Translate this page into:
Cancer care continuum at a tertiary care centre in India during the Covid-19 pandemic and nationwide lockdown: Healthcare delivery through telemedicine
Correspondence to RAJENDRA A. BADWE; badwera@tmc.gov.in
[To cite: Gokarn A, Joshi A, Wadasadawala T, Gulia S, Wakle S, Singh A, et al. Cancer care continuum at a tertiary care centre in India during the Covid-19 pandemic and nationwide lockdown: Healthcare delivery through telemedicine. Natl Med J India 2022;35:142–6.]
Abstract
Background
The Covid-19 pandemic and subsequent lockdown in India caused disruptions in cancer treatment due to the restriction on movement of patients. We aimed to maintain continuity in cancer treatment during the lockdown through teleconsultations. We tried to reach out to our patients using telephonic consultations by establishing a Teleconsult Centre facility run by a team of doctors and patient navigators.
Methods
We telephonically contacted all patients who had outpatient appointments from 23 March to 30 April 2020 at our centre through the Teleconsult Centre to understand their current circumstances, feasibility of follow-up, local resources and offered best possible alternatives to continue cancer treatment, if required.
Results
Of the 2686 patients scheduled for follow-up during this period, we could contact 1783 patients in 9 working days. Through teleconsultations, we could defer follow-ups of 1034 patients (57.99%, 95% confidence interval [CI] 55.6%–60.3%), thus reducing the need for patients to travel to the hospital. Change in systemic therapy was made in 75 patients (4.2%, 95% CI 3.3%–5.2%) as per the requirements and available resources. Symptoms suggestive of disease progression were picked up in 12 patients (0.67%, 95% CI 0.35%–1.17%), who were advised to meet local physicians.
Conclusion
Our study suggests that the majority of patients on follow-up can be managed with teleconsultation in times of crisis. Teleconsultation has the potential of being one of the standard methods of patient follow-up even during periods of normalcy.
INTRODUCTION
Novel coronavirus (2019-nCoV), also known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) originated from China around December 2019.1 Infection with this virus leading to coronavirus disease 2019 (Covid-19) was declared a pandemic by the WHO as it had infected >1 million people globally with approximately 70 thousand deaths till the end of the first week of April 2020.2 The number of cases in India gradually rose since March 2020 and the Government of India declared complete lockdown in the country from the midnight of 25 March 2020. This posed several challenges in the delivery of cancer treatment because patients were unable to visit the cancer treatment facility, procure necessary drugs or reach the cancer care-provider locally for continuation of treatment. The oncologist had to strike a balance between under-treatment of cancer, with resultant increase in cancer-related mortality and mortality due to Covid-19 in the vulnerable cancer patient. Various international organizations had published cancer treatment guidelines based on the disease stage, taking into account potential benefits versus risk of cancer treatment during the Covid-19 crisis. However, these were not based on robust evidence.3–5
Telemedicine had emerged as an important mode of communicating with our patients in this situation. The Ministry of Health and Family Welfare, Government of India, also accepted telemedicine as an alternative to outpatient consultation in the Covid-19 pandemic scenario to avoid direct contact between patients and physicians, and maintain social distancing.6
Tata Memorial Centre (TMC) in Mumbai is the largest tertiary cancer hospital in India. It treats approximately 50 000 new cancer patients annually. It has a dedicated residency programme for training doctors in surgical, medical and radiation oncology. TMC also runs a 1-year, full-time diploma programme in patient navigation (KEVAT), which trains personnel in patient navigation and communication. To reach out to our cancer patients, we decided to establish a Teleconsult Centre during the Covid-19 lockdown period. We describe the observations and experience of our teleconsultations at TMC during the Covid-19 lockdown.
METHODS
To facilitate teleconsultation, a dedicated Teleconsult Centre facility was created on the campus of the Advanced Centre for Treatment Research and Education in Cancer (ACTREC) branch of TMC. The goals of the Teleconsult Centre were to:
establish contact with the patient;
allay anxiety regarding continuity of treatment in the lockdown period;
provide a medium for patients to communicate with doctors at TMC; and
find the most practical solution for continuing the best possible treatment while reducing the footfall at TMC so as to avoid overcrowding during the Covid-19 lockdown.
The constitutional framework of the facility is shown in Fig. 1. This Teleconsult Centre was grouped into four teams, each comprising a resident doctor (from surgical oncology, medical oncology and radiation departments) and a patient navigator. The facility was supervised full-time by a consultant from each of the above disciplines, to facilitate quick decision-making at the time of teleconsultation. Dedicated computers were used for accessing electronic medical records and mobile phones were used for making calls to cancer patients. The list of patients scheduled for visits from five Disease Management Groups (i.e. breast cancer, gastrointestinal [GI], gynaecological, adult haematolymphoid and head-and-neck cancers) from 23 March 2020 to 30 April 2020 was retrieved from the medical records department. This list provided phone numbers and email addresses of patients if available. Standard operating procedures (SOPs) were developed anticipating different clinical scenarios and their probable interventions as per the stage of the disease and ongoing treatment. Table I summarizes the SOPs defined for each disease site, which were broadly categorized into six scenarios. The teleconsultation call was made by a doctor. During the teleconsultation, patients were questioned about their general health status and issues that they were facing in receiving cancer treatment and a viable alternative was given to them in case their treatment was hampered by the lockdown. The teleconsultation was documented in the hospital electronic medical record as well as in a separate data sheet in Microsoft Excel format. Each patient was given the mobile number of the Teleconsult Centre and an email address for further communication with the treating oncologist. Patients who were on clinical trials were given contact numbers of respective trial coordinators for communication. Email queries were responded to within 24 hours.
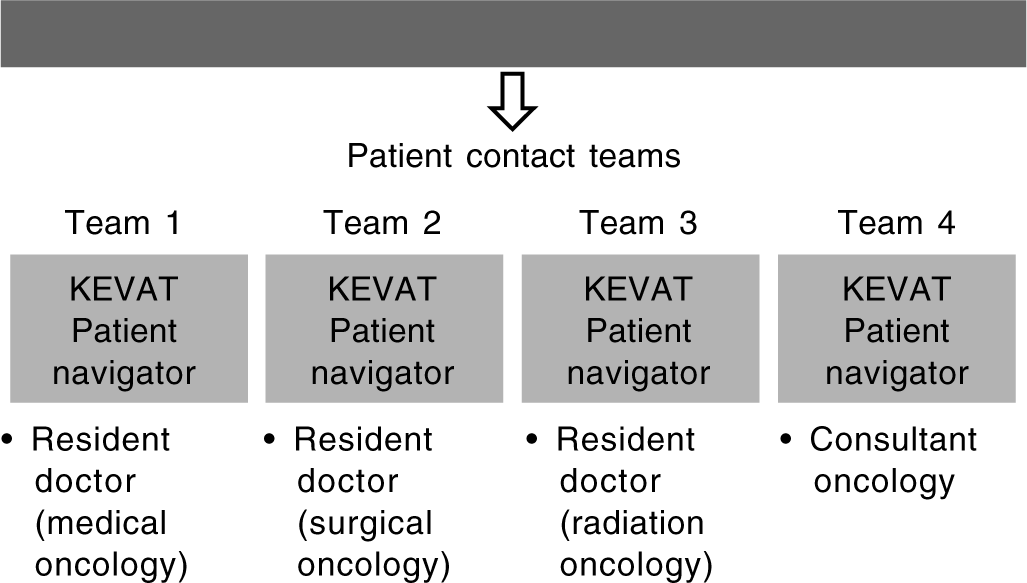
- The constitutional framework of the Teleconsult Centre at Tata Memorial Centre
| Scenario | Breast cancer | Adult haemato-lymphoid cancer | Gynaecological cancer | Gastrointestinal cancer | Head-neck cancer |
|---|---|---|---|---|---|
| 1 | Completed primary treatment and on follow- up; if well, review after 4 months | Completed treatment and on follow-up; if well, review after 4 months | Completed treatment and on follow-up; if well, review after 4 months | Completed treatment and on follow up. If well, review after 4 months | Completed treatment and on follow-up. If well, review after 4 months |
| 2 | On chemotherapy in Mumbai; to postpone chemotherapy by 2 weeks | Acute lymphoblastic leukemia patients on maintenance; to continue current dose of maintenance; to review after 2 months | On chemotherapy in Mumbai; to postpone chemotherapy by 2 weeks | On chemotherapy in Mumbai; to postpone chemotherapy by 2 weeks | On follow-up have features indicative of recurrence: consult local oncologist. If not possible, review in 15 days |
| 3 | On chemotherapy (adjuvant) and doing well (outside Mumbai); complete chemotherapy and review after 2 months | Acute leukaemia/high- grade lymphoma patients on intensive curative chemotherapy treatment; to continue treatment with treating oncologist | On chemotherapy (adjuvant) and doing well (outside Mumbai); complete chemotherapy and review after 1–2 months | On chemotherapy (adjuvant) and doing well (outside Mumbai): complete chemotherapy and review after 1–2 months | Immediate postoperative case: ask about wound problems (if yes, staying nearby, visit hospital, else consult local surgical oncologist); discuss the need for adjuvant treatment (guide to local oncology centre) |
| 4 | On chemotherapy (neoadjuvant) with surgery planned; to confirm delay with surgeons. If delay confirmed, then complete neoadjuvant at local place, consider total neoadjuvant approach with due risk | CML patients: to continue same dose of TKI; may follow-up after 2 months; can purchase tablets from local place if available | On chemotherapy (neoadjuvant) with surgery planned with dates given; to confirm delay with surgeons. If delay confirmed, then complete neoadjuvant at local place | On chemotherapy (neoadjuvant) with surgery planned with dates given: to confirm delay with surgeons. If delay confirmed, then complete neoadjuvant at local place | On adjuvant treatment and doing well (outside Mumbai): complete therapy; review after 3 months |
| 5 | On palliative chemotherapy and doing well, consider 2–3 more cycles of chemotherapy with local oncologist | Low-grade lymphoma on chemotherapy; preferable to withhold chemotherapy for 1 month | On palliative chemotherapy: if doing well in terms of tolerance and improvement symptomatically, consider 2–3 more cycles of chemotherapy with local oncologist | On palliative chemotherapy: if doing well, consider 2–3 more cycles of chemotherapy with local oncologist | On palliative chemotherapy: if doing well, consider 2–3 more cycles of chemotherapy with local oncologist |
| 6 | On palliative chemotherapy with increasing symptoms or poor tolerance; to consider dose modifications or change in treatment; to meet local oncologist | Multiple myeloma on chemotherapy; may continue current therapy at local place; to delay follow-up by 1 month | On palliative chemotherapy, if having increasing symptoms or poor tolerance, to consider dose modifications or change in treatment; to meet local oncologist | On palliative chemotherapy: if having increasing symptoms or poor tolerance, to consider dose modifications or change in treatment; to meet local oncologist | On palliative chemotherapy: if having increasing symptoms or poor tolerance, to consider dose modifications or change in treatment; to meet local oncologist |
TKI tyrosine kinase inhibitor CML chronic myeloid leukaemia
For patients with breast cancer who could not visit the hospital due to the lockdown, we decided to delay chemotherapy by 2–4 weeks in adjuvant and neoadjuvant chemotherapy settings. Those patients who lived far away but had access to cancer therapy nearby were advised to continue treatment at local places. Patients with hormone receptor-positive breast cancer, who had absolutely no access to travel or local healthcare facilities and were on palliative intent chemotherapy, were started on oral hormonal therapy wherever feasible. Radiotherapy was withheld for patients with only 1–3 lymph node positivity post-mastectomy, who had intermediate risk of local recurrence.
Similarly, for patients with GI and gynaecological cancers, those who were on neoadjuvant or adjuvant chemotherapy and could not reach TMC due to the lockdown were advised to postpone chemotherapy by 2 weeks. Those who were on adjuvant chemotherapy and had access to facilities at their local place were advised to complete the course of chemotherapy and follow-up after 1 month. Patients with head-and-neck cancer, who were on palliative chemotherapies, were shifted to oral metronomic chemotherapies and asked to continue these at local places till their next possible follow-ups. Patients who had lately undergone surgery were advised to consult local surgeons for wound care. All patients who were planned for radiotherapy but could not reach TMC were asked to take radiotherapy at local place wherever feasible or delay by 2–4 weeks if the immediate start of radiation was not possible. The referral protocol for radiation planning was generated, and patients were asked to access the same with their own login from the web-based electronic medical record available on the institute website. Patients with haematological malignancies, who were on follow-up and doing well, were asked to defer the follow-up visit by 3 months. Patients with acute lymphoblastic leukaemia, who were on maintenance therapy, were asked to continue the same maintenance dose of medications till their next follow-up post-lockdown. Patients with low-grade lymphomas were advised to withhold chemotherapy for 1 month. Patients with multiple myeloma, who could not attend outpatient department (OPD) and were on oral medications (thalidomide/lenalidomide), were asked to continue therapy and delay OPD visits. A follow-up plan was also given to each patient (Fig. 2).
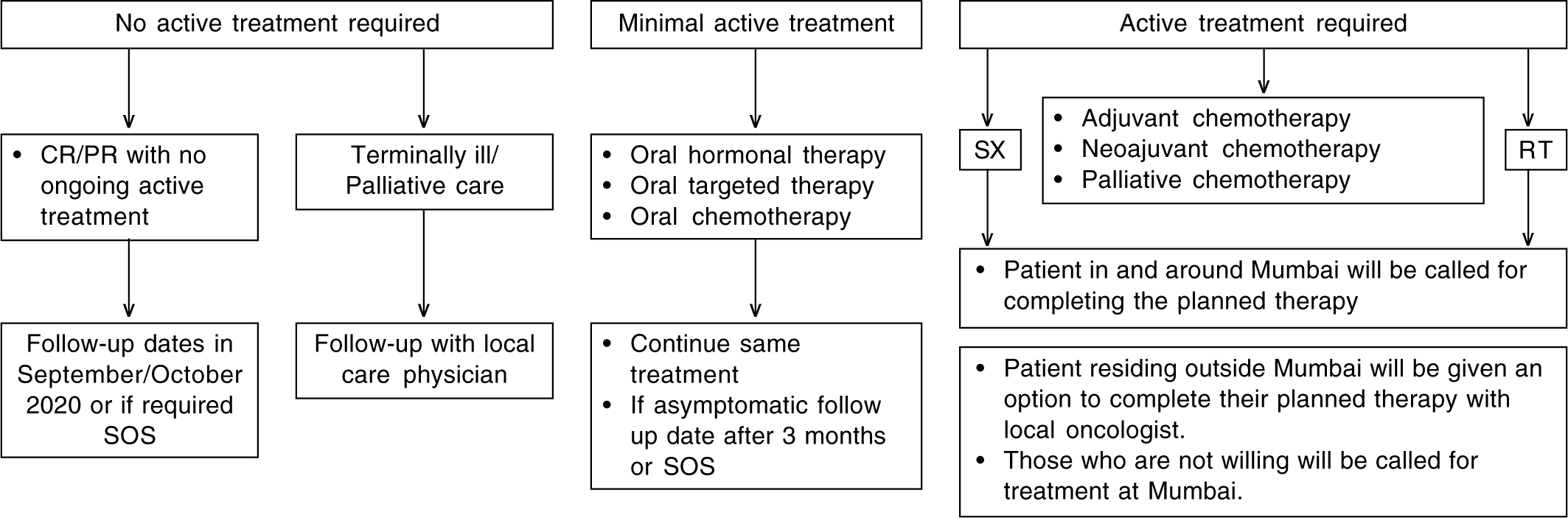
- Follow-up plan for patients post-Covid-19 lockdown CR/PR complete remission/partial remission Sx surgery RT radiotherapy
RESULTS
Teleconsultations were done from 9.30 a.m. to 5.30 p.m. on weekdays between 23 March and 30 April 2020. A total of 2686 cancer patients, who had appointments between 23 March and 30 April 2020 were called from the Teleconsult Centre. Of these, communication could be established with 1783 patients. The remaining patients could not be reached even on a repeat attempt. Each telephone call attempted was documented in the electronic medical records. The scenario-wise split of the data is shown in Table II. The disease-wise results are presented below.
| Scenario | Breast (n=513) | Haemato-lymphoid (n=280) | Gynaecological (n=138) | Gastrointestinal (n=635) | Head-neck (n=72) | Total (n=1638) |
|---|---|---|---|---|---|---|
| 1 | 185 | 16 | 89 | 133 | 48 | 471 |
| 2 | 73 | 20 | 11 | 175 | 11 | 290 |
| 3 | 80 | 5 | 10 | 74 | 8 | 177 |
| 4 | 11 | 194 | 3 | 20 | 2 | 230 |
| 5 | 139 | 3 | 12 | 194 | 1 | 349 |
| 6 | 16 | 39 | 4 | 27 | 2 | 88 |
| Patients in clinical trials | 5 | 2 | 9 | 3 | 0 | 19 |
| Patients expired | 4 | 1 | 0 | 9 | 0 | 14 |
Apart from the 1638 patients mentioned above, there were 8 patients with neurological cancers, 39 children with cancer and 98 patients with lung cancers who were called (total n=1783)
Breast cancer
Teleconsultation was done for 513 breast cancer patients, of which 185 (36.06%) were in scenario 1 (completed their primary treatments). Of these 185 patients, 72 (14.03%) were on no treatment, whereas 91 (17.7%) were on adjuvant hormonal therapy and 22 (4.28%) were on adjuvant maintenance trastuzumab. Of all the breast cancer patients included in the analysis, 52 (10.14%, 95% confidence interval [CI] 7.66%– 13.08%) were advised change in treatment including 43 (8.38%, 95% CI 6.13%–11.12%) requiring a change in chemotherapy (23 in adjuvant, 7 in neoadjuvant and 13 in palliative chemotherapy), 7 (1.36%, 95% CI 0.55%–2.79%) a delay in adjuvant trastuzumab by >3 weeks and 2 (0.39%, 95% CI 0.05%–1.4%) a delay in adjuvant radiotherapy.
Gynaecological cancer
Among the 138 patients with gynaecological malignancies, treatment was changed in 6 (4.35%, 95% CI 1.61%–9.22%) patients through teleconsultation including concurrent chemotherapy in carcinoma cervix being omitted in 2 patients due to the absence of infrastructure and delay in starting of radiotherapy by 2 weeks in 4 patients.
Head-and-neck cancer
Among the 72 patients with head-and-neck cancer, 14 patients (19.44%, 95% CI 11.06%–30.47%) required modification in treatment including 1 patient who was shifted to oral metronomic therapy because of delay in surgery, 12 patients had to delay palliative chemotherapies by 2 weeks, whereas 1 patient with carcinoma buccal mucosa was advised to undergo surgery at a nearby centre.
Haematological malignancy
Of the 394 patients of chronic myeloid leukaemia who had appointments during this period, telephonic contact could be established with 194 patients (49%). Efforts were made to supply them with tyrosine kinase inhibitors (TKI), mainly imatinib, through various sources, including patient assist programmes. Of these 194, a follow-up call was made to 66 patients (16.75%) of whom 35 (8.8%) could procure medicines. The remainder could not access medications because of the following reasons: 8 (2.03%) due to financial reasons, 21 (5.32%) due to non-availability of drugs in local pharmacies and 2 (0.5%) could not have the medicines couriered to their home towns due to the absence of courier services. Of these 21 patients, 6 were from Uttar Pradesh, 5 were from Maharashtra, 3 each were from Bihar and West Bengal, 2 were from Madhya Pradesh and 1 each from Jharkhand and Assam. Three patients with low-grade lymphomas were advised to delay chemotherapy by 1 month due to the lockdown and low-grade nature of malignancy.
Overall, follow-up was deferred in 1034 (57.99%, 95% CI 55.6%–60.3%) of the 1783 patients contacted. These were patients who were on oral palliative therapy (e.g. TKIs, hormonal therapy, oral metronomic therapy, etc.), palliative chemotherapy or on surveillance following completion of planned therapy and were doing well in terms of symptom control and treatment tolerance. They were all asked to delay follow-up visits by 3–4 months.
Telephonic conversations could pick symptoms suggestive of disease progression in a total of 12 patients (0.67%, 95% CI 0.35%–1.17%) including 3 breast cancer, 6 head-and-neck cancer, 2 with gynaecological malignancies and 1 GI cancer patients.
Suggestions to meet local physicians/oncologist were made in all these cases. However, whether these suggestions resulted in change in therapy is not known and is planned to be assessed on follow-up calls to these patients. Fourteen patients (0.79%, 95% CI 0.43–1.31%) had died due to their disease. All of these patients had advanced metastatic cancers and were on palliative therapies.
DISCUSSION
The Covid-19 pandemic prompted many countries to enforce harsh, unprecedented restrictions on movements of citizens to limit the spread and ‘flatten the curve’ of SARS-CoV-2. Although televised media and the internet was abuzz with ‘Covid meters’ presenting real-time statistics about Covid-19 infection and mortality, there was limited enquiry about the impact of the pandemic and subsequent lockdown on health outcomes of those who were already suffering from diseases such as cancers. The pandemic tapped into already scarce health resources in India, with major government hospitals in big cities concentrating on Covid-19.
Apart from the uncertainty of the lockdown, there was uncertainty about the impact of Covid-19 on cancer and its treatment. Preliminary reports from China suggest that there may be a higher proportion of cancer patients among Covid-19 victims and also a much higher probability of severe adverse events in cancer patients who get Covid-19, especially if anti-cancer therapy has been received within 14 days of being infected.7,8 However, it is unclear whether this was due to underlying cancer or due to underlying comorbid conditions and lifestyle (e.g. smoking and chronic obstructive pulmonary disease) among cancer patients.9 Faced with the dilemma of treating life-threatening malignancy or delaying treatment to prevent severe Covid-19 disease, in the absence of real evidence in this scenario, it was a difficult decision to make.
We tried to assess the impact of Covid-19 lockdown on cancer treatment at the Teleconsult Centre. Patient navigators were teamed up with doctors for the teleconsultations. In resource-limited settings with the scarcity of medical practitioners, it is difficult to have dedicated teleconsultation centres run solely by doctors. Patient navigators played a crucial role in the documentation of teleconsults while doctors made calls––this hastened the process and we could reach out to more patients in a shorter duration of time. In a week’s time, we tried to call all the patients who had planned appointments over a 5-week period. We could call only about 66% of patients; the remaining could not be tracked as telephonic contact could not be established.
The lockdown resulted in the inability of patients to come for their routine therapy sessions for >3 weeks. As mentioned in the methodology, we tried to find the best possible solution in each case scenario to help patients get the most appropriate therapy given the logistic constraints, travel restrictions, Covid threat and feasibility of treatment at their local place. This resulted in change of treatment in 75 patients. Whether these changes would affect the outcomes of these patients would only be known on future follow-ups.
Hospital visit itself carries a risk of SARS-CoV-2 infection, and in one study, it was found to be responsible for 41% of Covid-19 cases in Wuhan.10 Hence, it was important to avoid hospital visits as much as possible. By teleconsultations, we could defer follow-ups of 1034 patients (40%) who had planned appointments during the lockdown period and who were otherwise doing well on treatment, thus effectively reducing footfalls at the hospital, reducing the crowd in outpatient clinics and promoting social distancing. Patients in India spend a lot of time and money to travel long distances for treatment and follow-up. India has approximately 1.15 billion wireless phone connections for a population of 1.33 billion, with 86.98 mobile phone connections per 100 population.11 Setting up effective teleconsulting services may have applicability beyond the Covid-19 pandemic, as it can help reduce healthcare costs and improve accessibility. Now with smartphones becoming more popular, apart from teleconsultation, video consultations may provide a more satisfactory and realistic experience for the patient as well as the doctor. A prospective trial done at our centre showed a 100% concurrence rate, improved patient satisfaction and reduced cost of video follow-up compared with clinic follow-up.12 Randomized trials are needed to establish telemedicine and video consultations as an alternative to physical follow-ups to improve access and reduce cancer care costs, especially in low- and middle-income countries.
We also found that there was limited access to oral medications, for example, TKIs, at many places. Half of the patients with chronic myeloid leukaemia, who were contacted again, could not get imatinib at their local pharmacies. We, therefore, need to build a better network of pharmacies that can provide cancer-directed medications/drugs throughout the country. The Covid-19 pandemic has once again brought to the front the need to decentralize cancer care to the hinterlands rather than limiting it to a few centres of excellence.
In the pandemic situation, the impact on mortality outcomes due to SARS-CoV-2 infection versus a delay or change in cancer treatment is unclear. We will follow these patients for their oncological outcome.
Conflicts of interest
None declared
References
- Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet. 2020;395:507-13.
- [CrossRef] [PubMed] [Google Scholar]
- Coronavirus Disease (COVID-19) Pandemic. Available at www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 7 Apr 2020)
- [Google Scholar]
- Recommendations for Prioritization. Treatment and Triage of Breast Cancer Patients during the COVID-19 Pandemic. 2020. Executive Summary. Available at www.breastsurgeons.org/docs/news/The_COVID-19_Pandemic_Breast_Cancer_Consortium_Recommendations_EXECUTIVE_SUMMARY.pdf?01 (accessed on 7 Apr 2020)
- [Google Scholar]
- COVID-19 Resources. Available at www.surgonc.org/resources/covid-19-resources/ (accessed on 7 Apr 2020)
- [Google Scholar]
- Managing cancer care during the COVID-19 pandemic: Agility and collaboration toward a common goal. J Natl Compr Canc Netw 2020 Mar 20:1-4.
- [CrossRef] [PubMed] [Google Scholar]
- Telemedicine Practice Guidelines. 2020. Available at www.mohfw.gov.in/pdf/Telemedicine.pdf (accessed on 8 Apr 2020)
- [Google Scholar]
- Cancer patients in SARSCoV-2 infection: A nationwide analysis in China. Lancet Oncol. 2020;21:335-7.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical characteristics of COVID-19-infected cancer patients: A retrospective case study in three hospitals within Wuhan, China. Ann Oncol. 2020;31:894-901.
- [CrossRef] [PubMed] [Google Scholar]
- Risk of COVID-19 for patients with cancer. Lancet Oncol. 2020;21:e180.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061-9.
- [CrossRef] [PubMed] [Google Scholar]
- Highlights of Telecom Subscription Data as on 31st December 2019. 2020. Available at https://main.trai.gov.in/sites/default/files/PR_No.17of2020_0.pdf (accessed on 11 Apr 2020)
- [Google Scholar]
- Shadow study: Randomized comparison of clinic with video follow-up in glioma undergoing adjuvant temozolomide therapy. CNS Oncol. 2018;7:CNS14.
- [CrossRef] [PubMed] [Google Scholar]




