Translate this page into:
Surgery for benign prostatic hyperplasia: Profile of patients in a tertiary care institution
2 Department of Surgery, University of Minnesota, Minnesota, USA
3 Department of Urology, All India Institute of Medical Sciences, Ansari Nagar, New Delhi 110029, India
Corresponding Author:
Rajeev Kumar
Department of Urology, All India Institute of Medical Sciences, Ansari Nagar, New Delhi 110029
India
rajeev02@gmail.com
| How to cite this article: Rajeev R, Giri B, Choudhary LP, Kumar R. Surgery for benign prostatic hyperplasia: Profile of patients in a tertiary care institution. Natl Med J India 2017;30:7-10 |
Abstract
Background. Medical therapy is widely used for managing benign prostatic hyperplasia (BPH) and has made an impact on the profile of patients who ultimately undergo surgery. This changing profile may impact outcomes of surgery and associated complications. To assess the impact of medical management, we evaluated the profile of patients who had surgery for BPH at our institution.
Methods. A retrospective chart-review was performed of patient demographics, indications for surgery, preoperative comorbid conditions and postoperative course in patients who underwent surgery for BPH over a 5-year period. The data were analysed for demographic trends in comparison with historical cohorts.
Results. A total of 327 patients underwent surgery for BPH between 2008 and 2012. Their mean age was 66.4 years, the mean prostate gland weight was 59.2 g and the mean duration of symptoms was 35.3 months; 34% had a prostate gland weight of >60 g; 1 59 (48.6%) patients had an absolute indication for surgery; 139 (42.5%) of these were catheterized and 6.1% of patients presented with azotaemia or upper tract changes without urinary retention.
Conclusions. In comparison with historical cohorts, more patients are undergoing surgery for absolute indications including retention of urine and hydroureteronephrosis. However, the patients are younger, they have fewer comorbid conditions and have a similar rate of complications after the procedure.
Introduction
Benign prostatic hyperplasia (BPH) is a clinical condition characterized by lower urinary tract symptoms (LUTS) in men. This condition is of public health importance because half of all men over 50 years of age have pathological BPH, and the presence of LUTS among Asian men ranges from 18% in the 40–49 years age group to over 50% in the 70–79 years age group.[1],[2]
Alpha-adrenergic receptor blockers (AARBs) and 5α-reductase enzyme inhibitors (5-ARI) are the mainstay of initial management of BPH. Medical management has led to improvement in symptoms with reduced incidence of acute urinary retention (AUR) and need for surgery.[3],[4] The current indications for surgery are refractory urinary retention, renal insufficiency or hydroureteronephrosis (HDUN) secondary to BPH, progressive symptoms while on medical management, persistent haematuria, recurrent urinary tract infections (UTIs), bladder stones and diverticuli. The increasing use of medical management has changed the profile of patient undergoing surgery for BPH. Studies from Korea and Canada have described a change in patient demographics and associated complications due to medical therapy for BPH.[5],[6]
We hypothesized that the increasing use of medical therapy for managing LUTS in the Indian population would lead to a larger number of patients presenting with complications of BPH or with increased comorbid conditions. This could impact treatment strategies and patient outcomes. We therefore determined the profile of patients who undergo surgery for BPH at our institution and assessed possible implications.
Methods
Case records of consecutive patients who underwent surgery for BPH at our tertiary care centre between 1 January 2008 and 31 December 2012 were retrieved. Data from these records were manually extracted and entered in a pre-designed proforma. Information on patient demographics, comorbid conditions, medical therapy, prostate size, imaging findings, indications of surgery, type of surgical procedures, and in-hospital and postoperative course were extracted.
Medical therapy was recorded as AARB, 5-ARI, combination therapy or herbal supplements. Medical therapy given only after the first episode of retention of urine but discontinued due to a failed trial without catheter (TWOC) was recorded as ‘no medical therapy’. Comorbid conditions recorded included diabetes mellitus (DM), hypertension, chronic obstructive pulmonary disease (COPD), coronary artery disease (CAD) and asthma. Any other comorbid condition was classified as ‘Other’. Patients who underwent any concomitant surgery were excluded from the study.
AUR was defined as history of acute painful retention of urine and less than 12 weeks of bladder catheterization at the time of surgery. Patients with a history of AUR and at least one episode of failed TWOC were classified as refractory retention. Chronic urinary retention (CUR) was defined as patients presenting with a post-void residual volume (PVR) >300 ml if voiding spontaneously. Upper tract changes were defined as patients with HDUN on ultrasound and normal preoperative urea and creatinine levels. Obstructive uropathy was defined as HDUN on ultrasound with preoperative urea >40 mg/dl or creatinine >2 mg/dl. Patients with >2 episodes of haematuria were defined as ‘recurrent haematuria’. Failure of medical therapy was a diagnosis of exclusion and was defined as patients who elected for surgery despite being on medical management but with none of the other indications for surgery. Serum sodium level <130 mEq/L or >150 mEq/L and serum potassium levels <3mEq/L or >6 mEq/L were labelled as dyselectrolytaemia.
Statistical analysis was done using Stata/IC 12.1 (StataCorp LP, College Station, Texas). Chi-square test was used to compare categorical variables. All p values are 2-sided and p value ≤0.05 was considered statistically significant.
Results
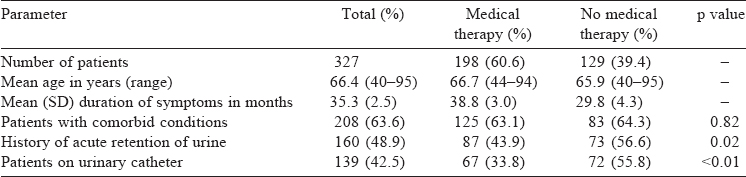
A total of 327 patients’ records were reviewed during the study [Table - 1]. The median age for patients who underwent surgery was 66.8 years with a mean duration of symptoms of 35.3 months. Two hundred and eight (63.6%) patients had at least one comorbid condition and 60.6% of patients had received prior medical therapy. This was significantly lower among patients who had an episode of AUR or were on a catheter at the time of surgery. Of the 198 patients who received medical therapy, AARB were the most commonly prescribed medications with 186 patients (56.8%) having taken them whereas 49 patients (14.1%) were taking 5-ARIs. Thirty-nine patients (11.9%) took a combination of these drugs while 8 patients (2.4%) had taken herbal and alternative medicines.
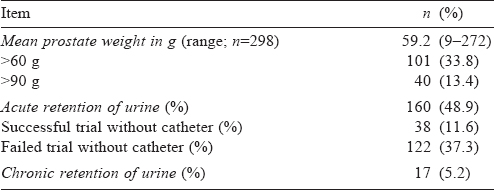
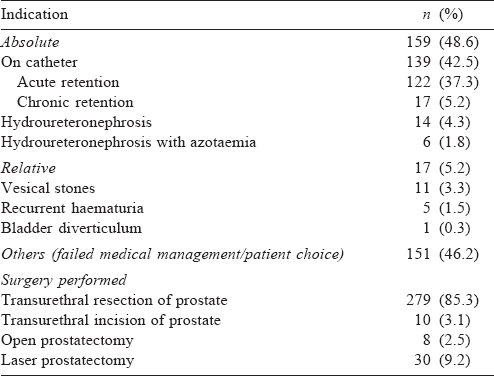
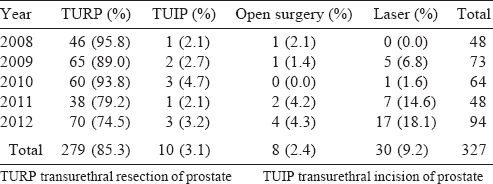
The mean weight of the prostate was 59.2 g (range 9–272) in the 298 patients for whom the data were available [Table - 2]. One hundred and seventy-seven patients (54.2%) had a history of urine retention and 159 (48.6%) had an absolute indication for surgery [Table - 3]. This included 139 (42.5%) patients who were on a catheter (122 AUR, failed TWOC; 17 CUR) and 20 (6.1%) with azotaemia or upper tract changes but who did not have urinary retention. Another 5.2% had relative indications including bladder stones, diverticuli and recurrent haematuria; 46.2% underwent surgery either due to failure of medical management (progressive or unresolved symptoms) or personal choice. Four kinds of procedures were done: transurethral resection of prostate (TURP) was the most common procedure (85.3%) followed by green light laser prostatectomy (LP) [9.2%; Table 3]. The number of laser procedures increased over the 5 years of the study period [Table - 4].
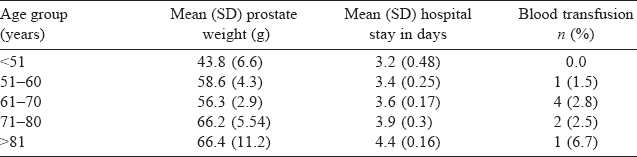
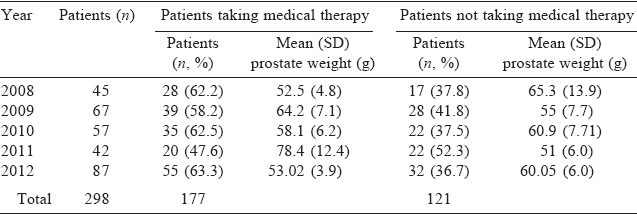
Eight patients (2.4%) required postoperative blood transfusions and 13 (3.9%) had dyselectrolytaemia. None of these progressed to a TURP syndrome. Postoperative complications were more in the no-medical therapy group (dyselectrolytaemia 5.4%, transfusion 3.9%) than the medical therapy group (3.0% and 1.5%, respectively). However, prostate weight, hospital stay and need for transfusion showed a linear increase with increase in age [Table - 5]. The time-trends of prostate weight over the 5 years in relation to use of medical management are given in [Table - 6].
Discussion
Historically, TURP has seen marked improvement in mortality rate s from 2.5% in the 1960s to almost 0.1% at present, though the morbidity rates have remained unchanged at 17%–25%.[7] Combination medical therapy has been convincingly shown to reduce the risk of AUR and the need for invasive therapy in patients with symptomatic BPH.[4] However, the change in clinical profile of patients presenting for surgery after prolonged medical management and subsequent failure of treatment is not well characterized.
In our study, patients were younger with fewer or similar comorbid conditions as compared to the large cohorts of Mebust et al. and Reich et al.[8],[9] In fact, <2% of our patients were older than 85 years compared to 14.5% in the study by Reich et al. in 2008.[9] Age has an impact on the surgical procedure and its outcomes. Post-TURP catheter dependence is higher in patients above 85 years of age and these patients are at an increased risk of incontinence.[10],[11],[12] Our data show that as the age at surgery increased, prostate volume, postoperative hospital stay and rate of blood transfusion increased proportionately. A retrospective single institution study from Spain showed that the mean age of patients undergoing TURP in 2002 compared to 1992 increased by an average of 3.1 years without any significant increase in comorbid conditions or postoperative complications.[13] Similar studies have either shown no or slight change in the age at presentation for surgery with no significant increase in post-procedure complications and morbidity.[14],[15] Our data showing a lower age at surgery could be reflective of two social trends in India. First, patients may be seeking surgery earlier due to the costs associated with medical management. Only 61% of our patients had received medical management before surgery and since our report comes from a public institution catering to the financially poorer strata of society, financial implications may be driving patients to surgery. Second, life expectancy in India is lower than that in western populations and perhaps accounts for a lower number of octogenarians in our series.
Consistent with our finding of lower age at surgery, we noted fewer comorbid conditions among our patients than those reported in the literature. Just over one-third (36%) of our patients had no comorbid conditions compared with only 24% in the series of Mebust et al.[8] In a study of similar design, Borboroglu et al.[15] evaluated 520 consecutive patients who had undergone surgery for BPH from a single centre in 1999. They reported that only 30% of patients had two or more comorbid conditions, similar to our 27.2%.
It has been suggested that the proportion of patients presenting with AUR and CUR have almost doubled in the past two decades.[6] In our study, more than half the patients had a ‘classical’ absolute indication for surgery (retention, upper renal tract changes or complications). In contrast, the study by Mebust et al. had only 27% of patients with AUR but almost 12% each with recurrent infections and haematuria.[8] Both these indications were uncommon in our cohort, possibly due to early treatment in the community before presentation to us. This is an important finding, consistent with our hypothesis of delayed presentation. Urinary retention results in emergency hospital visits, the need for catheterization and its attendant complications, infection and potential renal deterioration. Armitage et al. reported a higher 1-year mortality in men with spontaneous AUR admitted for BPH in the UK during 1998–2002.[16] This effect is further enhanced by increasing age (75–84 years old) and presence of comorbid conditions. They found a 12.5% 1-year mortality rate in patients without comorbid conditions and 28.8% in those with comorbid conditions in the age group of 75–84 years. In a retrospective study of Taiwanese population involving 4367 patients with and without preoperative AUR, the mean length of hospital stay was longer in patients with AUR at 6.4 days (n=3305 patients) versus patients without AUR at 4.2 days (n=1062, p<0.001). Similarly, there was a higher rate ofre-catheterization in patients with AUR, higher medical expenses during hospitalization and a higher rate of blood transfusion.[17]
Our data also show a trend towards higher early complications in patients with increasing age and comorbid conditions. However, we also found that patients who presented with urinary retention were less likely to have received medical management, suggesting that medical management is not the reason for the late presentation. On the contrary, this may actually argue in favour of medical management and this finding may simply be a reflection of the fact that our patients typically present late.
Although TURP continues to be the preferred surgical option, 9.2% of procedures were performed using a laser, particularly in recent years [Table - 6]. This trend reflects the global scenario where lasers replaced almost 50% of TURP over the past decade in the USA.[18] The introduction of lasers, both holmium and green light, has created a choice about the type of surgery offered to patients. Prostate size is used as one of the selection criteria and TURP is often considered suitable only for glands of weight <60 g, or at most 90 g. In our series, 101 patients (34%) had a gland weight of >60 g and 40 (13%) >90 g. However, none of them underwent laser prostatectomy. Only 1 patient who underwent laser surgery had a gland weight of >60 g and open surgery was required for only 8 patients. These data suggest that selecting lasers purely on the basis of gland weight may not be appropriate.
Our study has a number of limitations. This is a retrospective collection of data and a number of data-points may not have been accurately recorded in the case sheets. There is also likely to be a selection bias since the data are from a public-funded tertiary care hospital, not necessarily representative of the general population. Complication data are restricted to in-hospital records and long-term complications were not included. Despite these limitations, the data reflect the reality of surgical management for BPH today.
Conclusion
Our data show that surgery for BPH is being done more frequently for absolute indications such as urinary retention. Patients who present with urinary retention are less likely to have received medical therapy. TURP is the most common procedure with wide application in prostate gland irrespective of weights. Despite the use of medical management, the age at surgery has not increased and there is no increase in the number of comorbid conditions or complications suffered by these patients.
| 1. | Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol 1984;132:474–9. [Google Scholar] |
| 2. | Homma Y, Kawabe K, Tsukamoto T, Yamanaka H, Okada K, Okajima E, et al. Epidemiologic survey of lower urinary tract symptoms in Asia and Australia using the international prostate symptom score. Int J Urol 1997;4:40–6. [Google Scholar] |
| 3. | Roehrborn CG, Boyle P, Nickel JC, Hoefner K, Andriole G, ARIA3001 ARIA3002 and ARIA3003 Study Investigators. Efficacy and safety of a dual inhibitor of 5-alpha-reductase types 1 and 2 (dutasteride) in men with benign prostatic hyperplasia. Urology 2002;60:434–41. [Google Scholar] |
| 4. | McConnell JD, Roehrborn CG, Bautista OM, Andriole GL Jr, Dixon CM, Kusek JW, et al. Medical Therapy of Prostatic Symptoms (MTOPS) Research Group. The long-term effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia. N Engl J Med 2003;349:2387–98. [Google Scholar] |
| 5. | Choi SY, Kim TH, Myung SC, Moon YT, Kim KD, Kim YS, et al. Impact of changing trends in medical therapy on surgery for benign prostatic hyperplasia over two decades. Korean J Urol 2012;53:23–8. [Google Scholar] |
| 6. | Izard J, Nickel JC. Impact of medical therapy on transurethral resection of the prostate: Two decades of change. BJU Int 2011;108:89–93. [Google Scholar] |
| 7. | Uchida T, Ohori M, Soh S, Sato T, Iwamura M, Ao T, et al. Factors influencing morbidity in patients undergoing transurethral resection of the prostate. Urology 1999;53:98–105. [Google Scholar] |
| 8. | Mebust WK, Holtgrewe HL, Cockett AT, Peters PC. Transurethral prostatectomy: Immediate and postoperative complications. A cooperative study of 13 participating institutions evaluating 3,885 patients. J Urol 1989;141:243–7. [Google Scholar] |
| 9. | Reich O, Gratzke C, Bachmann A, Seitz M, Schlenker B, Hermanek P, et al. Urology Section of the Bavarian Working Group for Quality Assurance. Morbidity, mortality and early outcome of transurethral resection of the prostate: A prospective multicenter evaluation of 10,654 patients. J Urol 2008;180:246–9. [Google Scholar] |
| 10. | Dubey D, Kumar A, Kapoor R, Srivastava A, Mandhani A. Acute urinary retention: Defining the need and timing for pressure-flow studies. BJU Int 2001;88:178–82. [Google Scholar] |
| 11. | Hakenberg OW, Pinnock CB, Marshall VR. Preoperative urodynamic and symptom evaluation of patients undergoing transurethral prostatectomy: Analysis of variables relevant for outcome. BJU Int 2003;91:375–9. [Google Scholar] |
| 12. | Losco G, Mark S, Jowitt S. Transurethral prostate resection for urinary retention: Does age affect outcome? ANZ J Surg 2013;83:243–5. [Google Scholar] |
| 13. | Vela-Navarrete R, Gonzalez-Enguita C, Garcia-Cardoso JV, Manzarbeitia F, Sarasa- Corral JL, Granizo JJ. The impact of medical therapy on surgery for benign prostatic hyperplasia: A study comparing changes in a decade (1992-2002). BJU Int 2005;96:1045–8. [Google Scholar] |
| 14. | Wendt-Nordahl G, Bucher B, Häcker A, Knoll T, Alken P, Michel MS. Improvement in mortality and morbidity in transurethral resection of the prostate over 17 years in a single center. J Endourol 2007;21:1081–7. [Google Scholar] |
| 15. | Borboroglu PG, Kane CJ, Ward JF, Roberts JL, Sands JP. Immediate and postoperative complications of transurethral prostatectomy in the 1990s. J Urol 1999;162: 1307–10. [Google Scholar] |
| 16. | Armitage JN, Sibanda N, Cathcart PJ, Emberton M, van der Meulen JH. Mortality in men admitted to hospital with acute urinary retention: Database analysis. BMJ 2007;335:1199–202. [Google Scholar] |
| 17. | Chen JS, Chang CH, Yang WH, Kao YH. Acute urinary retention increases the risk of complications after transurethral resection of the prostate: A population-based study. BJU Int 2012; 110: E896–E901. [Google Scholar] |
| 18. | Schroeck FR, Hollingsworth JM, Kaufman SR, Hollenbeck BK, Wei JT. Population based trends in the surgical treatment of benign prostatic hyperplasia. J Urol 2012;188:–41. [Google Scholar] |
Fulltext Views
2,460
PDF downloads
1,526




