Translate this page into:
Typhoid appendicitis and ‘the man from Istanbul’
Correspondence to SANJAY A. PAI; sanjayapai@gmail.com
To cite: Mendos A, Pai SA. Typhoid appendicitis and ‘the man from Istanbul’. Natl Med J India 2021;34:341–2.
Abstract
We describe typhoid appendicitis in a 19-year-old girl. The appendix showed aggregates of macrophages in the mucosa and in the wall. Blood culture yielded Salmonella enterica serovar Typhi. The presence of macrophages in an appendicectomy specimen should prompt the pathologist to consider the possibility of typhoid fever, even in the absence of supporting microbiological investigations.
INTRODUCTION
The legendary pathologist Dr Juan Rosai used to refer to his mentor, the equally legendary Dr Lauren Ackerman and his illustrative anecdote on ‘the man from Istanbul’. In it, he touches on the fact that just as one may not recognize a familiar face in unfamiliar settings, pathologists sometimes fail to recognize common entities in uncommon clinical settings.1 We present one such example, that of typhoid appendicitis.
THE CASE
A 19-year-old girl presented with fever, abdominal pain and constipation. Physical examination revealed distension and vague diffuse tenderness of the abdomen. Abdominal ultrasonography showed a dilated appendix, peri-appendiceal fat inflammation and mildly dilated distal ileal loops, suggestive of subacute small bowel obstruction. Laboratory investigations showed mild anaemia, leucopenia and thrombocytopenia.
At laparoscopy, there was moderate straw-coloured ascites. The mid-ileal segments were dilated and there was no obvious perforation. The appendix was tortuous and inflamed. An appendicectomy was done and the patient was started on intravenous meropenem. The contents of the appendix were not sent for culture studies. Microscopy showed aggregates of macrophage–monocytes in the mucosa and in the wall (Figs 1 and 2). The macrophages did not exhibit erythrophagocytosis. The wall of the appendix also contained lymphoid aggregates. Germinal centres were present but were not unusually prominent. There were no epithelioid granulomas and practically no eosinophils or neutrophils in the wall of the appendix. The lumen contained aggregates of neutrophils. We were unable to classify the lesion and hence, looked up the medical records for further clinical information. We learnt that a rapid indirect solid-phase immunochromatographic assay (Typhidot IgG/IgM) test done elsewhere was positive and that a blood culture (collected just before appendicectomy) had yielded S. enterica subsp. enterica ser. Typhi at 21 hours of incubation. The organism was sensitive to ampicillin, co-trimoxazole, ceftriaxone and cefotaxime. We made a diagnosis of typhoid appendicitis. Meropenem was stopped and intravenous injection of ceftriaxone 2 g once a day was given for 10 days. The patient showed clinical improvement.
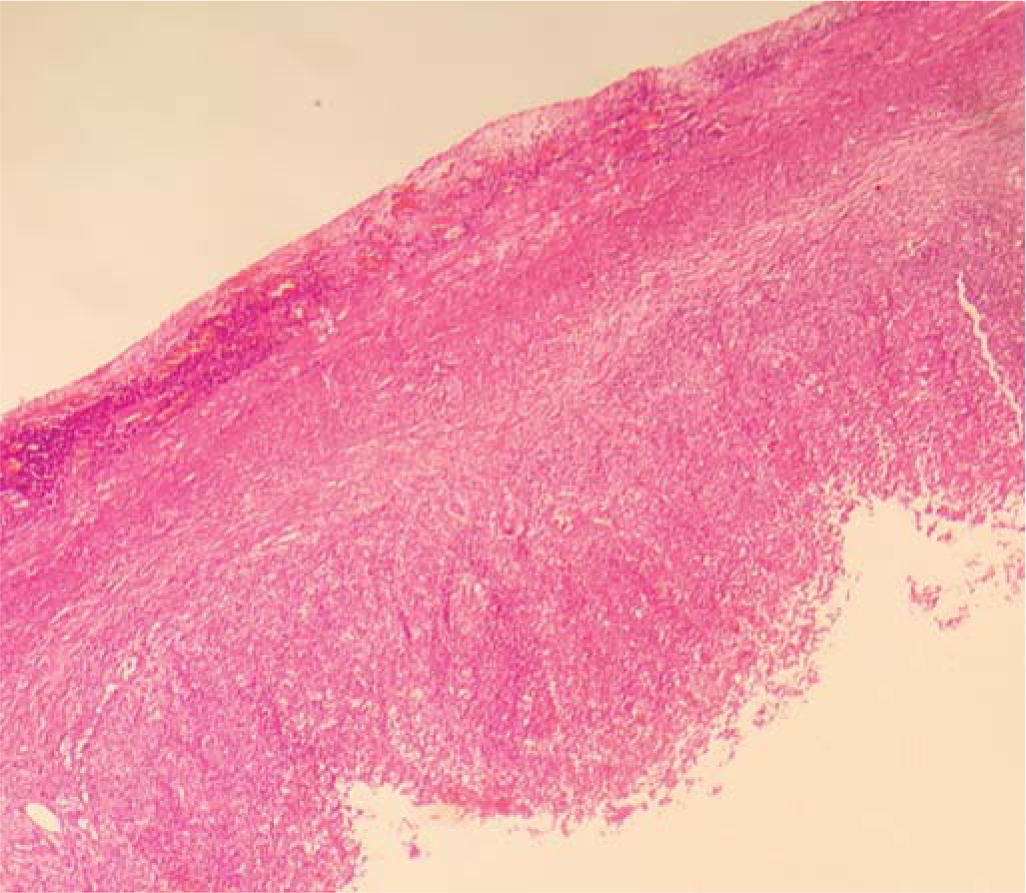
- Low-power image of appendix showing absence of transmural infiltrates of neutrophils
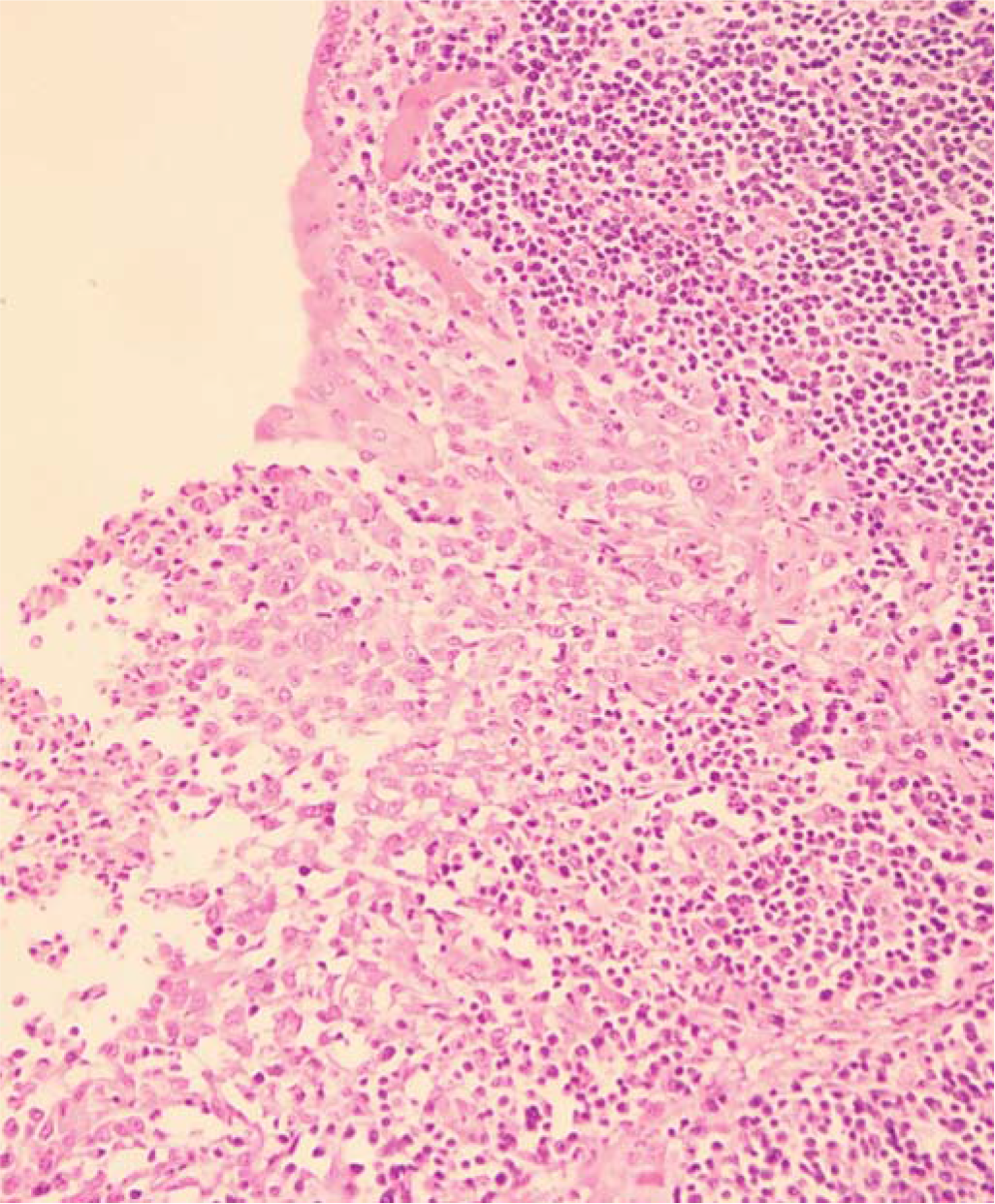
- Macrophages lining the mucosal aspect of the appendix
DISCUSSION
Descriptions of the histopathology of typhoid in the gut are usually restricted to the ileum, though typhoid also rarely affects the appendix and colon.2 Typhoid fever was a common disease in the West over a century ago and hence, it was the first chapter in Sir William Osler’s classic textbook Principles and practice of medicine, as well as in its reprint in 1967.3 In fact, this chapter3 specifically refers to typhoid appendicitis.
However, references to typhoid—either in the ileum or in the appendix—in many current textbooks of surgical pathology are brief.4,5 This is due to the decreased incidence of enteric fever, over the past century, in the West. Thus, the histopathological features of typhoid affecting the ileum as well as of typhoid appendicitis may not be known to many pathologists and the correct diagnosis may elude them. In particular, pathologists in India and other low- and middle-income countries need to be aware of this entity, as typhoid is more common in these countries.
Macrophages are the predominant inflammatory cells in typhoid.2,6 Aggregates of intramural neutrophils and/or eosinophils are specifically rare in typhoid. However, ‘transmural inflammation extending into the subserosa, neutrophilic cryptitis and crypt abscesses’as well as ‘transmural mixed inflammatory infiltrate’ have been described.7,8 Granulomas have also been reported.2,8–9 Erythrophagocytosis has also been noted in ileal biopsies in typhoid fever.8 Our case, which also contained macrophages but no intramural neutrophils, amply illustrates the classical morphology of typhoid fever, but in an unusual site—and that recognition of the entity may be difficult despite the classical appearances. Occasionally, typhoid appendicitis may be complicated with other infections.10
The genus Salmonella is classified into two main species, namely, Salmonella enterica and Salmonella bongori, based on their phenotypic profile and DNA hybridization studies. Salmonella bongori species is an animal pathogen and rarely causes human infections.
S. enterica species is further classified into six subspecies by their phenotypic profile and into 2500 serotypes based on the specificity of the two phases of the flagellar ‘H’ antigen. Most of the typhoidal Salmonellae, i.e. Salmonella serovar Typhi, serovar Paratyphi A, serovar Paratyphi B and serovar Paratyphi C and the non-typhoidal pathogenic Salmonellae, belong to species enterica subsp. Enterica.11
Typhoidal Salmonellae cause enteric fever whereas nontyphoidal Salmonellae usually cause food poisoning and gastroenteritis. However, typhoidal6,10 and non-typhoidal12 Salmonellae occasionally do cause appendicitis. Typhoid and non-typhoidal salmonellosis is treated with specific antibiotics. Non-typhoidal salmonellosis requires antibiotic therapy only in severely ill patients or those having risk factors for extra-intestinal spread. Salmonella typhi infection can also cause complications such as splenic and renal infarction.6 Some of the antibiotics used empirically for the medical management of appendicitis may not effectively treat typhoid. Hence, identifying typhoid appendicitis is important for the specific diagnosis which enables administering targeted antibiotic therapy, thereby optimizing medical management, averting complications, strengthening antibiotic stewardship by preventing antibiotic abuse and also stopping progression to carrier status.13,14
We—and our patient—were fortunate to have the results of a Typhidot and blood culture to nudge us towards the correct diagnosis. However, such appropriate supporting investigations may not be available, especially in geographical settings with limited medical resources—which is also where typhoid is common. Thus, it is imperative that pathologists familiarize themselves with the morphology of typhoid appendicitis and make the correct diagnosis on haematoxylin and eosin stains. A macrophage–monocyte infiltrate with few/no neutrophils in appendicitis should prompt the pathologist to consider the possibility of typhoid.
Appendicectomy is one of the most common surgical procedures and most appendicectomy specimens show features of ‘garden variety’ acute appendicitis, i.e. a transmural infiltrate of neutrophils. However, surprise diagnoses are not uncommon wherein management of the patient by a surgical excision may not be the complete treatment.15–17 We recommend that every specimen of the appendix be paid great attention to, by the pathologist and that surgeons always follow-up all specimens for the final histopathology report, so as not to miss unexpected findings. Campora et al. have recently published another example of ‘the man from Istanbul’ in which the appendix showed ectopic thyroid tissue in the mesoappendiceal fat.18
References
- Surgical pathology of the GI tract, liver, biliary tract, and pancreas (2nd ed). Philadelphia: Saunders; 2009.
- [Google Scholar]
- Rosai and Ackerman’s surgical pathology. (11th ed). Philadelphia: Elsevier; 2018. p. :583-627.
- [Google Scholar]
- Non-neoplastic intestinal diseases In: Mills SE, ed. Sternberg’s Diagnostic surgical pathology (6th ed). Philadelphia: Wolters Kluwer; 2015.
- [Google Scholar]
- Samonella typhi infection-related appendicitis: A case report. World J Clin Cases. 2021;9:8782-8.
- [CrossRef] [PubMed] [Google Scholar]
- Typhoid fever associated with acute appendicitis caused by an H1-j strain of Salmonella enterica serotype Typhi. J Clin Microbiol. 2005;43:1470-2.
- [CrossRef] [PubMed] [Google Scholar]
- Granulomatous inflammatory response in a case of typhoid fever. Med Princ Pract. 2009;18:239-41.
- [CrossRef] [PubMed] [Google Scholar]
- An unusual cause of granulomatous ileitis: With a brief history of the pathology of typhoid. Int J Surg Pathol. 2018;26:240-1.
- [CrossRef] [PubMed] [Google Scholar]
- Typhoid fever and acute appendicitis: A rare association not yet fully formed. Case Rep Gastroenterol. 2017;11:446-51.
- [CrossRef] [PubMed] [Google Scholar]
- Salmonella, Shigella, and Yersinia. Clin Lab Med. 2015;35:225-46.
- [CrossRef] [PubMed] [Google Scholar]
- Appendicitis in non-typhoidal salmonella bacteraemia. Oxf Med Case Reports. 2018;2018(11):omy082.
- [CrossRef] [PubMed] [Google Scholar]
- Available at https://emedicine.medscape.com/article/1976216-overview (accessed on 22 Nov 2021)
- Toxoplasma appendicitis: A once-in-a-lifetime diagnosis! Int J Surg Pathol. 2018;26:89-92.
- [CrossRef] [PubMed] [Google Scholar]
- Histopathologic characteristics of the transitional stage of measles-associated appendicitis: Case report and review of the literature. Hum Pathol. 2011;42:285-90.
- [CrossRef] [PubMed] [Google Scholar]
- Intramural ova of Enterobius vermicularis in the appendix—an egg-topic location! Int J Surg Pathol 2021:10668969211032455.
- [CrossRef] [PubMed] [Google Scholar]
- Abdominal ectopic thyroid tissue: The man from Istanbul. Int J Surg Pathol. 2019;27:553-5.
- [CrossRef] [PubMed] [Google Scholar]




