Translate this page into:
Workplace violence against resident doctors in a tertiary care hospital in Delhi
Corresponding Author:
Tanu Anand
Maulana Azad Medical College and associated hospitals, New Delhi 110002
India
drtanu.anand@gmail.com
| How to cite this article: Anand T, Grover S, Kumar R, Kumar M, Ingle GK. Workplace violence against resident doctors in a tertiary care hospital in Delhi. Natl Med J India 2016;29:344-348 |
Abstract
Background. Healthcare workers particularly doctors are at high risk of being victims of verbal and physical violence perpetrated by patients or their relatives. There is a paucity of studies on work-related violence against doctors in India. We aimed to assess the exposure of workplace violence among doctors, its consequences among those who experienced it and its perceived risk factors.Methods. This study was done among doctors working in a tertiary care hospital in Delhi. Data were collected by using a self-administered questionnaire containing items for assessment of workplace violence against doctors, its consequences among those who were assaulted, reporting mechanisms and perceived risk factors.
Results. Of the 169 respondents, 104 (61.4%) were men. The mean (SD) age of the study group was 28.6 (4.2) years. Sixty-nine doctors (40.8%) reported being exposed to violence at their workplace in the past 12 months. However, there was no gender-wise difference in the exposure to violence (p=0.86). The point of delivery of emergency services was reported as the most common place for experiencing violence. Verbal abuse was the most common form of violence reported (n=52; 75.4%). Anger, frustration and irritability were the most common symptoms experienced by the doctors who were subjected to violence at the workplace. Only 44.2% of doctors reported the event to the authorities. 'Poor communication skills' was considered to be the most common physician factor responsible for workplace violence against doctors.
Conclusions. A large proportion of doctors are victims of violence by their patients or relatives. Violence is being under-reported. There is a need to encourage reporting of violence and prepare healthcare facilities to tackle this emerging issue for the safety of physicians.
Introduction
Workplace violence is violence or threat of violence against workers. It can occur at or outside the workplace and can range from threats and verbal abuse to physical assaults and homicide. [1] Workplace violence can occur in any organization, against anybody and at any time. However, some workers are at greater risk. The Occupational Safety and Health Administration (OSHA), USA, describes workers who provide services, work in remote or high crime areas, and those who work shift hours and/or have a great deal of contact with the public are at risk. This group includes healthcare workers such as physicians, nurses and other providers (both community- and hospital-based), social workers and psychiatric evaluators. [2]
According to the data of the Bureau of Labour Statistics (BLS), USA for 1995, workplace assaults and violent acts occur in the health sector more often than in any other industry. [3] Several independent studies all over the world have reported the prevalence of workplace violence among physicians to be 56%-75%. [4] ,[5] ,[6] ,[7] ,[8] Patients and their relatives are the most common perpetrators of non-fatal workplace violence. [9] However, violence and abuse is also committed by hospital co-workers, particularly emotional abuse and sexual harassment. [10] In several countries a pattern seems to emerge whereby patients and their relatives are the main perpetrators of physical violence while staff are the main perpetrators of psychological violence. [11] Workplace violence in the health sector has a major impact on the effectiveness of health systems, especially in developing countries. [11]
India has the second largest population in the world, where healthcare is one of the growing fields. [12] Instances of patient′s relatives assaulting the treating doctor are a common scenario all over India. [13] ,[14] However, there is limited research on violence in healthcare settings against physicians in India. A study by Ori et al. in 2014 in Manipur found that 78% of doctors had experienced some form of violence. [15] We assessed the magnitude, consequences and risk factors for workplace violence against physicians working in a government hospital in Delhi. We also examined the incident reporting patterns of affected doctors.
Methods
Study settings and participants
This was an institution-based study done among resident doctors working in a tertiary care hospital attached to a medical college in central Delhi. The hospital has around 1600 beds in all the medical and surgical specialties catering to a large population of Delhi and neighbouring states. The hospital has a highly skilled and trained workforce. [16]
Inclusion and exclusion criteria
All resident doctors working for at least 1 year in the hospital were eligible for the study. Interns and undergraduate students and doctors who did not give consent to participate in the study were excluded. The mean age was calculated on the basis of the findings reported by the victims.
Sampling and sample size
Taking 78% as the expected prevalence rate of violence at workplace experienced by doctors as in a previous study in similar settings [15] at a 95% confidence level, the required sample size was calculated to be 113 to yield a prevalence estimate with 10% precision. For the survey, we included about 200 eligible doctors working in various departments. However, 169 doctors could be contacted and interviewed. Data were collected between January 2014 and June 2014. A pre-tested, semi-structured, self-administered questionnaire was used for data collection. The questionnaire was divided into five sections:
Section I: Identification such as age, gender, educational qualifications, work experience, job setting, designation in current workplace, whether working in shifts and type of patient care.
Section II: Exposure to workplace violence ever in life and in past 12 months; type of violence experienced and its description.
Section III: Consequences of exposure to workplace violence such as symptoms following the exposure, treatment history, and work changes as a result of the event.
Section IV: Reporting mechanisms of workplace violence.
Section V: Assessing the perception of participating doctors about the patient, physician and external factors responsible for increasing incidence of workplace violence.
The study tool was developed after a detailed review of studies done in similar settings elsewhere. [4] ,[5] ,[6] ,[7] ,[8] ,[10] ,[12] ,[15]
Content validity of the tool
To ensure content validity, the tool along with the blueprint, objectives and criteria checklist were given to five experts in the field of public health and psychiatry. There was 100% agreement among the experts with respect to items 7 to 10 in section I; all the eleven items in section II, five in section III, two in section IV; and three in section V.
Reliability of study tool
The tool was administered to 20 doctors from a different hospital. The participants said that the items used in the questionnaire were clear and understandable.
All the selected doctors were contacted personally and after taking their informed consent, the questionnaire was administered and data collected on the spot.
Statistical analysis
The data collected were entered in Microsoft Excel and analysed using Epi-info 2005 software of WHO and SPSS version 16.0 (SPSS Inc., Chicago, IL). The results are presented as proportions and any difference between two proportions in relation to a particular factor was assessed by Chi-square (or Fischer exact test if the expected frequency in any cell was <5) and was considered significant at p<0.05.
Ethical considerations
Informed written consent was taken from all the participants and the study was approved by the ethics committee of our institution.
Results
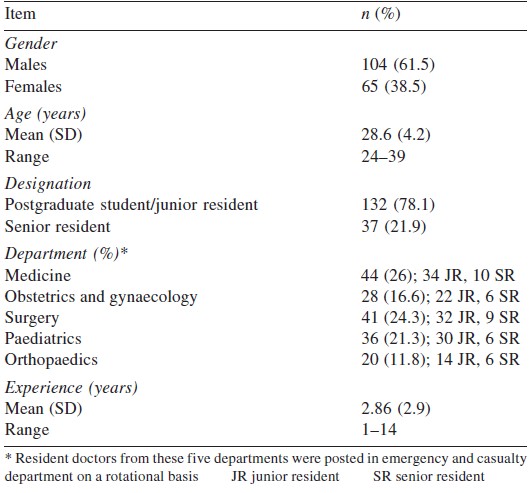
Of the 169 participants, 65 were women (38.5%). The mean (SD) age of the participants was 28.6 (4.2) years (range 24-39 years). There were 132 postgraduate students (78.1%) and 37 senior residents (21.9%). The mean (SD) years of experience of the study group was 2.86 (2.9) years (range 1-14 years). The department-wise distribution showed that the maximum resident doctors were from medicine (n=44; 26%) followed by surgery (n=41; 24.3% [Table - 1]).
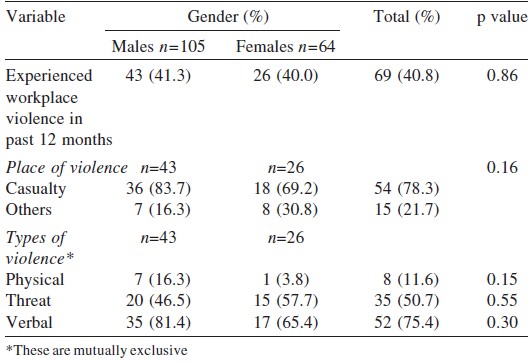
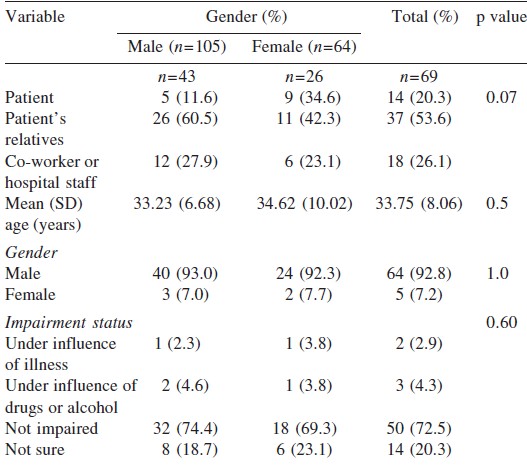
Sixty-nine doctors (40.8%) reported being ever exposed to workplace violence. There was no gender-wise difference in exposure to violence (men 31, 29.8%; women 21, 32.3%; p=0.73). More than three-fourths of the doctors faced violence in the emergency services (n=54; 78.3%). Of the 69 resident doctors who reported being exposed to violence at the workplace, 8 (11.6%) had been assaulted physically, 35 (50.7%) had been threatened, while 52 (75.4%) said that they were verbally abused. A higher proportion of males were abused verbally as compared to females. None of them reported sexual abuse ([Table - 2]). In a majority of instances the violence was perpetrated by the patients′ relatives (n=37; 53.6%), followed by co-workers or hospital staff (n=18; 26.1%). Most perpetrators of violence (n=64, 92.8%) were men with an approximate mean (SD) age of 33.8 (8.06) years (range 20-72 years; [Table - 3]). The most common reasons for the violence was ′death of the patient′ (n=10; 14.5%) and ′delay in initiation of treatment′ (n=10; 14.5%). Other reasons were ′lack of medicines′, ′mismanagement of the patients′ as perceived by their relatives and ′inadequate attention given to the patient′.
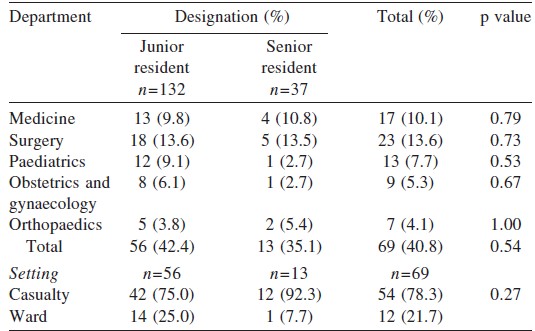
A higher proportion of resident doctors from the department of surgery (13.6%) reported exposure to workplace violence followed by residents from the department of medicine (10.1%). However, there was no significant difference between exposure to workplace violence among junior and senior residents of each department. A higher proportion of senior residents (n=12; 92.3%) faced violence in the emergency services as compared to junior residents, though the difference was not significant ([Table - 4]).
Of the 8 resident doctors who faced physical violence, all of them felt angry, frustrated, fearful, irritable and sad. There were 4 (50%) who felt fatigued and had low self-esteem. Six reported developing depression following the event while 2 reported to have headache (25%). Two doctors were hospitalized following the event. Among those who reported non-physical violence (n=61), all felt angry, frustrated and irritable. While 36 resident doctors (59%) became fearful, 44.3% (n=27) felt sad and 31.1% (n=19) developed headache and felt fatigued. Nearly one-quarter of the participants reported feeling depressed and with low self-esteem (n=15; 24.6%) following the event. None of the resident doctors who experienced non-physical violence were hospitalized while 2 of 8 who experienced physical violence were hospitalized ([Table - 5]).
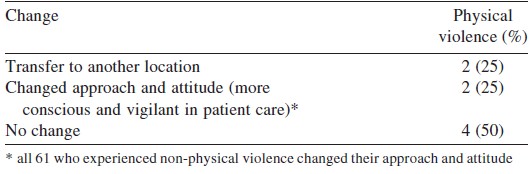
While 2 of the affected doctors reported no change in workplace as a result of the event, 67 (97.1%) said that they became more conscious and vigilant. Only 23 of those who experienced workplace violence reported the event to higher authorities (33.3%). While 11 had reported the event to the medical superintendent of the hospital, 6 reported it to the concerned senior faculty member of their department, 4 to the casualty medical officer and 2 to their head of department. The most common mode of reporting was verbal (n=18; 78.2%). Of those who did not report (n=46), all of them considered it a useless and time-wasting activity.
Only half the participants (n=83; 49.1%) were aware of any legislation regarding punishment for assault on healthcare workers.
Resident doctors were asked about risk factors that may have led to workplace violence. Among the physician factors, 137 (81.1%) considered poor communication skills as the most common. Poor conflict resolution skills among physicians were considered by 96 of the resident doctors (56.8%). Drug addiction among patients or their relatives was perceived as the most common risk factor for violence by 116 of the participants (68.6%) followed by a history of personality disorders among patients′ or their relatives by 109 (64.5%). The most common external risk factor for workplace violence was considered to be overcrowding in hospitals (n=131, 77.5%). Frequent shortage of medicine and other supplies (n=124, 73.4%) and poor working conditions of doctors in hospitals (n=122, 72.2%) were also considered to be risk factors for workplace violence.
Discussion
Workplace violence is becoming an occupational health hazard among doctors. Our study revealed that 40.8% of resident doctors had experienced workplace violence in the past 12 months. This is much less than that reported by Ori et al. in 2014 in Manipur [15] where 78.3% of postgraduate students had faced at least one form of violence during their entire residency period. The duration of exposure, different definition of workplace violence and different geographical location may explain the difference between the two studies. However, the findings of our study are in line with the study conducted by Newman et al. in 2011 [17] in Uganda where 39% of health workers reported experiencing at least one form of workplace violence in the previous 12 months.
Verbal abuse (75.4%) was the most common form of violence followed by a threat. This finding too is consistent with studies done elsewhwere. [5] ,[15] ,[18] Though no gender difference was noted with the type of violence, a higher proportion of males faced physical violence and verbal abuse while females doctors were threatened. Our findings are similar to those by Kitaneh and Hamdam from Palestine [19] and a literature review from Portugual. [20] Gender appears to influence the pattern of workplace violence, its perpetration and victimization. [17]
In our study, more than three-fourths of affected resident doctors faced violence while they were working in the casualty. Many studies have recognized the emergency department as a particularly violent environment. [18] ,[19] ,[21] ,[22] These departments usually have patients who are critically ill and are accompanied by relatives who are anxious and stressed. Hence, they are more prone to aggression and violence if they feel that the patient was not attended to well. As in previous studies, [10] ,[11] ,[15] ,[18] ,[19] ,[20] patients and their relatives were frequently reported to be the main source of violence. Patients′ relatives should have realistic expectations of the course and outcome of illness. For this, treating doctors should explain to them the nature of the illness, the investigations needed, the possible line of management and probable course and outcome in a simple-to-understand manner. They should also provide periodic updates of the condition of the patient. [15] Perpetrators of violence are more likely to be males as reported by Eisele and colleagues. [23]
Another matter of growing concern is violence by co-workers or colleagues. About 26.1% of the affected doctors faced violence at the hands of their co-workers. Though we have not explored the reasons for this, understaffing, job stress and low job satisfaction are among the factors that might lead to aggression towards colleagues and co-workers as reported elsewhere. [19]
A higher proportion of doctors from the department of surgery experienced workplace violence compared to other departments. Evidence suggests that psychiatrists, emergency physicians and anaesthesiologists are often victims of violence followed by surgeons and internists. [18] Since our study sample did not include psychiatrists and anaesthesiologists, this finding should be interpreted with caution.
Work-related violence usually results in short- and long-term effects on the victims′ physical, psychological state and professional performance. [19] ,[24] ,[25] Adverse consequences of violence in our study were similar to those reported by others. [19] ,[26] Occupational violence has been associated with reduced productivity, increased turnover, absenteeism, counselling costs, decreased staff morale and reduced quality of life. [26] Further, some studies have shown that victims of violence at workplace can have adverse mental health outcomes such as acute stress disorder or post-traumatic stress disorder. [27] ,[28] Thus, there is an urgent need to institute policies and measures to deter violence in the health sector.
Violence remains an under-reported phenomenon. [18] In our study too, only one-third of doctors reported the event to higher authorities. Also, all those who did not report considered it a useless and time-wasting activity. This highlights the need to encourage reportage of violence among afflicted workers and to develop institutional mechanisms for speedy measures to avoid such events.
The states of Odisha, Maharashtra and Kerala had passed laws for punishment of workplace violence for medical services in 2008, 2009 and 2012, respectively. [15] ,[29] These legislations protect the rights of patients, doctors and hospital properties in the event of an attack. Only half of our respondents were aware of such legislations. However, the state of Delhi does not have a law for punishment of workplace violence for healthcare services.
Violence is a style of communication and conflict resolution; physicians are treated no different from anybody else. [9] Similar risk factors were perceived as physician risk factors in our study too. The patient risk factors were in line with those mentioned in the literature where intoxication, acute psychosis and personality disorders among patients or their relatives have been considered as risk factors for violence and aggression. [9] Other environmental or external factors include shortage of supplies and demands of work particularly in government settings, which make work conditions stressful and vulnerable to violence and aggression.
Limitations
Our study has a few limitations. It was done in only one hospital, and hence limits the generalization of our findings. Further, studies are warranted for physicians of other specializations, nurses and other healthcare providers (both community- and hospital-based). Participants self-reported violence and relevant exposures and hence there is a potential for bias. Attempts to minimize recall bias included limiting recall of violent events to the previous 12 months-an approach adopted in previous studies. [26] Our study depicts the perspective of violence in terms of physicians. Other stakeholder′s (including patients′) perspective was not taken into account.
Despite these limitations, our study provides an insight into the growing incidents of workplace violence among doctors in Delhi. It also highlights the potential risk factors perceived by our respondents that can serve as a basis for developing interventions to prevent and control workplace violence at healthcare delivery facilities. Further, there is a need to encourage reporting and follow-up on incidents as well as providing adequate physical and psychological support to victims of health workplace violence. [19]
| 1. | OSHA Fact Sheet. [Internet] 2002 Available at www.osha.gov/OshDoc/data_General_Facts/factsheet-workplace-violence.pdf (accessed on 24 Jul 2014). [Google Scholar] |
| 2. | Papa A, Venella J. Workplace violence in healthcare: Strategies for advocacy. Online J Issues Nursing 2013. doi: 10.3912/OJIN.Vol18No01Man05. [Google Scholar] |
| 3. | OSHA. Guidelines for preventing workplace violence for healthcare and social service workers. [Internet] 2004. U.S. Department of Labor, Occupational Safety and Health Administration, OSHA 3148-04R 2015. Available at www.osha.gov/Publications/osha3148.pdf (accessed on 27 Jul 2014). [Google Scholar] |
| 4. | Magin PJ, May J, McElduff P, Goode SM, Adams J, Cotter GL. Occupational violence in general practice: A whole-of-practice problem. Results of a cross-sectional study. Aust Health Rev 2011; 35: 75-80. [Google Scholar] |
| 5. | Kowalenko T, Walters BL, Khare RK, Compton S; Michigan College of Emergency Physicians Workplace Violence Task Force. Workplace violence: A survey of emergency physicians in the state of Michigan. Ann Emerg Med 2005; 46: 142-7. [Google Scholar] |
| 6. | Gates DM, Ross CS, McQueen L. Violence against emergency department workers. J Emerg Med 2006; 31: 331-7. [Google Scholar] |
| 7. | Carmi-Iluz T, Peleg R, Freud T, Shvartzman P. Verbal and physical violence towards hospital- and community-based physicians in the Negev: An observational study. BMC Health Serv Res 2005; 5: 54. [Google Scholar] |
| 8. | Chen Z, Peek-Asa C, Yang G. Prevalence of and risk factors associated with workplace violence: A cross-sectional study in 7026 health staff in South China. Inj Prev 2010; 16 (Suppl 1):A1-A289. [Google Scholar] |
| 9. | Morrison JL, Lantos JD, Levinson W. Aggression and violence directed towards physicians. J Gen Intern Med 1998; 13: 556-61. [Google Scholar] |
| 10. | Hesketh KL, Duncan SM, Estabrooks CA, Reimer MA, Giovannetti P, Hyndman K, et al. Workplace violence in Alberta and British Columbia hospitals. Health Policy 2003; 63: 311-21. [Google Scholar] |
| 11. | Martino VD. Workplace violence in the health sector: Country case studies. [Internet] 2002. Available at www.who.int/violence_injury_prevention/injury/en/WVsynthesisreport.pdf (accessed on 3 Aug 2014). [Google Scholar] |
| 12. | Balamurugan G, Jose TT, Nandakumar P. Patients′ violence towards nurses: A questionnaire survey. Int J Nursing 2012; 1: 1-7. [Google Scholar] |
| 13. | Pant S. Why are physical attacks on doctors commonplace in India [Internet] 2015. Available at www.huffingtonpost.in/dr-shubham-pant/ek-doctor-ki-maut-india a_b_7288100.html (accessed on 24 Sep 2015). [Google Scholar] |
| 14. | Dey S. Over 75% of the doctors have faced violence at work, a study finds. [Internet] 2015. Available at http://timesofindia.indiatimes.com/india/Over-75-of-doctors-have-faced-violence-at-work-study-finds/articleshow/47143806.cms (accessed on 24 Sep 2015). [Google Scholar] |
| 15. | Ori J, Devi NS, Singh AB, Thongam K, Padu J, Abhilesh R. Prevalence and attitude of workplace violence among the post graduate students in a tertiary hospital in Manipur. J Med Soc 2014; 28: 25-8. [Google Scholar] |
| 16. | Lok Nayak Jai Prakash Narayan Hospital. www.delhi.gov.in, Govt of NCT of Delhi, India. Available at http://delhi.gov.in/wps/wcm/connect/doit_lnjp/LNJP/Home/About+Us/ (accessed on 7 Aug 2014). [Google Scholar] |
| 17. | Newman CJ, de Vries DH, d′Arc Kanakuze J, Ngendahimana G. Workplace violence and gender discrimination in Rwanda′s health workforce: Increasing safety and gender equality. Hum Resour Health 2011; 9: 19. doi: 10.1186/1478-4491-9-19. [Google Scholar] |
| 18. | Arimatsu M, Wada K, Yoshikawa T, Oda S, Taniguchi H, Aizawa Y, Higashi T. An epidemiological study of work-related violence experienced by physicians who graduated from a medical school in Japan. J Occup Health 2008; 50: 357-61. [Google Scholar] |
| 19. | Kitaneh M, Hamdam N. Workplace violence against physicians and nurses in Palestinian public hospitals: A cross-sectional study. BMC Health Serv Res 2012; 12: 469. [Google Scholar] |
| 20. | Ferrinho P, Biscaia A, Fronteira I, Craveiro I, Antunes AR, Conceição C, et al. Patterns of perceptions of workplace violence in the Portuguese health care sector. Hum Resour Health 2003; 1: 11. [Google Scholar] |
| 21. | Fernandes CM, Bouthillette F, Raboud JM, Bullock L, Moore CF, Christenson JM, et al. Violence in the emergency department: A survey of health care workers. CMAJ 1999; 161: 1245-8. [Google Scholar] |
| 22. | Alameddine M, Kazzi A, El-Jardali F, Dimassi H, Maalouf S. Occupational violence at Lebanese emergency departments: Prevalence, characteristics and associated factors. J Occup Health 2011; 9: 455-64. [Google Scholar] |
| 23. | Eisele GR, Watkins JP, Matthews KO. Workplace violence at government sites. Am J Ind Med 1998; 33: 485-92. [Google Scholar] |
| 24. | Erkol H, Gökdoðan MR, Erkol Z, Boz B. Aggression and violence towards health care providers-a problem in Turkey? J Forensic Leg Med 2007; 14: 423-8. [Google Scholar] |
| 25. | Gillespie GL, Gates DM, Miller M, Howard PK. Workplace violence in healthcare settings: Risk factors and protective strategies. Rehabil Nurs 2010; 35: 177-84. [Google Scholar] |
| 26. | Gerberich SG, Church TR, McGovern PM, Hansen HE, Nachreiner NM, Geisser MS, et al. An epidemiological study of the magnitude and consequences of work related violence: The Minnesota Nurses′ Study. Occup Environ Med 2004; 61: 495-503. [Google Scholar] |
| 27. | Ryan JA, Poster EC. The assaulted nurse: Short-term and long-term responses. Arch Psychiatr Nurs 1989; 3: 323-31. [Google Scholar] |
| 28. | Levin PF, Hewitt JB, Misner ST. Insights of nurses about assault in hospital-based emergency departments. Image J Nurs Sch 1998; 30: 249-54. [Google Scholar] |
| 29. | Magar A. Violence against doctors in Nepal. J Nepal Med Assoc 2013; 52: I-II. [Google Scholar] |
Fulltext Views
6,942
PDF downloads
3,505




