis syndrome according to the annual incidence rate (per 100 000 population) |
The districts of Patna, Jehenabad, Nawada, Gaya, Lakhisarai, Gopalganj, Siwan, East Champaran and West Champaran have annual incidence rate of JE ranging from 0.546 to 1.78 per 100 000 population, which falls in the fourth quartile. Kaimur, Rohtas, Vaishali, Sheohar, Begusarai, Munger, Supaul, Araria, Purnia, Katihar and Kishanganj did not report any cases of JE. However, Aurangabad, Arwal, Bhojpur, Buxar, Saran, Nalanda, Khagaria and Banka were in the third quartile [Figure - 4].
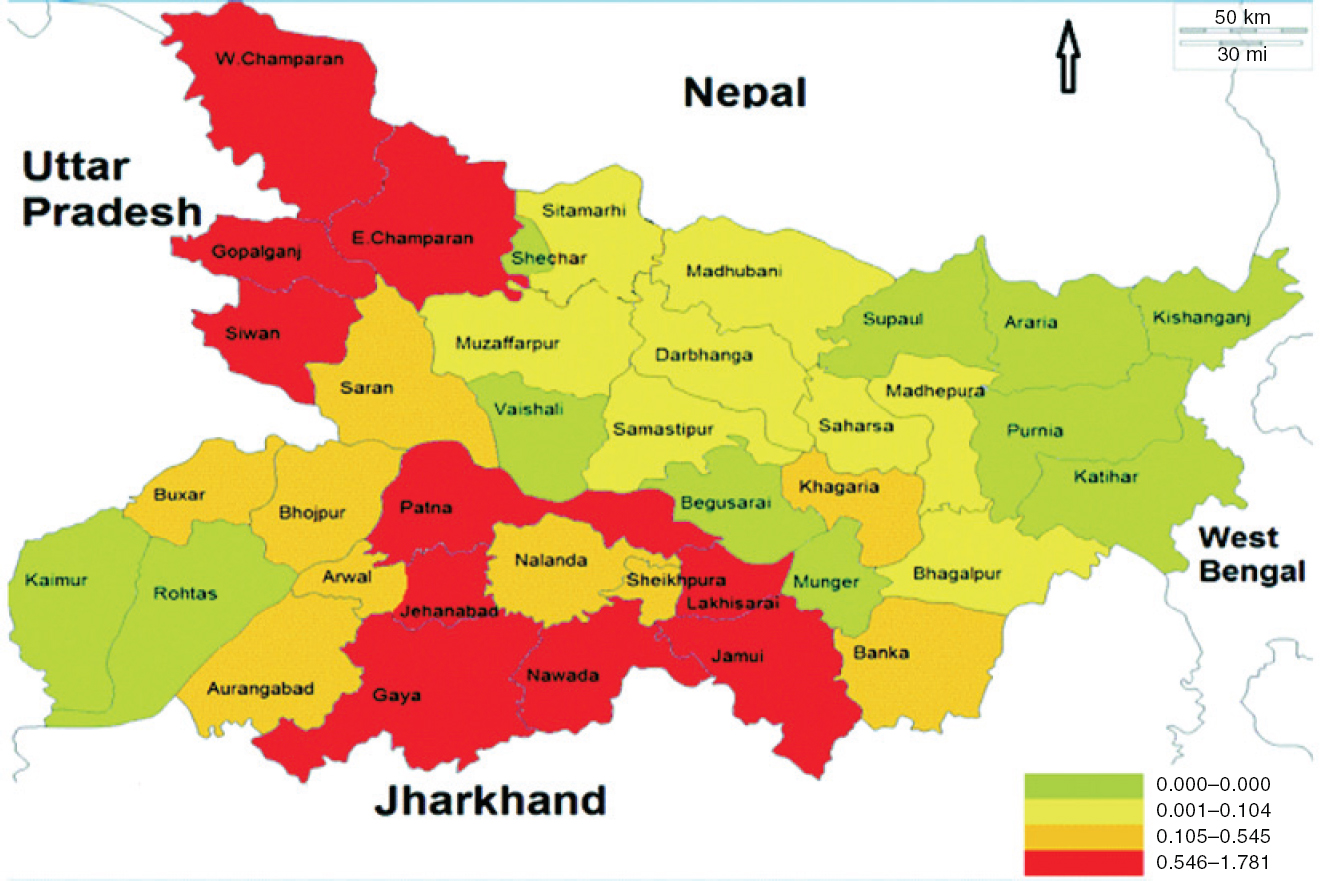 |
| Figure 4: A map showing district-wise distribution in Bihar of Japanese encephalitis (confirmed) cases according to the annual incidence rate (per 100 000 population) |
Discussion
We collected data from 2009 to 2014 and observed that year on year the reporting of AES and confirmed JE cases increased. This could be due to strengthening of the surveillance system by the NVBDCP. The average CFR was 30% in AES and 13% in confirmed cases of JE. The CFR ranged from 5.3% to 34.8% for AES. A CFR of 20%–36% was reported in another study from Bihar in 2013.[8] However, a study from UP by Kakkar et al.,[13] which analysed two years' data from a tertiary care centre found that the CFR for AES ranged from 18% to 19.8%; less than that in our study. Another study that compared CFR at different times found it to be 31.5% in 1978 during an outbreak, 34.5% in 1985 and 31.5% in 1988, and declined to 24.9% in 2005. This was possibly due to improvement in the management of cases with JE.[14] A study between 1978 and 2007 of over 100 000 AES cases showed a CFR of almost 33% from 13 different states.[15] In Nepal, which is adjoining Bihar, the overall mortality of JE varied from 9.8% in 2000 to 20.9% in 2003;[16] similar to our study.
The AES cases had a seasonal distribution—beginning in the months of April and May and peaking in June. The cases started to decline from October. A similar pattern was seen in confirmed cases of JE. Most previous studies too reported epidemics between May and October, and mostly from the northern and eastern parts of India.[17] In UP, the reported JE cases between 1998 and 2007 were sporadic in June and peaked in September before declining. Seasonal peaks of cases of JE have occurred during July to October, coinciding with the rainy and post-rainy seasons. The onset of winter brings a decline in the cases of JE.[10] In Nepal, cases of AES and JE started a little earlier, in April–May, and reached a peak during late August to early September, and then declined.[16] Saxena et al. studied the trend of AES cases and suggested that JE was increasing in northern India, which may result in larger epidemics in the future.[18] In India, Karnataka has been reported to have two epidemics each year, a severe form from April to July and a milder one from September to December along with the rest of India.[15] In Tamil Nadu, of 561 AES cases reported during a study, JE was confirmed in 4.9% with an increasing trend from 4.1% in 2007 to 5.3% in 2009.[19] The minimum reported incidence in a tropical setting for all ages was 6.34 per 100 000 population.[20] Districts of Patna, Nalanda, Jehenabad, Nawada, Gaya, Aurangabad, Vaishali, Muzaffarpur, Sheohar and East Champaran had the maximum number of cases of AES cases with an annual incidence ranging from 4.7 to 24.8 per 100 000 population. Dinesh et al.[21] and Mishra et al.[8],[22] have also reported a similar distribution of cases.
Conclusions
With all districts reporting cases of AES and JE, the disease is endemic in Bihar. The cases of AES start appearing in April and reach a peak in June and then decline. There is another peak of JE cases in October. The CFR of AES and JE ranges from 5% to 35% in Bihar. The annual incidence rate of AES ranges from 0.05 to 25 per 100 000 population with all districts reporting cases. Confirmed cases of JE have an annual incidence ranging from 0 to 2 per 100 000 population and 75% of the districts report cases of JE. The reporting and surveillance mechanism needs to be strengthened in all the districts of the state. Private practitioners who participate less in surveillance activities need to be encouraged to do so especially for cases of AES. Intense information, education and communication (IEC) activities must be started at the village level to increase participation from the community and to improve the long-term passive surveillance. Hence, there is a need to intensify efforts for prevention and control during April–June.
Conflicts of interest. None
| 1. | Baruah HC, Biswas D, Patgiri D, Mahanta J. Clinical outcome and neurological sequelae in serologically confirmed cases of Japanese encephalitis patients in Assam, India. Indian Pediatr 2002;39:1143-8. [Google Scholar] |
| 2. | Ministry of Health and Family Welfare. National Programme for Prevention and Control of Japanese Encephalitis/Acute Encephalitis Syndrome, Operational Guidelines. New Delhi:National Vector Borne Disease Control Programme, Directorate General of Health Services, Ministry of Health and Family Welfare; 2014. [Google Scholar] |
| 3. | Erlanger TE, Weiss S, Keiser J, Utzinger J, Wiedenmayer K. Past, present, and future of Japanese encephalitis. Emer Infect Dis 2009;15:1-7. [Google Scholar] |
| 4. | World Health Statistics 2015. Geneva:World Health Organization; 2015. [Google Scholar] |
| 5. | Campbell G, Hills S, Fischer M, Jacobson J, Hoke C, Hombach J, et al. Estimated global incidence of Japanese encephalitis: A systematic review. Bull World Health Organ 2011;89:766-74. [Google Scholar] |
| 6. | Tiwari S, Singh RK, Tiwari R, Dhole TN. Japanese encephalitis: A review of the Indian perspective. Braz J Infect Dis 2012;16:564-73. [Google Scholar] |
| 7. | National Institute of Virology. Japanese encephalitis. New Delhi:Indian Council of Medical Research. Available at www.icmr.nic.in/pinstitute/niv/JAPANESE%20ENCEPHALITIS.pdf (accessed on 15 Jul 2017). [Google Scholar] |
| 8. | Mishra R. Epidemiological report on acute encephalitis syndrome (AES)/Japanese encephalitis (JE) outbreak in Bihar and planning perspectives for its control. Am J Health Res 2014;2:404-10. [Google Scholar] |
| 9. | Guidelines: Clinical management of acute encephalitis syndrome including Japanese encephalitis. New Delhi:National Vector Borne Disease Control Programme, Directorate General of Health Services, Ministry of Health and Family Welfare; 2009. [Google Scholar] |
| 10. | Government of Bihar. State profile. Updated 16 Jul 2016. Available at http://gov.bih.nic.in/Profile/default.htm (accessed on 16 Jul 2016). [Google Scholar] |
| 11. | Ministry of Health and Family Welfare, Government of India. Integrated Disease Surveillance Program. New Delhi:National Centre for Disease Control, Directorate General of Health Services. Available at http://idsp.nic.in/index4.php?lang=1&level=0&linkid=313&lid=1592 (accessed on 16 Jul 2017). [Google Scholar] |
| 12. | Directorate of National Vector Borne Diseases Control Programme. Guidelines for surveillance of acute encephalitis syndrome (with special reference to Japanese encephalitis). New Delhi:National Vector Borne Diseases Control Programme, Directorate General of Health Services, Ministry of Health and Family Welfare; 2006. [Google Scholar] |
| 13. | Kakkar M, Rogawski ET, Abbas SS, Chaturvedi S, Dhole TN, Hossain SS, et al. Acute encephalitis syndrome surveillance, Kushinagar district, Uttar Pradesh, India, 2011-2012. Emerg Infect Dis 2013;19:1361-7. [Google Scholar] |
| 14. | Kumari R, Joshi PL. A review of Japanese encephalitis in Uttar Pradesh, India. WHO South-East Asia J Public Health 2012; 1:374-95. [Google Scholar] |
| 15. | Kelly R. Acute encephalitis syndrome outbreaks in India—An ongoing puzzle. Sydney : School of Public Health and Community Medicine; Oct 2014. Available at https://sphcm.med.unsw.edu.au/infectious-diseases-blog/acute-encephalitis-syndrome-outbreaks-india-%E2%80%93-ongoing-puzzle (accessed on 15 Jul 2017). [Google Scholar] |
| 16. | Bhatta LR, Wierzba T, Joshi AB, Banjara MR. Status and trend of Japanese encephalitis epidemics in Nepal: A five-year retrospective review. J Nepal Health Res Counc Dec 2008. Available at http://jnhrc.com.np/index.php/jnhrc/article/view/75 (accessed on 4 Jul 2017). [Google Scholar] |
| 17. | Joshi R, Kalantri SP, Reingold A, Colford JM. Changing landscape of acute encephalitis syndrome in India: A systematic review. Natl Med J India 2012;25: 212-20. [Google Scholar] |
| 18. | Saxena SK, Mishra N, Saxena R, Singh M, Mathur A. Trend of Japanese encephalitis in North India: Evidence from thirty-eight acute encephalitis cases and appraisal of niceties. J Infect Dev Ctries 2009;3:517-30. [Google Scholar] |
| 19. | Gunasekaran P, Kaveri K, Arunagiri K, Mohana S, Kiruba R, Kumar VS, et al. Japanese encephalitis in Tamil Nadu (2007–2009). Indian J Med Res 2012;135: 680-2. [Google Scholar] |
| 20. | Jmor F, Emsley HCA, Fischer M, Solomon T, Lewthwaite P. The incidence of acute encephalitis syndrome in western industrialised and tropical countries. Virol J 2008;5:134. [Google Scholar] |
| 21. | Dinesh DS, Pandey K, Das VNR, Topno RK, Kesari S, Kumar V, et al. Possible factors causing acute encephalitis syndrome outbreak in Bihar, India. Int J Curr Microbiol App Sci 2013;2:531-8. [Google Scholar] |
| 22. | Mishra R. Annual communicable disease surveillance report 2013, Bihar. Patna:Integrated disease surveillance project, State health society, Bihar; 2013. [Google Scholar] |
Fulltext Views
6,218
PDF downloads
2,687




