Translate this page into:
Viper bite and its complications at a tertiary care centre in southern part of West Bengal: A prospective, clinical, socioeconomic and epidemiological study
Corresponding Author:
Kripasindhu Gantait
Department of General Medicine, Midnapore Medical College, Midnapore, West Bengal
India
gkripasindhu@yahoo.inShinjan Patra
Department of General Medicine, Midnapore Medical College, Midnapore, West Bengal
India
shinjan100@gmail.com
| How to cite this article: Gantait K, Patra S, Chowdhury R, Pramanick S. Viper bite and its complications at a tertiary care centre in southern part of West Bengal: A prospective, clinical, socioeconomic and epidemiological study. Natl Med J India 2019;32:13-16 |
Abstract
Background. Viper snake bite is a threat to the Indian health system with 83 000 deaths annually. There is a paucity of literature regarding independent risk factors for renal damage due to viper bite. We present the scenario in a rural part of West Bengal and highlight some vital factors to prevent the complications.Methods. We screened all patients with snake bite from January 2012 to December 2015 in Midnapore Medical College and chose definite viper bites according to our inclusion criteria, treated them as per the Indian government protocol, followed them for any acute kidney injury, managed them with haemodialysis (HD) if needed and compared some socioeconomic and clinical factors between HD and non-HD groups to predict the outcome.
Results. A total of 1220 snake bites were screened, 660 were viper bites, and 1 80 needed HD at least once. The HD group mostly consists of tribal population (75% v. 45% in non-HD group) who used unscientific first-aid measures. Bite timing was characteristically between 4 a.m. and 8 a.m., especially during defecation in fields, without any considerable seasonal variation. The average bite-to-needle time was 24.6 hours in the HD group and 5.1 hours in the non-HD group, with the average economic burden of ₹3345 in the HD group and ₹730 in the non-HD group.
Conclusions. Along with formal education, there is a need to create awareness among the relatively poor tribal population about snake bite to reduce the bite-to-needle time.
Introduction
Poisonous snake bites are a major public health threat in tropical countries including India.[1] WHO estimates approximately 125 000 deaths and 2 500 000 poisonous snake bites a year worldwide. Data regarding mortality, morbidity and incidence rates of poisonous snake bites from India are scarce. More than 2700 species of snakes are recognized worldwide, but only about 450 of these have front fangs that make them capable of injecting venom during a bite. Only a few of these are of medical importance. The venomous snakes belong to four families: Elapidae, Viperidae, Hydrophiidae and Colubridae. Vipers are the most widely distributed species, especially in India (Russell viper and Echis carinatus are the two most common), Myanmar, Bangladesh, Pakistan and Thailand. Among these the Russell viper is abundant in rural areas of West Bengal especially in the district of Paschim Medinipur.[2] Renal dysfunction is characteristically associated with Russell viper, and acute renal failure (ARF) is a dreaded complication needing haemodialysis (HD). The earliest sign of a viper bite is pain and swelling of the affected part followed by subcutaneous oedema progressing to necrosis or gangrene.[3] Viper bites lead to coagulation abnormalities by blocking multiple sites of the coagulation cascade such as inhibition of factor-X activation and fibrin clot stabilization. However, the renal manifestations are unpredictable but most commonly acute tubular necrosis in 70%-80% of patients.[4] Oliguria or anuria can develop after a few hours or can be delayed up to 96 hours.[5] Features unique to snake bite-induced ARF are severe tubular and vascular lesions, increased apoptosis (defined as accelerated physiological cell death) in the distal tubules and in the presence of eosinophils, mast cells and hyperplastic fibroblasts in the interstitium.[6] The pathogenic mechanisms responsible for this renal insult include hypotension, leading to impaired renal perfusion, intravascular haemolysis, myoglobinuria, etc.[7] Although the pathophysiology of acute kidney injury in a viper bite is well known, data regarding prevention of complications in India are lacking. Comprehensive care against viper bite is essential to protect against acute kidney injury and the possible hazards of renal replacement therapy. We estimated the incidence of acute kidney injury in viper bites, need for HD and possible risk factors for acute kidney injury.
Methods
We did a prospective longitudinal study at Midnapore Medical College in the city of Midnapore from January 2012 to December 2015.
The inclusion criteria were a definitive history of viper bite or local signs of fang marks,[8] oedema, cellulitis and gangrene following a bite by an unknown animal taking into consideration the patient’s locality and habitat of the snake. Patients with no identifiable fang marks were excluded, as were those with comorbid conditions such as hypertension, diabetes mellitus, chronic liver disease, chronic obstructive pulmonary disease and chronic heart failure. Patients receiving nephrotoxic drugs were also excluded.
A detailed history was taken including the exact timing of the bite, and a complete physical examination along with bedside whole blood clotting time (WBCT-20) was done every 30-minutes for up to 3 hours and hourly thereafter[9] along with maintenance of an intake and output chart. Laboratory investigations done included a complete blood count, serum urea and creatinine, liver function tests and serum electrolytes, bleeding and clotting times, prothrombin time and international normalized ratio (INR). Urine was examined for red blood cells, granular casts or epithelial cell casts. An X-ray of the chest and ultrasound of the abdomen were also done.
Treatment
All patients received tetanus toxoid injection at presentation. We classified the patients as mild or severe according to the time taken for appearance of symptoms after the snake bite. Ten vials of polyvalent anti-snake venom (ASV) were infused in 300 ml of normal saline premedicated with hydrocortisone and an anti- histamine over 1 hour in all viper bites. We repeated WBCT every 6 hours after the first dose of ASV and did not give ASV if two consecutive WBCTs were clotted.[10] We gave a maximum of 30 vials of ASV in viper bite. Antibiotics were given to prevent local infection, but non-steroidal anti-inflammatory drugs were avoided. We used paracetamol or chymotrypsin for pain relief. We maintained urine output by giving appropriate amounts of fluids and avoided diuretics. However, we did HD if there was evidence of acute kidney injury in a patient with a viper bite (increase in serum creatinine by 0.3 mg/dl within 48 hours, increase in serum creatinine 1.5 times the baseline or urine volume <0.5 ml/kg/hour for 6 hours), with life-threatening hyperkalaemia, refractory metabolic acidosis, pulmonary oedema, uraemic encephalopathy, uncorrectable volume overload or anuria for 24 hours.
Data collection and processing
We divided the viper bite population into two groups: those who received HD and those who did not with or without evidence of systemic envenomation. We followed them up to discharge or death in the hospital. We collected data such as age, sex, locality, ethnicity (tribal/non-tribal) and compared the presence of local site swelling, necrosis, gangrenous changes, snake bite-to-needle time, hypotension, disseminated intravascular coagulation (DIC), coagulopathy and amount of ASV given, and outcome.
Ethical guidelines
We obtained approval from the Ethics Committee of Midnapore Medical College and Hospital as well as written informed consent from all the participants.
Results
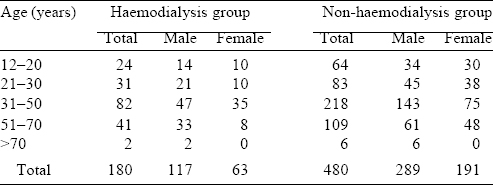
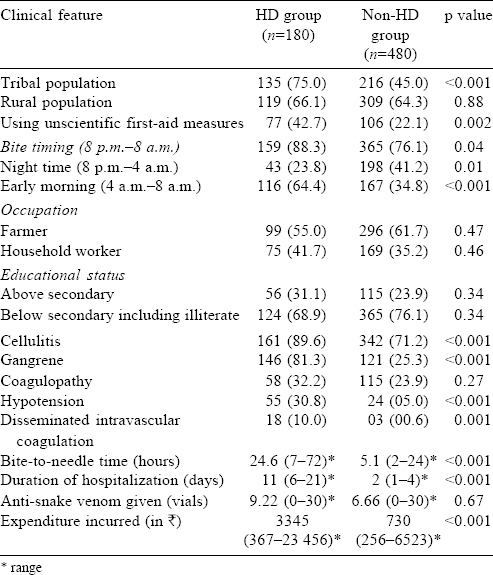
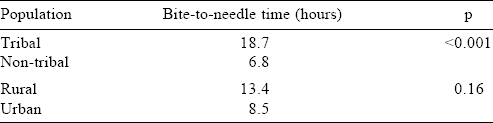
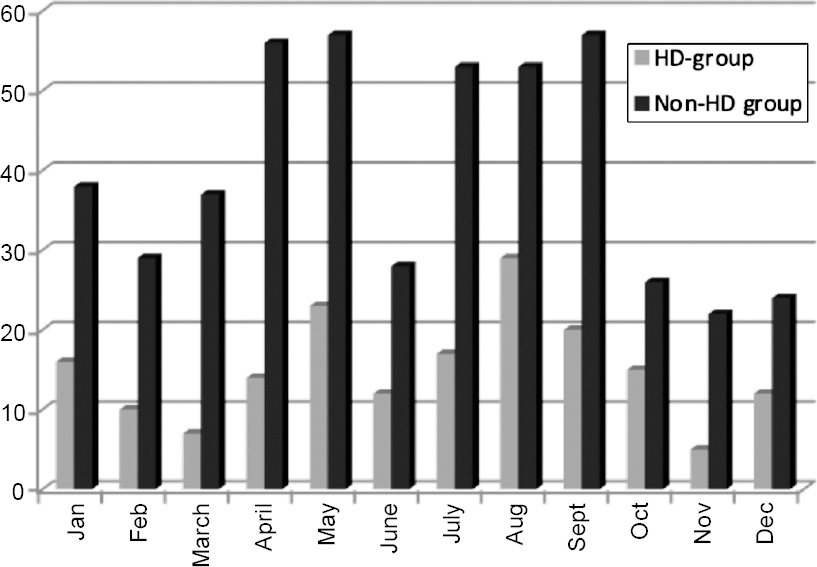
A total of 1220 patients with snake bite were seen during the study period, 820 of them had features of envenomation and 660 were identified as viper bites by our inclusion criteria. The rest (160 patients) were neurotoxic snake bites, 17 of the patients died with a mortality rate of 10. 6%. Among the 660 patients with viper bites, 180 required HD. Thirty-eight patients with viper bite died—28 of 180 (15%) who required HD died and 10 of 480 patients (2%) who did not require HD died. Most patients were in the 31-50 years age group (45% in both groups) and there was no significant difference in sex between the two groups [Table - 1]. There was not much seasonal variation as even in the winter months there were a number of toxic snake bites with envenomation. The most common site of the snake bite was the lower limb (78% in the HD group v. 73% in the non-HD group). Also, there were significantly more tribals in the HD group than in the non-HD group suggesting that they reached late to our tertiary healthcare centre because of poor educational status and lack of awareness [Table - 2]. Another noteworthy point was a similar proportion of urban and rural population in these two groups. Expectedly bite-to-needle time, i.e. time taken from the snake bite (as per patients’ statement) up to the time of administering ASV in the hospital, was more in tribal and rural populations compared to non-tribal and urban people. Although this delay was significant only in the tribal and not in the rural population ([Table - 3]. A comparison of various clinical parameters between the HD and non-HD groups, expectedly showed that signs of local site swelling as well as systemic features of DIC and hypotension were more in the HD group. Also, the bite-to-needle time was much more in the HD group (mean 24.6 hours v. 5.1 hours in the non-HD group; [Table - 2]).
Discussion
India is estimated to have the highest snake bite mortality in the world. WHO estimates the number of bites to be 83 000 per annum with 11 000 deaths.[11] Most fatalities are due to the victim not reaching the hospital in time where protocol-based treatment can be administered. Moreover, the community is often ill- informed about occupational risks and simple measures that could prevent snake bite. After the snake bite, patients often use measures such as applying tourniquets, or cutting and suctioning the wound. They often take such patients to a local ‘tantrik’ or ‘ojha’ first, resulting in a delay in seeking appropriate treatment. Such local tribal practices in our district are common and more such patients underwent HD. The caregivers of our patients often applied a tight tourniquet, and then ‘sucked’ the poison from the bite wound. This would result in severe local infection, cellulitis and gangrene. Another important aspect was that doctors at the primary health centre, subcentre, block primary health centre and rural hospitals could not treat snake bite patients properly due to lack of infrastructure. At the primary and secondary level, multiple protocols are being followed for administration of polyvalent ASV.[12] Primary care physicians usually either over- or under-treat patients with snake bite, either giving ASV without any signs of envenomation or not giving it despite obvious and serious features of envenomation. These and other reasons have resulted in the burden of snake bite in Paschim Medinipur district along with the burden from the adjoining districts of Orissa and Jharkhand coming to our medical college.
 |
| Figure 1: Month-wise distribution of snake bites during the study period |
Our study is different as there are few, if any, studies comparing the HD and non-HD groups in India. Most of our patients are below the poverty line and extremely poor. Women were represented a little more in the non-HD group. The distribution of those undergoing HD in the winters and rainy season was the same, contrary to previously published reports.[13],[14],[15] As expected, tribals were in a large proportion in the HD group (75% v. 45% in the non-HD group, p<0.001). However, there was no significant difference between the rural and urban population between these two groups (66.1% in the HD and 64.3% in the non-HD group). The time of snake bite was between 4 a.m. and 8 a.m. in the HD group (64.4% v. 34.8%, p<0.001) patients, suggesting a morning bite habit in most toxic vipers, as well as the vulnerability of people who go to defecate in the fields in the morning. Indirectly, this suggests the need to encourage people to stop defecating in the fields. On comparing the educational status, people who had above secondary level education required more HD though the difference was not statistically significant (31.1% v. 23.9%, p=not significant).[16] Thus, formal education alone may not be sufficient to tackle the problem of adverse outcomes in patients with snake bite. There was a larger proportion of patients in the HD group who used incorrect first-aid measures (42.7% v. 21.1%, p=0.002). However, the amount of ASV used was comparable in these two groups suggesting a possible inability of ASV to treat the acute kidney injury after it has set in.
Clinical complications such as cellulitis, gangrene, hypotension and DIC were more in the HD group, but coagulopathy was more in the non-HD group suggesting unifying pathogenic mechanisms in clotting abnormality and renal damage. Patients who underwent HD remained in hospital for a longer and the economic burden even in a government hospital was more than in those who did not require HD (money spent was ₹3345 v. ₹730 in the non-HD group). The bite-to-needle time was 24.6 hours in those requiring HD compared to 5.1 hours in the non-HD group, and has been reported in a previous study.[17]
We attempted to find risk factors of viper bite that could predict the outcome of renal involvement and need for HD. The potential economic, social and medical burden of HD in India is large as patients with chronic kidney disease are not able to get HD regularly in government hospitals. If we educate the relatively poor tribal population about the importance of proper first-aid management and ask them to report to a government hospital at the earliest after any form of snake bite, we can reduce this load of HD. While education and awareness alone may not suffice to decrease this burden of HD, defecation in the open should be discouraged. Adequate preparedness is important as the only definitive treatment of viper bite is early administration of ASV. Once acute kidney injury sets in, ASV is ineffective to reverse this pathology.[18]
Acknowledgements
We thank our Principal, Vice-Principal and all members of our Nephrology Unit for their constant cooperation and support.
Conflicts of interest. None declared
| 1. | Chippaux JP. Snake-bites: Appraisal of the global situation. Bull World Health Organ 1998;76:515-24. [Google Scholar] |
| 2. | Lei C, Badowski NJ, Auerbach PS, Norris RL. Disorders caused by venomous snakebites and marine animal exposures. In: Kasper D, Fauci A, Hauser S, Longo D, Jameson JL, Loscalzo J. Harrison ‘s principals of internal medicine. 19th ed. New York:McGraw-Hill; 2014:2734. [Google Scholar] |
| 3. | Ohsaka A. Hemorrhagic, necrotizing and edema-forming effects of snake venoms. In: Lee CY (ed). Snake Venoms. Berlin:Springer-Verlag; 1979:480-546. [Google Scholar] |
| 4. | Sitprija V, Boonpucknavig V. Snake venoms and nephrotoxicity. In: Lee CY (ed). Snake Venoms. Berlm:Sprmger-Verlag; 1979:997-1018. [Google Scholar] |
| 5. | Chugh KS, Pal Y, Chakravarty RN, Datta BN, Mehta R, Sakhuja V, et al. Acute renal failure following poisonous snakebite. Am J Kidney Dis 1984;4:30-8. [Google Scholar] |
| 6. | Date A, Shastry JC. Renal ultrastructure in acute tubular necrosis following Russell’ s viper envenomation. J Pathol 1982;137:225-41. [Google Scholar] |
| 7. | Condrea E, Devries A, Mager J. Hemolysis and splitting of human erythrocyte phospholipids by snake venoms. Biochim Biophys Acta 1964;84:60-73. [Google Scholar] |
| 8. | Norris RL. Bite marks and the diagnosis of venomous snakebite. Wilderness Environ Med 1995;6:159-61. [Google Scholar] |
| 9. | Simpson ID. Snakebite management in India, the first few hours : A guide for primary care physicians. J Indian Med Assoc 2007;105:324, 326, 328. [Google Scholar] |
| 10. | Singh S, Singh G. Snake Bite: Indian guidelines and protocol. In: API Medicine Update 2013. Mumbai:API; 2013:424-6. [Google Scholar] |
| 11. | Kasturiratne A, Wickremasinghe AR, de Silva N, Gunawardena NK, Pathmeswaran A, Premaratna R, et al. The global burden of snakebite: A literature analysis and modelling based on regional estimates of envenoming and deaths. PLoS Med 2008;5:e218. [Google Scholar] |
| 12. | Simpson ID. A study of the current knowledge base in treating snake bite amongst doctors in the high-risk countries of India and Pakistan: Does snake bite treatment training reflect local requirements? Trans R Soc Trop Med Hyg 2008; 102:1108-14. [Google Scholar] |
| 13. | Punde DP. Management of snake-bite in rural Maharashtra: A 10-year experience. Natl Med J India 2005;18:71-5. [Google Scholar] |
| 14. | Sharma N, Chauhan S, Faruqi S, Bhat P, Varma S. Snake envenomation in a North Indian hospital. Emerg Med J 2005;22:118-20. [Google Scholar] |
| 15. | Kalantri S, Singh A, Joshi R, Malamba S, Ho C, Ezoua J, et al. Clinical predictors of in-hospital mortality in patients with snake bite: A retrospective study from a rural hospital in central India. Trop Med Int Health 2006;11:22-30. [Google Scholar] |
| 16. | Anjum A, Husain M, Hanif SA, Ali SM, Beg M, Sardha M. Epidemiological profile of snake bite at tertiary care hospital, North India. J Forensic Res 2012;3:146. [Google Scholar] |
| 17. | Suchithra N, Pappachan JM, Sujathan P. Snakebite envenoming in Kerala, South India: Clinical profile and factors involved in adverse outcomes. Emerg Med J 2008;25:200-4. [Google Scholar] |
| 18. | Chugh KS. Snake-bite-induced acute renal failure in India. Kidney Int 1989;35: 891-907. [Google Scholar] |
Fulltext Views
2,387
PDF downloads
2,294




