Translate this page into:
The undergraduate virtual grand teaching ward round: Perceptions from the subcontinent
Correspondence to THUSHAN GOONERATNE; thushan@srg.cmb.ac.lk
[To cite: Gooneratne T, Wijeyaratne M. The undergraduate virtual grand teaching ward round: Perceptions from the subcontinent. Natl Med J India 2024;37:32–4. DOI: 10.25259/NMJI_429_2022]
Abstract
Background
Grand ward rounds are an integral component of undergraduate medical education. Covid-19 prevented the conduct of conventional grand ward rounds (CWRs) prompting a ‘virtual’ grand ward round (VWR). With restrictions lifted should future grand ward rounds remain virtual? Undergraduate perceptions on the two formats were sought to explore the feasibility of the VWR as a teaching ward round for medical students.
Methods
Our study was done during April 2021 to April 2022. The weekly grand ward round was converted to a VWR during April–November 2021. Following lifting of restrictions, it was reverted to a CWR. All patients provided informed consent. A Zoom-based, secure, online platform was created with the use of smartphones to share audiovisuals and patient discussions. An online anonymised feedback survey was conducted for undergraduates during both VWR and CWR phases.
Results
The response rate was 71% (182/258). VWR was considered more advantageous than the CWR in terms of time efficiency (p=0.03), space restrictions (p=0.01), improved audibility (p=0.02) and better opportunity to engage in discussions (p=0.1). Most students (80%) felt that the VWR provides a more ‘ideal’ grand ward. Overall preference was towards VWR across safety (92%), efficacy (72%), communication (85%), information availability (84%) and training opportunity (73%). Again 80% of students preferred future ward rounds to be virtual.
Conclusions
VWR is an innovative approach. While not a substitute for bedside teaching it appears safer, efficient, thought/discussion-provoking and more satisfactory. Successful elements of the VWR can be adopted in future, to develop a more ideal undergraduate grand ward round.
INTRODUCTION
The clinical grand ward round is considered the zenith of clinical ward-based education with the participation of many experts in the field with sharing of knowledge and expertise.1 It is an opportunity to see first-hand, how a ‘team’ handles the patient and uses evidence-based, best practice to tailor a management plan that suits that ‘individual’ patient. It is also an opportunity for trainees to present to a forum, share opinions and observe ‘soft skills’.2
The grand round or the teaching ward round, however, has encountered many criticisms over the years. The gradual departure from a patient-centred process to a more service-driven, discharge focused, entity has seen a decline in its educational value. Lack of time owing to the increasing work load, too many participants and poor preparation have been key contributors to the demise of an ‘educational’ grand round.3,4
The past decade has seen medical educationists working hard to transform pedagogy and adopting new teaching strategies.5 Tools such as clinical skills laboratories, small group discussions, clinical lecture demonstrations, and problem-based learnings were adopted to facilitate active and self-directed learning.6 However, clinical learning remains in essence a bedside learning process.
The emergence of Covid-19 resulted in further unprecedented challenges. While lecture room-based teaching was more easily transferred to an online format, this was challenging in clinical teaching. Medical institutions embraced new technology. Imperial College London used a Holo Lens headset worn by a physician carrying out the ward round, with an entire cohort of medical students watching the ward round remotely.7 Augmented reality in clinical teaching and virtual ward rounds become a ‘fad’ in the modern educational institute, with much of the curriculum being transformed into an online format.8,9
Despite limitations in resources and technology our institution too commenced a virtual grand ward round (VWR) format. The use of technology for undergraduate bedside teaching has not been previously described in the region. With easing of Covid-19 restrictions, the VWR reverted to the conventional format, and allowed us to compare the conventional and virtual formats, post-Covid, to better understand the perception of undergraduates. Our study aims to draw light on how the future undergraduate teaching ward round in Sri Lanka may evolve.
METHODS
We did this observational comparative study during April 2021 and April 2022 between the VWR and conventional ward round (CWR). The weekly CWR was converted to a VWR for 6 months during April–November 2021. With lifting of restrictions of social distancing ward rounds were reverted to the CWR in November 2021.
The VWR was conducted via a Zoom-based platform. Patients provided informed consent before being included in the VWR. The minimum number of participants took part in the VWR; on average 4–6 participants (1 postgraduate trainee, 1 nurse, 1 healthcare assistant and 2 medical students). Principles of infection control were adhered to with social distancing practices and use of personal protective equipment. One member carrying a smartphone shared audiovisuals of patients while another member presented patient information to the remote audience towards the clinical discussion. Information relevant to the patient that was being discussed (i.e. images of CT scans, duplex scans, images of wounds) were shared using the ‘screen share’ function. There was an opportunity for all the participants to engage in discussions, critique and devise a management plan for each patient. The ‘Chat’ function was also enabled to allow anyone to raise questions.
An online anonymous feedback survey was conducted at the end of the appointment on expectations/objectives of the ward round, strengths and weaknesses of the ward round, critique or suggestions towards improving the grand ward round, and opinion on the future of the grand ward round. The questionnaire was based on both open-ended questions and Likert scales. Local institutional ethical approval was obtained (AAJ/ETH/COM/2021/09). Statistical analysis was performed using SPSS 21.0
RESULTS
We received 258 unique responses over the 12-month period, with a response rate of 71% (132 for VWR and 126 for CWR).
Participants opinion on the ‘ideal’ grand ward round was that it should provide a holistic approach to patient management (76%), ensure best-practice of evidence-based patient management (89%), maintain emphasis on enhancing trainee education (85%), aim to enrich knowledge (90%) and soft skills (65%), provide an environment conducive for active participation of students (90%) and should stimulate learning (58%); 82% v. 56% felt that the VWR provided a more ‘ideal’ grand ward round (p=0.02).
On a thematic analysis, four potential themes were identified— safety, efficacy, communication opportunity and training opportunity.
Almost all participants recorded that the VWR was superior to CWR in terms of safety (92%). ‘Ability to maintain social distancing’, ‘including the minimum number of participants required for the ward round purpose’ were cited as the reasons for safety.
On the theme of ‘efficacy of ward round’, VWR was considered more ‘efficacious’ by 72% of the participants. It was more advantageous in terms of mean duration of ward round (132 v. 186 minutes; p=0.03), absence from restrictions/limitations of space (83% v. 46%, p=0.003) and for better physical comfort (85% v. 55%, p=0.02). In comparison, CWR was deemed more advantageous due to lack of disruptions from network failures (0% v. 34%, p=0.0001).
The theme of communication was considered an important aspect of the ward round. In terms of being able to clearly listen to the ongoing discussions, as well as students being able to communicate their issues to the forum. Improved audibility/clarity of discussions (86% v. 55%, p=0.02), better opportunity to engage in discussions and ask questions/clarifications (62% v. 46%, p=0.01)) were advantages of the VWR in comparison to the CWR. Availability of the ‘Chat’ function was felt to be a useful tool for communication.
With regard to training opportunity, a more student-friendly environment to openly interact and engage in discussions (75% v. 65%, p=0.08) was noted in the VWR format. When compared to the VWR, the CWR was considered more suitable due to ability to review the patient physically to elicit clinical signs (76% v. 34%, p=0.002), and the physical experience of the grand ward round (23% v. 0%, p=0.002; Fig. 1).
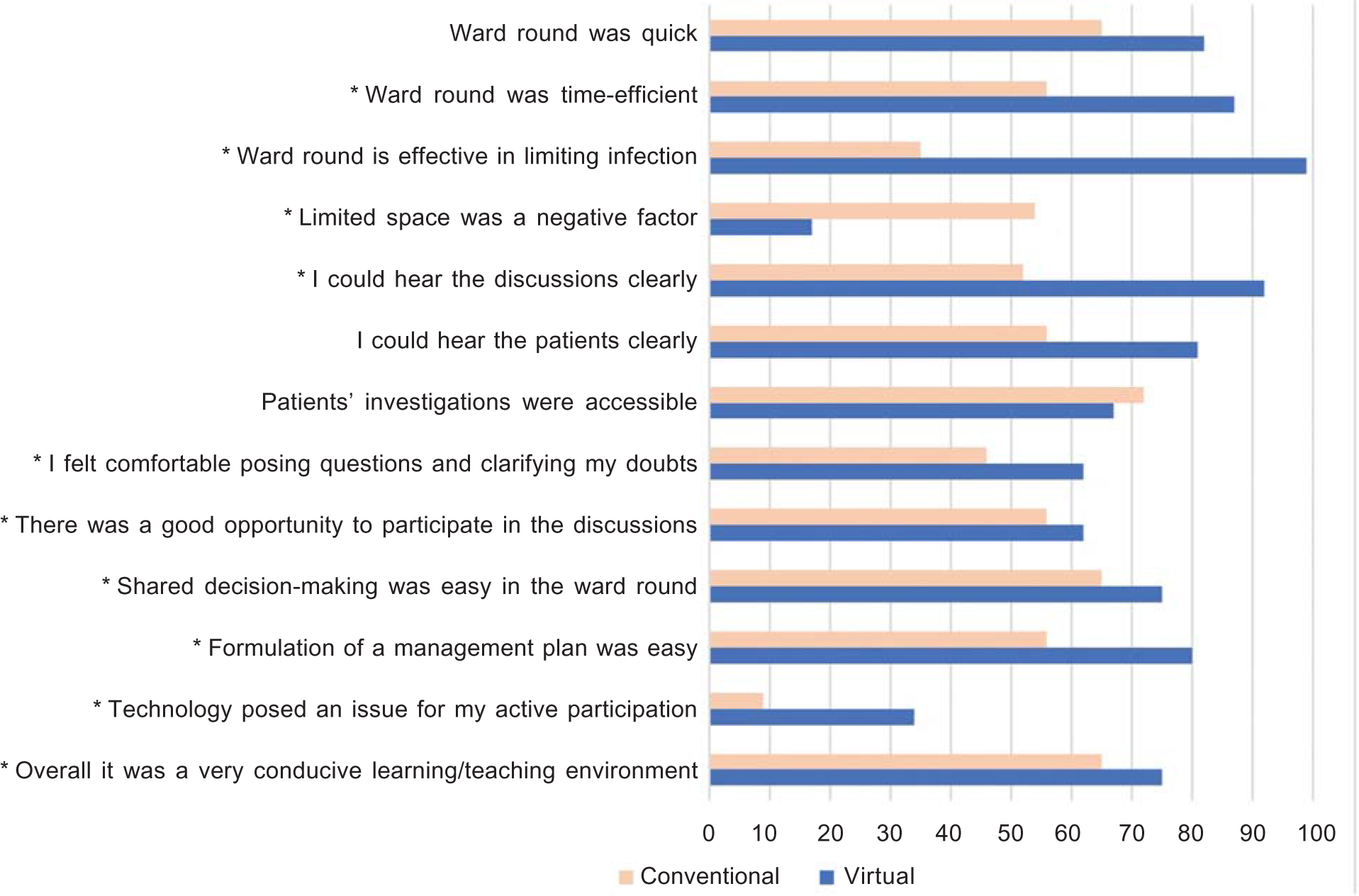
- Agreement to respective questions with 0%=Not agreeing; 100%=fully agreeing * Indicates p<0.05 on Mann– Whitney U test
Survey results showed a preference towards VWR over CWR across domains of safety (92%), efficacy (72%), communication (85%), information availability (84%), training opportunity (73%); 80% preferred VWR in the future.
DISCUSSION
Covid-19 created a major challenge to the delivery of health services. Yet, university units/teaching hospitals have the added responsibility of ensuring that undergraduate training is not compromised owing to below-par clinical exposure and supervision.10 Despite a gradual transformation of clinical teaching worldwide, South Asia has been slow to embrace technology and augmented reality in undergraduate teaching. In Sri Lanka, it was the advent of Covid-19 that necessitated a change of practice. With return to normalcy, we analysed the perception of undergraduates on the VWR and CWR to understand the dynamics of future undergraduate ward-based clinical teaching.
The VWR was quickly embraced by clinical hungry students. Study participants found the virtual format more advantageous. Space, visibility and hearing distance were no longer an issue. There was better and uniform visibility/audibility. The VWR was felt to provide a better more teaching/learning supportive environment. Our study findings were similar to previous studies by Schwartzstein et al. and Mill et al.11,12
There were initial concerns that technology and access to smart devices may lead to difficulties for medical students. Use of technology in undergraduate clinical teaching has been impacted negatively by a steep learning curve, hardware costs and unreliable Wi-fi connectivity.12 However, <30% of participants considered technology as an important detriment to the VWR. Mobile interfaces used in our VWR format are much more familiar to undergraduates compared to technology such as Holo Lens and may explain the difference.
The virtual format also brought in new dimensions that were not anticipated. Student involvement was greater in the virtual format, with more students posing questions and taking part in discussions. In the absence of an overwhelming physical presence the availability of the ‘chat function’ provided students, who were reluctant to speak, a more comfortable avenue. Student feedback highlighted the non-threatening nature of the virtual environment, feeling less ‘vulnerable’ in the online format, the availability of the chat function to pose questions, ability to pose questions while the discussions were ongoing without disturbing current conversations were helpful in this regard.
Important suggestions were made. Trainee/participant controlling the smartphone device needed to be extra cautious in the movements of the camera to avoid ‘motion sickness’. There were moments when more than one person took part in the discussions simultaneously. Adequate pre-ward round preparation is required to streamline the VWR to ensure that the time-frame is maintained and to avoid screen fatigue. Patient images and investigations could be prepared in advance and shared, rather than using the camera to ‘show’ them at the time of the ward round. Post-session summary and feedback could be introduced to reinforce key messages and learning points. There were suggestions to record the ward rounds and formulate a library for future references. The VWR could be made available for a wider audience, i.e. students from different institutes, postgraduates, etc. Local and regional specialists could be invited to the VWR to create a broader engaging discussion. However, issues regarding privacy and patient confidentiality will need to be addressed with such modifications.
Our results should be viewed considering certain limitations. Undergraduate student groups change weekly, therefore different study populations over a 12-month period have been included for comparison. Further, the VWR was introduced following months of Covid pandemic restrictions, therefore opinions on the VWR may be confounded by cognitive bias.
Nevertheless, the VWR is an innovative approach and future wards rounds could very likely be a new model that captures advantages of both formats. While not a substitute for bedside teaching, it appears safer, time-efficient and may provide a more conducive learning/teaching environment for discussions. Advantages of the CWR need to be retained, but the study results support the move to step outside the limited box of the ward and to engage a wider audience for knowledge sharing. Thanks to Covid-19, the evolution of the teaching ward round has finally reached Sri Lanka. Important lessons learnt during this period will allow the clinical teacher to better transform the undergraduate clinical ward round nearer to the ideal ward round in the future.
Conflicts of interest
None declared
References
- What is the educational value of ward rounds? A learner and teacher perspective. Clin Med (Lond). 2011;11:558-62.
- [CrossRef] [PubMed] [Google Scholar]
- Achieving high standards of training. Clin Med (Lond). 2009;9:514.
- [CrossRef] [PubMed] [Google Scholar]
- Exploring reasoning mechanisms in ward rounds: A critical realist multiple case study. BMC Health Serv Res. 2018;18:643.
- [CrossRef] [PubMed] [Google Scholar]
- The strategic use of lecture recordings to facilitate an active and self-directed learning approach. BMC Med Educ. 2016;16:201.
- [CrossRef] [PubMed] [Google Scholar]
- Modern techniques of teaching and learning in medical education: A descriptive literature review. Med Ed Publish. 2021;10:1-14.
- [CrossRef] [PubMed] [Google Scholar]
- The mixed reality medical ward round with the MS Holo Lens 2: Innovation in reducing COVID-19 transmission and PPE usage. Future Healthc J. 2021;8:e127-e130.
- [CrossRef] [PubMed] [Google Scholar]
- Augmented reality in medical education: Students' experiences and learning outcomes. Med Educ Online. 2021;26:1953953.
- [CrossRef] [PubMed] [Google Scholar]
- Augmented reality in medical education: A systematic review. Can Med Educ J. 2020;11:e81-e96.
- [CrossRef] [Google Scholar]
- Conference didactic planning and structure: An evidence-based guide to best practices from the Council of Emergency Medicine Residency Directors. West J Emerg Med. 2020;21:999-1007. Erratum in West J Emerg Med 2020;21:1287
- [CrossRef] [Google Scholar]
- Saying goodbye to lectures in medical school--paradigm shift or passing fad? N Engl J Med. 2017;377:605-7.
- [CrossRef] [PubMed] [Google Scholar]
- Live streaming ward rounds using wearable technology to teach medical students: A pilot study. BMJ Simul Technol Enhanc Learn. 2021;7:494-500.
- [CrossRef] [PubMed] [Google Scholar]




