Translate this page into:
Low-fidelity simulation to enhance understanding of infection control among undergraduate medical students
2 Central Research Services, Charutar Arogya Mandal, Karamsad 388325, Anand, Gujarat, India
Corresponding Author:
Ajay G Pathak
Central Research Services, Charutar Arogya Mandal, Karamsad 388325
India
ajaygp@charutarhealth.org
| How to cite this article: Singh SP, Modi CM, Patel CP, Pathak AG. Low-fidelity simulation to enhance understanding of infection control among undergraduate medical students. Natl Med J India 2017;30:215-218 |
Abstract
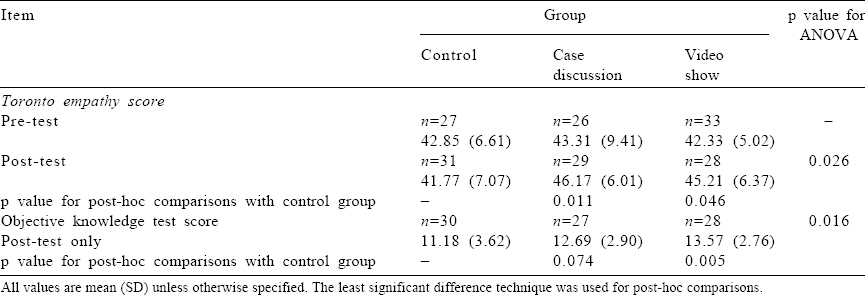
Background. Developing economies are stressing institutional care for better health outcomes but its advantages are dampened by healthcare-associated infections (HAIs). Besides other undesired complications, the economic cost of HAIs is enormous. Developing countries have higher HAI rates compared with Europe or the USA. The knowledge and practice of infection control is poor among medical students. Based on introspection of ‘Infection Control Module’ for undergraduates introduced in 2012, we tested emotional sensitization using low-fidelity techniques to enhance its effectiveness.Methods. All medical undergraduate students in their second year (n=102) were randomly divided into three groups using balanced randomization (two test and one control). Test groups were made to realize the emotional, social and financial consequences of HAI on patients and their families through low-fidelity simulation in the form of case discussions and video demonstrations. Pre- and postintervention empathy scores were calculated using Toronto empathy questionnaire (TEQ) for all the 102 students. Postintervention, all students were subjected to an infection control module and knowledge test. Perceptions of the intervention groups were recorded. Descriptive statistics and ANOVA were applied for data analysis.
Results. Of the 102 students, 93 (91.1%) participated in the study. There was no significant difference in the pre-test TEQ score (p=0.87) but there was a significant difference in the post-test TEQ (p = 0.026) and knowledge test score (p = 0.016) among the groups. Both the simulation exercises were well appreciated by the students.
Conclusion. Emotional sensitization using low-fidelity simulation served as a catalyst in understanding infection control among medical undergraduate students.
Introduction
Quality is an integral part of healthcare. A conceptual framework elaborating different dimensions of quality of care[1] and ways to achieve it led by clinicians has been formulated.[2],[3] Though an important quality indicator, healthcare-associated infections (HAIs) remain the most common complication in hospitalized patients.[4] Based on limited data, developing countries report higher HAI rates compared with those in Europe or the USA and this gap widens further in intensive care units.[5] Besides other undesired implications, the economic cost of HAI is high and is a driving force to address HAI through a business model.[6],[7]
Lack of adequate knowledge coupled with poor adherence to infection control protocols is a universal phenomenon among medical students.[8],[9],[10],[11] WHO has developed a comprehensive thematic framework and technical tools addressing patient safety including a curriculum guide.[12] Considering medical students as future leaders and role models in inculcating culture, it is imperative to empower medical students about infection control and instil the culture of adherence to protocols among them. Various educational approaches such as lectures, case discussion, special interdisciplinary modules as well as e-learning modules are used to empower medical students as well as allied health workers about infection control.[13],[14],[15]
In the absence of an established formal curriculum in India, we introduced an ‘Infection control module’ for undergraduate students in the year 2012.[16] Formal as well as informal feedback of students and introspection of the process indicated a need to incorporate ‘real-life experience’ in the module. The aim was to influence the affective domain and generate empathy for patients. For practical as well as ethical reasons, it was not possible to provide a ‘real-life experience’ in the hospital.
Simulation is the imitation of the operation of a real-world process or system over time. The utility of simulation in medical education without inherent risk associated with a real-life experience has been established.[17],[18] Absence and impracticality of high-fidelity simulators for infection control and remembering the guiding principle: ‘Simulation is a technique not technology’, we tried low-fidelity simulation techniques (LFST) to improve the module. The students were sensitized using a LFST in the form of case discussions and a video show before the infection control module to check whether the sensitization process acted as a catalyst in their learning.
Methods
The educational intervention was designed as a randomized controlled trial and implemented for a batch of 102 students in their second year MBBS in September 2014. The students were divided into three groups: (i) control group; (ii) video show group (VSG); and (iii) case discussion group (CDG) using the block randomization method. The students were oriented about the intervention and verbal consent was obtained. The institutional ethics committee approved the study with instructions to conduct the study anonymously.
The VSG group was made to realize the importance of preventing HAI and its impact on patient, family and institution with six videos (downloaded from YouTube) depicting experiences of people who suffered from HAI and its consequences. This was followed by a classroom discussion on the various issues and an interactive slideshow. The CDG was further divided into three small groups of 9–10 students and given separate paper case histories for discussion in groups followed by reflections and discussion with the whole group. Case histories were adopted from the WHO patient safety curriculum guide for medical schools with some modification.[12]
In both the VSG and CDG, the following discussion themes were used: Put yourself in place of X and feel what would be your reaction when you come to know about the incident? What would be the impact of this incident on your life when you are detected with HAI? Was this a preventable tragedy? Are you in a position to save such damages? What are the promises you make to yourself as a future doctor to prevent such incidents? These themes were meant to help students empathize with patients and realize the importance of compliance to infection control practices. Both groups had a trained faculty as facilitator. These sessions were conducted simultaneously. Students in the control group were not exposed to any of the above sensitizations.
The Toronto empathy questionnaire (TEQ) was administered to the three groups a week before the sensitization intervention. The TEQ contains 16 questions that encompass a wide range of attributes associated with theoretical facets of empathy such as emotional contagion, emotional comprehension, sympathetic physiological arousal, higher-order empathic responding, such as pro-social helping behaviours and altruism. Scoring of the items depends upon the nature of items. Positively worded items (No. 1, 3, 5, 6, 8, 9, 13, 16) were scored as Never 0; Rarely 1; Sometimes 2; Often 3; Always 4. The negatively worded items (No. 2, 4, 7, 10, 11, 12, 14, 15) were reverse scored. Scores were summed to derive the total for the TEQ score.[19]
After sensitization of test groups through LFST, all students went through a 4.5-hour infection control module spread over four sessions in a week. The module focused on delivery of knowledge and skills related to key areas in infection control, i.e. defining and identifying HAI, chain of transmission and strategies to break it with appropriate application of their knowledge about standard precautions, sterilization and disinfection of environment and patient care instruments, spillage management, biomedical waste management and needle stick injury. The specific learning objectives for these sessions were identified after discussion among members of the hospital infection control committee and clinicians. These objectives were communicated to the students at the beginning of the session. Combinations of teaching learning methods such as interactive lectures, video show and demonstration were used for delivery.
An anonymous written test assessing knowledge in the form of objective questions (multiple-choice questions and fill in the blanks with 22 items) was conducted for all students at the end of the module. The TEQ was also administered at the end of the course. At the same time, perceptions of students towards LFST as well as the module (VSG and CDG only) were recorded in the form of an anonymous semi-structured feedback questionnaire with 15 statements. The statements were framed to assess the overall planning, organization, conduct and involvement of students in the infection control module along with effectiveness of LFST in sensitizing their emotions or empathy towards patients and relatives of patients with HAI and its effect on their future compliance to infection control protocols.
Statistical Analysis
Descriptive statistics were used to depict the characteristics of the study population and the students’ perceptions about LFST. The analysis of variance (ANOVA) was used to compare the post-intervention knowledge and empathy of the participants (TEQ) in the three groups. In the absence of identifiers, ANOVA on difference scores was not possible.
Results
Of the 102 students, 93 (91.1%) participated in the study. The TEQ data of 86 (92.5%) students on pre-test (control 27, CDG 26 and VSG 33) and 88 (94.6%) students on post-test (control 31, CDG 29 and VSG 28) were available for analysis. The written test was completed by 85 (91.4%) students (control 30, CDG 27 and VSG 28) after learning the infection control module. Feedback responses from 50 (CDG 24 and VSG 26) of 62 students (80.6%) in intervention groups were available for analysis.
Toronto empathy questionnaire (TEQ)
The pre-test TEQ score was similar in the three groups (p = 0.87). A significant difference was observed in the post-test TEQ score among the groups (p = 0.026). Post-hoc analysis revealed that CDG (p = 0.011) as well as VSG (p = 0.046) had significantly better empathy scores as compared to the control group [Table - 1] and [Figure - 1].
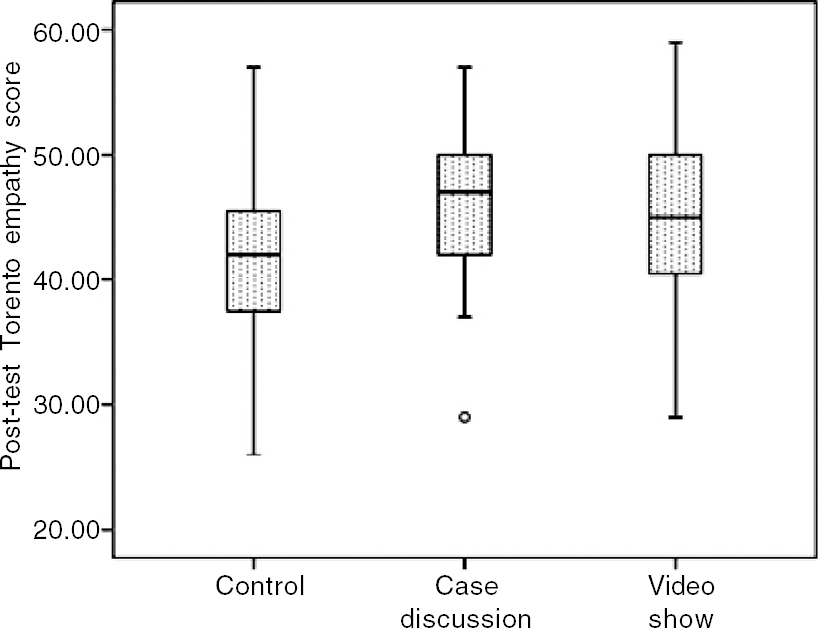 |
| Figure 1: Box plot showing distribution of post-test Toronto empathy scores |
Knowledge test
A significant difference was observed in the performance on objective knowledge test among the groups (p = 0.016). Posthoc analysis revealed that the CDG (p = 0.074) fared similar but the VSG (p = 0.005) performed significantly better compared with the control group [Table - 1] and [Figure - 2].
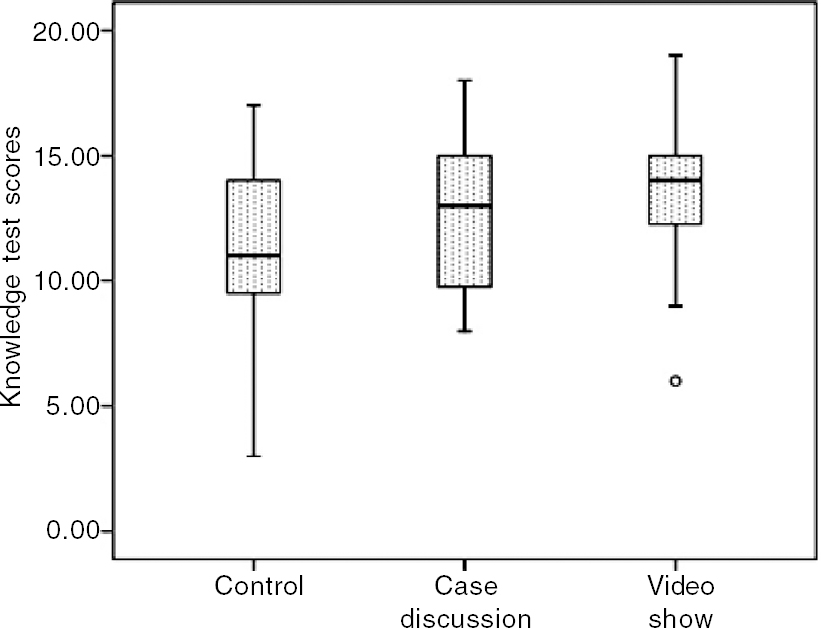 |
| Figure 2: Box plot showing distribution of multiple-choice question scores |
General perceptions about sensitization exercise (LFST) and infection control module
Over 90% of students felt that the module was well-planned, logically sequenced, relevant and useful with clearly communicated learning objectives. Cases selected were found to be interesting and appropriate for the sensitization in both CDG and VSG (91.7% and 96.2%). Time allotted for the case discussions was found to be optimum by 70.8% students in CDG and 96.2% in VSG. All students in the CDG and 88.5% in VSG felt that the session helped them assess the impact of HAI on patients’ emotional, financial and social life and this helped them understand the difficulties faced by a patient and their relatives due to non-compliance to certain protocols. The majority of students (95.8%) thought the case discussion provided them an opportunity to explore their thoughts and emotions about patients’ suffering, which was felt by only 80.8% of students in the VSG group. Compared to CDG, students in VSG enjoyed the process more (92.3% v. 87.5%). Only 53.8% students in the VSG group felt they would be able to motivate their friends and colleagues towards better compliance as compared to 75% in the CDG group.
All students in both intervention groups reported that their attitude towards infection control had changed for the better due to the sensitization exercise. Skill development was not achieved through this module as only 75% and 65.4% students in CDG and VSG, respectively, felt more skilful after the module [Table - 2].
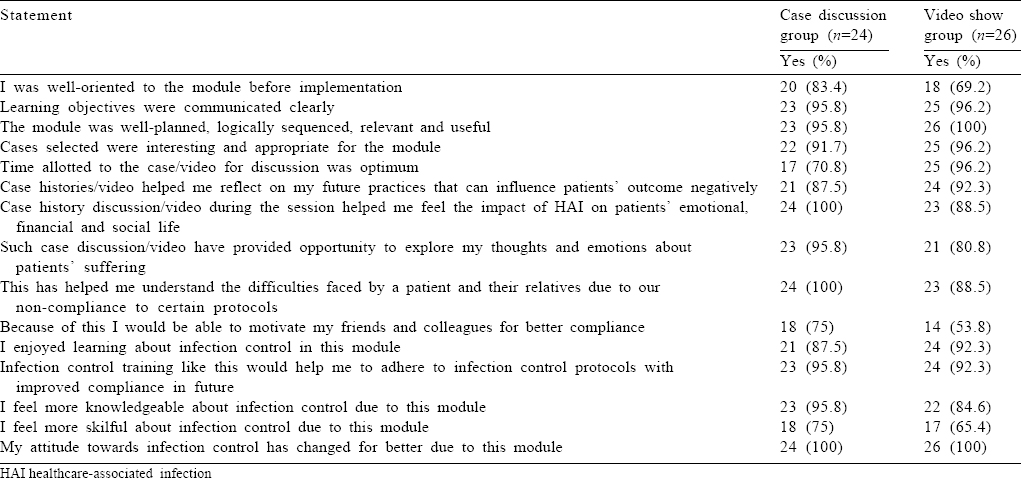
Overall, both sensitization exercises (LFST) were well appreciated and accepted by the students though case discussions were felt to be more stimulating compared to the video show. There is scope for improvement related to orientation before the intervention. Students also reported lack of confidence in acquisition of required skills, which needs to be emphasized in future modules.
Discussion
While developed economies are moving from institutional care to home care, developing economies such as India are stressing on institutional care for better health outcomes. The advantages of institutional care will be dampened if hospitals are not safe. Adherence to infection control protocols particularly hand hygiene has been identified as an intervention that can reduce infection rates by as much as 50%. However, poor compliance with interventions has been a universal phenomenon across all cadres of healthcare workers.[12] The need for more organized and formal curriculum to improve knowledge, skills and attitudes of undergraduate students has also been identified due to poor state of knowledge and skills in various studies conducted worldwide.[8],[9],[10],[11],[12]
The WHO patient safety curriculum guide for medical schools has suggested using problems or cases to enhance students understanding about various issues related to infection control.[12] Based on these recommendations and to make students more receptive to the technical aspects of infection control, we stimulated the emotions of students through exposing them to low-fidelity simulation in the form of case histories and videos highlighting the emotional, financial and social problems faced by relatives and patients. This was done to help them experience and later reflect on the issues. The aim was to make them understand the impact of their act of ignorance or carelessness in compliance with infection control practices on someone else’s life. The timing of such sensitization followed by the infection control module was chosen so that students could incorporate the knowledge during their clerkship and ward posting with some reinforcement.
While most studies show improvement in knowledge and attitudes towards infection control protocols after an educational intervention,[12][13],[14],[15],[16] the retention of practices was not encouraging,[14] which highlights the importance of ‘team work’ and reinforcement with supportive supervision till adherence becomes a culture.
Our study provides the basis for such cultural transformation though it should be followed by infrastructural support and clearly defined protocols coupled with active surveillance by the peers.
As instructed by our institutional ethics committee, we conducted the study without identifiers of the students. We, therefore, could not perform a pre–post comparison on different scores and hence the results are indicative but not confirmatory. Further, an appropriate and validated scale in healthcare setting such as ‘The Jefferson Scale of Empathy (JSE)’ was not used due to cost constraints; instead we used a free questionnaire. The TEQ was used to determine empathy. This general questionnaire may not be apt to measure empathy in healthcare settings.
Further, our study shows the impact of emotional sensitization on understanding (knowledge) of the participants as there was no opportunity to capture practices at this time point (the participants were second year students). However, we believe that people who are empowered as well as emotionally sensitized are more likely to follow the guidelines. We intend to follow these students through their clerkship to see the long-term impact of the simulation. The sample size per group was just sufficient but medical colleges with an intake of over 150 students per year may show the effect with more confidence.
With the above limitations, we believe that sensitization with low-fidelity simulation has a beneficial effect in learning.
Contributions
SS and CM conceived the study. AP and CP did the literature review. All authors contributed to the design of the study. SS, CP and CM collected the data. AP analysed the data and interpreted the findings. AP and CP wrote the manuscript. SS and CM provided intellectual inputs to the manuscript. The final draft was approved by all the authors.
| 1. | Panchapakesan P, Chandrasekharan R, Prakash Sai L. A conceptual framework of service quality in healthcare: Perspectives of Indian patients and their attendants. Benchmarking: An International Journal 2009;16:157-91. doi.org/10.1108/14635770910948213. [Google Scholar] |
| 2. | Ramanuj PP, Ryland H, Mitchell EW, Parvizi N, Chinthapalli K. In the spotlight: Healthcare inspections as an opportunity for trainee clinicians to be the leaders of today. BMJ Qual Saf 2014;23:624-8. [Google Scholar] |
| 3. | Runnacles J, Moult B, Lachman P. Developing future clinical leaders for quality improvement: Experience from a London children’s hospital. BMJ Qual Saf 2013;22:956-63. [Google Scholar] |
| 4. | Ostrowsky B. Epidemiology of healthcare-associated infections. In: Jarvis WR (ed). Bennett and Brachman’s Hospital Infections. 5th ed. Philadelphia:Lippincott Williams & Wilkins; 2007:3-24. [Google Scholar] |
| 5. | Allegranzi B, Nejad SB, Combescure C, Graafmans W, Attar H, Donaldson L, et al. Burden of endemic health-care-associated infection in developing countries: Systematic review and meta-analysis. Lancet 2011;377:228-41. [Google Scholar] |
| 6. | Anderson DJ, Kirkland KB, Kaye KS, Thacker PA 2nd, Kanafani ZA, Auten G, et al. Under resourced hospital infection control and prevention programs: Penny wise, pound foolish? Infect Control Hosp Epidemiol 2007;28:767-73. [Google Scholar] |
| 7. | Sheng WH, Wang JT, Lu DC, Chie WC, Chen YC, Chang SC. Comparative impact of hospital-acquired infections on medical costs, length of hospital stay and outcome between community hospitals and medical centres. J Hosp Infect 2005;59:205-14. [Google Scholar] |
| 8. | Ayub A, Goyal A, Kotwal A, Kulkarni A, Kotwal A, Mahen A. Infection control practices in health care: Teaching and learning requirements of medical undergraduates. Med J Armed Forces India 2013;69:107-12. [Google Scholar] |
| 9. | Amin TT, Al Noaim KI, Saad MAB, Al Malhm TA, Al Mulhim AA, Al Awas MA. Standard precautions and infection control, medical students’ knowledge and behaviour at a Saudi University: The need for change. Glob J Health Sci 2013;5:114-25. [Google Scholar] |
| 10. | Huang Y, Xie W, Zeng J, Law F, Ba-Thein W. Limited knowledge and practice of Chinese medical students regarding health-care associated infections. J Infect Dev Ctries 2013;7:144-51. [Google Scholar] |
| 11. | Legeay C, Thépot-Seegers V, Groh M, Pilmis B, Zahar JR. Medical students’ knowledge of infection control and prevention: Factors associated with better results and room for improvement. Am J Infect Control 2015;43:1142-3. [Google Scholar] |
| 12. | World Health Organization. WHO patient safety curriculum guide for medical students; 2009. Available at www.who.int/patientsafety/education/curriculum_guide_medical_schools/en/ (accessed on 22 Nov 2015). [Google Scholar] |
| 13. | O’Brien D, Richards J, Walton KE, Phillips MG, Humphreys H. Survey of teaching/learning of healthcare-associated infections in UK and Irish medical schools. J Hosp Infect 2009;73:171-5. [Google Scholar] |
| 14. | Wagner DP, Parker CJ, Mavis BE, Smith MK. An interdisciplinary infection control education intervention: Necessary but not sufficient. J Grad Med Educ 2011;3:203-10. [Google Scholar] |
| 15. | O’Neill E, Stevens NT, Clarke E, Cox P, O’Malley B, Humphreys H. Use of elearning to enhance medical students’ understanding and knowledge of healthcareassociated infection prevention and control. J Hosp Infect 2011;79:368-70. [Google Scholar] |
| 16. | Singh SP, Modi C, Patel C, Patel P. Introduction of infection control module for undergraduate medical students: Experience at a rural medical college in India. Int J Infect Control 2014;10(3). doi: http://dx.doi.org/10.3396/ijic.v10i3.12714. [Google Scholar] |
| 17. | Datta R, Upadhyay K, Jaideep C. Simulation and its role in medical education. Med J Armed Forces India 2012;68:167-72. [Google Scholar] |
| 18. | Okuda Y, Bryson EO, DeMaria S Jr, Jacobson L, Quinones J, Shen B, et al. The utility of simulation in medical education: What is the evidence? Mt Sinai J Med 2009;76:330-43. [Google Scholar] |
| 19. | Spreng RN, McKinnon MC, Mar RA, Levine B. The Toronto Empathy Questionnaire: Scale development and initial validation of a factor-analytic solution to multiple empathy measures. J Pers Assess 2009;91:62-71. [Google Scholar] |
Fulltext Views
1,571
PDF downloads
537




