Translate this page into:
Upward trend of caesarean sections in India: Incision over precision
2 Department of Paediatrics, Post Graduate Institute of Medical Education and Research, Chandigarh, India
Corresponding Author:
Rajesh Kumar
Department of Community Medicinel, Post Graduate Institute of Medical Education and Research Chandigarh
India
dr.rajeshkumar@gmail.com
| How to cite this article: Dhirar N, Kumar R, Dudeja S. Upward trend of caesarean sections in India: Incision over precision. Natl Med J India 2018;31:316-317 |
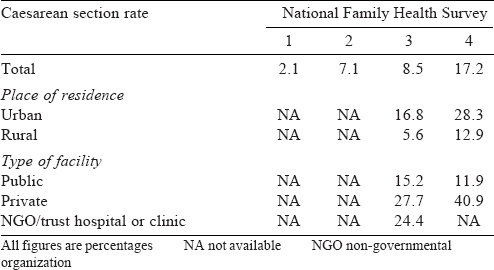
There was a time when caesarean section (CS) was a rarity, but now globally these are being done more frequently.[1],[2],[3] A rising trend has been observed in India too. The data of the National Family Health Survey-4 (NFHS-4)[4] conducted in 2015–16 indicated that the CS rate in India was 17.2% compared to 8.5% in the NFHS-3 conducted in 2005–6.[5] The CS rates in the NFHS-1 and -2 were low—2.1% and 7.1%, respectively [Table - 1].[6] The rising trend of CS rates is alarming.
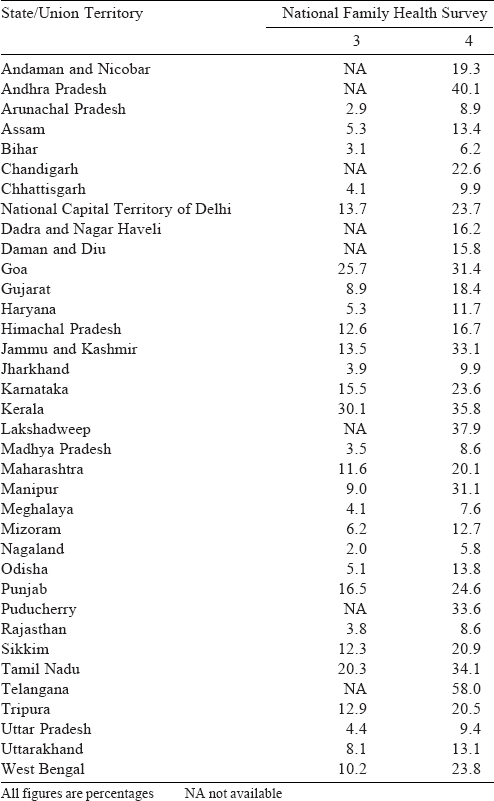
State-wise comparison of CS rates in the NFHS-4 show much variation [Table - 2]. The highest proportion was observed in Telangana (58.0%), Andhra Pradesh (40.1%), Kerala (35.8%) and Tamil Nadu (34.1%) while the rates were low in the Empowered Action Group states of Bihar (6.2%), Chhattisgarh (9.9%), Jharkhand (9.9%), Madhya Pradesh (8.6%), Odisha (13.8%), Rajasthan (8.6%), Uttarakhand (13.1%) and Uttar Pradesh (9.4%). The northeastern states too had lower rates with the exception of Manipur (31.1%) and Sikkim (20.9%).
The CS rates were higher in deliveries occurring in private healthcare facilities, across all states. The rates were also higher in urban areas compared to rural areas, though both had shown an increase compared to the previous round.[4] Private healthcare facilities did more than one-third (40.3%) deliveries by CS. Previous rounds of NFHS found an association between increased rates of CS with maternal education, parity and high wealth quintiles.[5],[6]
Non-medical indications for CS are more common in the private sector.[7] In India, 0.1%–0.2% of CS are done for non-medical indications.[8]
In recent years, there have been revisions in recommendations related to CS for term foetuses. It is ethically unacceptable to do CS for non-medical indications according to the International Federation of Gynaecology and Obstetrics (FIGO).[9] A rise in CS rates is linked with a fall in the neonatal mortality rate. WHO states that as countries increase their C S rates up to 10%, the neonatal and maternal mortality rates decrease.[2] However, there is evidence that if the increase in CS rates is beyond 10%, there is no further reduction in the neonatal and maternal mortality rates.[2] Previously, CSs have been categorized according to the indications (e.g. foetal distress, cephalopelvic disproportion [CPD] and failure in progression of labour). However, these are open to interpretation. The Robson (or ‘10 groups’) system overcomes some of the problems concerning the classification of ‘indications’.[10] The Robson system is modest, vigorous, replicable and clinically relevant. It permits comparisons and analysis of CS rates more reliably across different facilities, cities and regions. It categorizes women into 1 of 10 groups based on characteristics such as previous pregnancy, lie of the baby, number of babies and uterine scar. This classification may be used for defining indications of CS in patients as well as for national and international comparisons.[10]
The aim of public health is to prevent disease, but when a treatment option becomes a rising risk, it defeats the purpose. CS rates need a baseline assessment and monitoring of trends across cities and states. Careful monitoring of demographic profile of mothers, indications and rates of CS should be done to proactively control the unprecedented rise. No such systems are in place in India.
Every delivery can be managed on the basis of defined protocols. There should be periodic scrutiny of surgical procedures during delivery. Medical audits and strict supervision are required at government and private facilities. Based on the recommendations, prompt action should be taken at both individual and healthcare facility levels. As has been observed in NFHS-4, states with a higher maternal mortality rate have a lower CS rate. Hence, while CS is necessary, it should be done on the basis of a clear set of indications. Stricter action may be necessary for healthcare facilities, mostly private ones, where CS is being done for pecuniary benefit. Laws in relation to practical aspects of delivery need to be strengthened to safeguard the interest of not only patients but also obstetricians. Considering the variation in patient profiles and risk factors, relevant guidelines should be framed for CS. National guidelines should be made available for both public and private health facilities.
Conflicts of interest. None declared
| 1. | Cavallaro FL, Cresswell JA, França GV, Victora CG, Barros AJ, Ronsmans C, et al. Trends in caesarean delivery by country and wealth quintile: Cross-sectional surveys in Southern Asia and Sub-Saharan Africa. Bull World Health Organ 2013;91: 914-22D. [Google Scholar] |
| 2. | World Health Organization Human Reproduction Programme, 10 April 2015. WHO statement on caesarean section rates. Reprod Health Matters 2015;23:149-50. [Google Scholar] |
| 3. | Roberts CL, Nippita TA. International caesarean section rates: The rising tide. Lancet Glob Health 2015;3:e241-2. [Google Scholar] |
| 4. | Ministry of Health and Family Welfare. National Family Health Survey (NFHS-4). 2015-16. India Fact Sheet. Available at http://rchiips. org/nfhs/pdf/NFHS4/India.pdf (accessed on 20 Oct 2017). [Google Scholar] |
| 5. | Ministry of Health and Family Welfare. National Family Health Survey-3. Maternal Health 8; 2010:191-222. Available at http://rchiips.org/nfhs/NFHS-3%20Data/ VOL-1/Chapter%2008%20-%20Maternal%20Health%20(490K).pdfhttp:/ / www.rchiips.org/nfhs/NFHS-3Data/V0L-1/Chapter08-MaternalHealt(490K).pdf (accessed on 20 Oct 2017). [Google Scholar] |
| 6. | International Institute for Population Sciences. Maternal and Child Health. National Family Health Survey; 1995:227-67. Available at http://rchiips.org/NFHS/data/ india1/iachap9.pdf (accessed on 20 Oct 2017). [Google Scholar] |
| 7. | Leone T, Padmadas SS, Matthews Z. Community factors affecting rising caesarean section rates in developing countries: An analysis of six countries. Soc Sci Med 2008;67:1236-46. [Google Scholar] |
| 8. | Souza JP, Gülmezoglu A, Lumbiganon P, Laopaiboon M, Carroli G, Fawole B, et al. Caesarean section without medical indications is associated with an increased risk of adverse short-term maternal outcomes: The 2004-2008 WHO Global Survey on Maternal and Perinatal Health. BMC Med 2010;8:71. [Google Scholar] |
| 9. | FIGO Committee. Ethical issues in obstetrics and gynecology by the FIGO committee for the study of ethical aspects of human reproduction and women’s health. Ethical Issues Obstet Gynecol 2012;91. [Google Scholar] |
| 10. | 10 Betrán AP, Vindevoghel N, Souza JP, Gülmezoglu AM, Torloni MR. A systematic review of the Robson classification for caesarean section : What works, doesn’t work and how to improve it. PLoS One 2014;9:e97769. [Google Scholar] |
Fulltext Views
1,096
PDF downloads
298




