Translate this page into:
Assessment of pain in the elderly: A literature review
2 Department of Family Medicine, Konkuk University Medical Center, 120-1 Neungdong-ro (Hwayangdong), Gwangjin-gu, Seoul 05030, Korea
3 Department of Neurology, Konkuk University Medical Center, 120-1 Neungdong-ro (Hwayangdong), Gwangjin-gu, Seoul 05030, Korea
Corresponding Author:
Seol-Heui Han
Department of Neurology, Konkuk University Medical Center, 120-1 Neungdong-ro (Hwayangdong), Gwangjin-gu, Seoul 05030
Korea
alzdoc@kuh.ac.kr
| How to cite this article: Kim YS, Park JM, Moon YS, Han SH. Assessment of pain in the elderly: A literature review. Natl Med J India 2017;30:203-207 |
Abstract
Background. Pain perception is highly subjective, and effective pain management can be challenging in the elderly. We aimed to identify a set of practical measures that could be used to assess pain in elderly patients with or without cognitive impairment, as the first step towards effectively managing their pain.Methods. We used the PRISMA guidelines for this literature review. Two reviewers independently assessed titles, abstracts and full-text articles, and a third reviewer resolved any disagreements.
Results. A total of 11 285 abstracts and 103 full-text articles were assessed. Forty-one studies met the inclusion criteria. The Numeric Rating Scale, Visual Analogue Scale, Face Pain Scale and Verbal Descriptor Scale have proven valid in the elderly. The Abbey pain scale, Doloplus-2, Pain Assessment in Advanced Dementia scale, Pain Assessment Checklist for Seniors with Limited Ability to Communicate, Checklist of Nonverbal Pain Indicators, Pain Assessment for the Dementing Elderly rating tool and the Clinical Utility of the CNA Pain Assessment Tool are used in elderly patients with cognitive impairment.
Conclusions. We identified a number of reliable and valid methods for pain assessment in the elderly. Elderly patients can receive treatment in a variety of settings, and frequently it is administered by a caregiver or family member, rather than a medical employee. The development of a pain assessment tool that is not subject to variations arising from differences in settings or caregivers is needed to assess pain accurately in elderly patients, and provide timely treatment. Natl Med J India 2017;30:203–7
Introduction
Pain has been referred to as ‘the fifth vital sign’, but pain perception is highly subjective. Self-reporting is widely acknowledged as the most reliable gauge of an individual’s pain, and is regarded as the gold standard in most populations. Because elderly patients with cognitive impairment or communication difficulties are often unable to communicate their pain experiences verbally or in sufficient detail, their pain is often not recognized, or it is not effectively treated.[1],[2],[3]
The incidence of pain increases more than two-fold after the age of 60 years, and thereafter pain frequency increases every 10 years.[1] Studies have shown that 25%–50% of community-dwelling elderly adults suffer from pain.[1],[4] In many cases, effective pain management in the elderly can be complicated due to difficulty in determining whether their pain is acute or chronic. Studies indicate that elderly hospitalized patients who are asked about pain are far less likely than younger patients to report it, and thus they are less likely to receive analgesic treatment, or receive lower doses of analgesics.[5],[6]
Pain is directly associated with suffering, and it is related to the deterioration of many conditions including impaired mobility, decreased physical function, sleep disturbance and depression, as well as increased health utilization costs and decreased socialization. Pain is often overlooked and frequently undertreated, particularly in elderly patients with cognitive impairment.[7],[8] Unrelieved pain reduces a patient’s quality of life, as it isolates individuals from social stimulation, which further amplifies the functional and emotional losses directly resulting from the untreated pain.[4]
We aimed to determine a set of practical skills to assess pain in elderly patients with or without cognitive impairment, as the first step towards effective management of their pain.
Methods
We adhered to the PRISMA guidelines[9],[10] for conducting systematic reviews for this review. The primary review questions were:
- What tools are available to assess the presence of pain in elderly patients with and without cognitive impairment?
- What tools are available to assess the level of pain experienced by elderly patients with and without cognitive impairment?
Inclusion criteria
- Types of publication: publications available in English or Korean from 1997 to 2016.
- Types of study design: papers describing original studies, evidence-based guidelines or systematic reviews (qualitative and quantitative studies were included).
- Types of participants: elderly people (aged ≥65 years) with or without cognitive impairment.
Exclusion criteria
- Full-text of the article was not available.
Search strategy
Relevant full-length articles were identified via electronic searches of PubMed, EMbase, Cochrane, KoreaMed, Korean Studies Information Service System (KISS) and Korean Medical Database (KMbase) databases. The combination of search terms used was: Pain and assessment or scale or measurement or screening or questionnaire and older or elderly or senior or aged or geriatric or dementia or cognitive impairment.
Study selection and data extraction
Two reviewers (YSK, JM) independently assessed the titles and abstracts, and the full-texts of potentially relevant articles were obtained. The inclusion criteria were then independently applied to full-text articles by each of the reviewers. Disagreements were resolved by consensus or consultation with a third reviewer (YSM).
Quality of included reviews
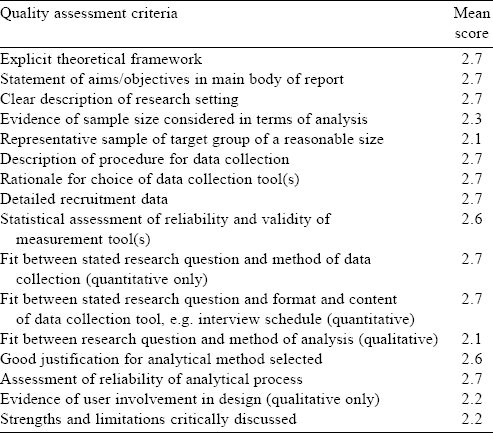
The Quality Assessment Tool for Studies with Diverse Designs[11] was used to assess study quality. Studies were assessed against the 16 criteria [Table - 1]. Publications were scored against each criterion on a 4-point scale (0–3) to determine the quality of each publication and the overall body of evidence.
Results
Article selection
After removing duplications, 11 285 records were identified. After screening titles and abstracts, it was determined that 11 052 were on the wrong topic, 42 were the wrong type of publication, and the full-text versions of 88 articles were not available. Thus, we obtained the full text of 103 articles for further analysis. After identifying and removing a further 2 duplications and 60 articles of the wrong publication type, 41 publications remained that fulfilled the eligibility criteria [Figure - 1].
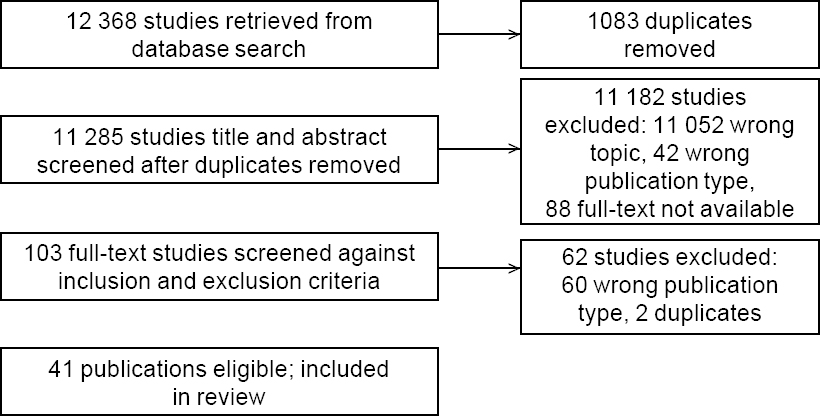 |
| Figure 1: PRISMA flow diagram |
Assessment of pain in the elderly
Self-reporting is the gold standard method for identifying pain. In patients with dementia who were not able to self-report pain, observing their behaviour in an effort to identify indicators of pain can be useful for pain assessment. However, general behaviour representing discomfort does not necessarily reflect the degree of pain, and it could be interpreted as being derived from another physiological cause or psychological distress in some cases. Therefore, it is useful for medical personnel to be aware of the usual behaviour of patients, and changes in these when the patients have discomfort, when distinguishing symptoms.[12],[13] The American Geriatrics Society (AGS) has reported six categories of pain behaviours in its Persistent Pain Guidelines : facial expressions, verbalizations/vocalizations, body language, changes in activity patterns or routines, mental status changes and changes in interpersonal interactions.[1]
Self-reported pain intensity
Self-reporting by a patient is the most accurate and reliable measure of pain intensity, and this holds true for patients of all ages. The Numeric Rating Scale (NRS), Visual Analogue Scale (VAS), Face Pain Scale (FPS), and Verbal Descriptor Scale (VDS) have proven valid and are acceptable for use in the elderly. Some of these tools can be used in patients who have mild to moderate cognitive impairment.[1],[4],[14]
The NRS[15],[16] requires the patient to rate their pain from 0 to 10, with 0 representing no pain and 10 representing extreme pain intensity. While the individual items of the NRS can be presented vertically or horizontally, a vertical presentation may make it easier and is often preferred by older people. The VAS[15],[17] consists of a 10-cm line, with the left-hand side labelled ‘no pain’ and the right-hand side labelled ‘most intense pain’. Although the VAS is acceptable for use in the elderly with regard to the psychomotor skills required to complete it, it has a higher failure rate than other less abstract tools.
The FPS[15],[16] consists of a series of progressively distressed facial expressions, and it was made for use in children. The patient chooses the face representing the severity or intensity of their current pain. Psychometric evaluation of the FPS suggest that it is a reliable and valid alternative for assessing pain intensity in the cognitively intact, and in elderly patients with mild to moderate cognitive impairment. The FPS is amenable to use in elderly patients with limited education, low literacy levels or dyslexia. However, focused psychometric evaluation of its use by the elderly is needed.
The VDS[16] is composed of a series of phrases representing different levels of pain intensity (e.g. no pain, mild pain, moderate pain, severe pain, extreme pain and the most intense pain). It has good reliability and validity in the elderly.
Observational pain assessment tools in elderly patients with cognitive impairment
An extensive literature search identified the use of seven observational pain assessment tools in elderly patients with cognitive impairment: the Abbey Pain Scale, Doloplus-2, Pain Assessment in Advanced Dementia (PAINAD) scale, Pain Assessment Checklist for Seniors with Limited Ability to Communicate (PACSLAC), Checklist of Nonverbal Pain Indicators (CNPI), Pain Assessment for the Dementing Elderly (PADE) scale, and Clinical Utility of the CNA Pain Assessment Tool (CPAT) [Table - 2].

The Abbey Pain Scale[18],[19],[20],[21] was developed in Australia to measure the severity of pain in individuals with late-stage dementia. It is reportedly efficient, effective and can be used by a variety of caregivers. The aim of the tool is to measure acute pain, chronic pain and combined acute and chronic pain. It contains six items—vocalization, facial expression, behavioural change, change in body language, physiological change and physical change. Each item is rated on a 4-point scale (0–3). Individual item scores are added to reach a total score range of 0 to 18. The interpretation is as follows: 0–2 no pain; 3–7 mild pain; 8–13 moderate pain; ≥14 severe pain. The tool has been tested in a long-term care setting by registered nurses and facility staff, and it could be completed within 1 minute. The scale was considered moderately valid, based on correlations between the total scores yielded by it and a nurse’s global pain assessment. Internal consistency ranged from 0.74 to 0.81, and intra-class correlation coefficients ranged from 0.44 to 0.63. However, test–retest reliability was not reported. The tool involves at least one cue from each of the six pain behaviour categories in the AGS Persistent Pain Guidelines: facial expressions, verbalizations/vocalizations, body language, changes in activity patterns or routines, mental status changes and changes in interpersonal interactions.
The Doloplus-2[22],[23],[24],[25],[26],[27],[28],[29],[30],[31] is a behavioural scale for evaluating pain in the elderly. It contains five somatic items (somatic complaints, protective body posture adopted at rest, protection of sore areas, expression and sleep pattern), two psychomotor items (washing and/or dressing, and mobility) and three psychosocial items (communication, social life and behaviour problems). Each item is scored 0–3, resulting in an overall score of 0–30. Five points is the threshold for pain. The tool was tested in acute care, long-term care and in the clinic by a registered nurse, and could be completed in 6–12 minutes. It demonstrated convergent and predictive validity, its internal consistency ranged from 0.58 to 0.82, and the intra-class correlation coefficient was 0.96. The tool uses five of six pain behaviour categorie s in the AGS Persistent Pain Guidelines (‘mental status changes’ is not used).
The PAIN AD Scale[6],[8],[25],[32],[33],[34],[35],[36],[37],[38],[39],[40] was designed to be a clinically relevant and easy-to-use pain assessment tool for patients with advanced dementia. The tool is an adaptation of DS-DAT and FLACC. It has five items (breathing, negative vocalization, facial expression, body language and consolability) with three response modalities scored 0–2, with a total score of 0–10. Total score interpretation was not reported in any of the studies assessed. The tool was tested in acute care, long-term care and community settings by a registered nurse, an auxiliary nurse and a caregiver. Before applying the scale, an observation period of 2–5 minutes is required. The test has moderate validity, internal consistency ranges from 0.69 to 0.85, its intra-class correlation coefficient was 0.80, inter-rater reliability ranged from 0.75 to 0.97, and test–retest reliability from 0.88 to 0.90. The tool includes only three of the six pain behaviour categories in the AGS Persistent Pain Guidelines (facial expressions, verbalizations/vocalizations, and body language).
The PACSLAC[21],[28],[35],[38],[41],[42],[43],[44],[45],[46] is a caregiver-administered pain evaluation checklist incorporating direct observation and caregiver information for assessment of pain in elderly patients who are not able to communicate well. The checklist contains four subscales and a total of 60 items : facial expressions (13 items), activity/body movements (20 items), social/personality/mood indicators (12 items), and physiological indicators/eating and sleeping changes/ vocal behaviours (15 items). Each item is scored as either present or absent. Subscale scores are added to give a total score range of 0–60. However, no interpretation of the total score is available at present.
The tool was tested in long-term care and community dwellings by a registered nurse, a special care aid, and facility staff, and could be completed in less than 5 minutes. It had moderate validity, internal consistency of 0.80–0.92, intra-class correlation coefficients of 0.89–0.96 and inter-rater reliability of 0.86. The tool is comprehensive and includes all six pain behaviour categories in the AGS Persistent Pain Guidelines.
CNPI[47],[48],[49],[50] is a behavioural observation scale for those who are unable to speak and have severe cognitive impairment. It is a modification of the University of Alabama Birmingham Pain Behavior Scale (UAB PBS), developed to measure chronic pain, from which some items have been removed and others have been redefined. Scoring includes observing patients while they are at rest and while they are moving. An item is scored as ‘1’ if the behaviour is observed during activity or rest, and as ‘0’ if the behaviour is not observed, and the total score is 0–6. After adding up the two scores (for movement and rest) the interpretation is as follows: 1–2 mild pain; 3–4 moderate; and 5–6 severe. The tool has been tested in acute care, long-term care and community- dwellings by a registered nurse and an auxiliary nurse. Completion time has not been reported. The scale has moderate validity, internal consistency of 0.54, inter-rater reliability from 0.63 to 0.82 and test–retest reliability of 0.43–0.66. The tool includes three of the six pain behaviour categories in the AGS Persistent Pain Guidelines—facial expressions, verbalizations/vocalizations and body language.
PADE[46],[51],[52] is a tool for evaluation of pain in individuals with advanced dementia, developed to help caregivers assess patient behaviour that may suggest pain. The tool has three parts and 24 items. The ‘physical’ component involves observable facial expression, breathing pattern and posture. The ‘global’ component includes proxy evaluation of pain intensity. The ‘functional assessment’ involves activities of daily living: dressing, feeding oneself and transfer from a wheelchair to bed. The items are rated via several different scoring methods. Items 1–12, 14 and 22–24 are rated using a Likert scale using a 1–4 score based on equally spaced divisions on a line. Items 13 and 15–21 are multiple-choice questions, with scores ranging from 1 to 4. Total score interpretation was not reported in any of the studies assessed. The tool was tested in long-term care by a registered nurse, an auxiliary nurse and a caregiver, and requires 5–10 minutes to complete. It has good validity, internal consistency ranged from 0.54 to 0.96 and intra-class correlation coefficients ranged from 0.81 to 0.96. The tool uses five of the six pain behaviour categories in the AGS Persistent Pain Guidelines—facial expressions, body movements, verbalizations/vocalizations, changes in activity patterns or routines, and interpersonal interactions.
CPAT[53],[54] has been used to measure pain in cognitively impaired inmates of nursing homes, and incorporates indicators of pain or no pain in five categories—facial expression, behaviour, mood, body language and activity level. Pain indicators are scored as 1 and no pain is scored as 0, with a maximum possible score of 5. For a score of 1 or more, evaluation was undertaken and the direct care provider was instructed to indicate the type of action taken. Total score interpretation was not reported in any of the studies assessed. The tool was tested in long-term care by a certified nursing assistant but the completion time was not reported. It had moderate validity, internal consistency of 0.72–0.84, intra-class correlation coefficients of 0.55–0.57, inter-rater reliability of 0.71 and test–retest reliability of 0.67. The tool includes three of the six pain behaviour categories in the AGS Persistent Pain Guidelines—facial expressions, body movements and changes in activity patterns or routines.
Conclusion
The perception of pain is highly subjective. Effective pain management can be complicated in the elderly, due to difficulty in determining whether their pain is acute or chronic. After reviewing the literature, we found a number of tools for pain assessment in the elderly with good reliability and validity. Self-reporting of pain is not confined to care facility settings. Tools that have been tested for observational pain assessment in acute care settings include the Doloplus-2, PAINAD and CNPI, and the tools that have been tested by caregivers include the PAINAD and PADE. It takes 1–12 minutes to complete observational pain assessment. Elderly patients can receive treatment in a variety of settings, including acute care, long-term care, a clinic and a community-dwelling. In addition, the pain assessor may be a caregiver or family member, pain assessment is not confined to medical staff. The development of an accurate pain assessment tool that can be administered rapidly in the elderly and is not subject to setting or caregiver limitations is needed, in order to facilitate the timely provision of medical treatment.
Acknowledgements
This research was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number HI16C0526).
Conflict of interest: None declared.
| 1. | AGS Panel on persistent pain in older persons: The management of persistent pain in older persons. J Am Geriatr Soc 2002; 50 (6 Suppl): S205-S224. [Google Scholar] |
| 2. | Bjoro K, Herr K. Assessment of pain in the nonverbal or cognitively impaired older adult. Clin Geriatr Med 2008;24:237-62, vi. [Google Scholar] |
| 3. | Schofield P, O’Mahony S, Collett B, Potter J. Guidance for the assessment of pain in older adults: A literature review. Br J Nurs 2008;17:914-18. [Google Scholar] |
| 4. | Hanks-Bell M, Halvey K, Paice JA. Pain assessment and management in aging. Online J Issues Nurs 2004;9:8. [Google Scholar] |
| 5. | de Rond ME, de Wit R, van Dam FS, Muller MJ. A pain monitoring program for nurses: Effects on communication, assessment and documentation of patients’ pain. J Pain Symptom Manage 2000;20:424-39. [Google Scholar] |
| 6. | Catananti C, Gambassi G. Pain assessment in the elderly. Surg Oncol 2010;19: 140-8. [Google Scholar] |
| 7. | American Geriatrics Society. The management of chronic pain in older persons: AGS Panel on Chronic Pain in Older Persons. J Am Geriatr Soc 1998;46:635-51. [Google Scholar] |
| 8. | Smith M. Pain assessment in nonverbal older adults with advanced dementia. Perspect Psychiatr Care 2005;41:99-113. [Google Scholar] |
| 9. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Reprint—preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Phys Ther 2009;89:873-80. [Google Scholar] |
| 10. | Harrison R, Walton M, Manias E, Smith-Merry J, Kelly P, Iedema R, et al. The missing evidence: A systematic review of patients’ experiences of adverse events in health care. Int J Qual Health Care 2015;27:424-42. [Google Scholar] |
| 11. | Sirriyeh R, Lawton R, Gardner P, Armitage G. Reviewing studies with diverse designs: The development and evaluation of a new tool. JEval ClinPract 2012; 18: 746-52. [Google Scholar] |
| 12. | Herr K, Coyne PJ, Key T, Manworren R, McCaffery M, Merkel S, Pelosi-Kelly J, et al. ; American Society for Pain Management Nursing. Pain assessment in the nonverbal patient: Position statement with clinical practice recommendations. Pain Manag Nurs 2006;7:44-52. [Google Scholar] |
| 13. | Kim HS, Yu SJ. Pain assessment in nonverbal older adults with dementia. Korean J Hosp Palliat Care 2013;16:145-54. [Google Scholar] |
| 14. | Herr K. Pain assessment in cognitively impaired older adults. Am J Nurs 2002;102: 65-7. [Google Scholar] |
| 15. | Herr KA, Garand L. Assessment and measurement of pain in older adults. Clin Geriatr Med 2001;17:457-78, vi. [Google Scholar] |
| 16. | Herr KA, Mobily PR, Kohout F J, Wagenaar D. Evaluation of the faces pain scale for use with the elderly. Clin J Pain 1998;14:29-38. [Google Scholar] |
| 17. | Wynne CF, Ling SM, Remsburg R. Comparison of pain assessment instruments in cognitively intact and cognitively impaired nursing home residents. Geriatr Nurs 2000;21:20-3. [Google Scholar] |
| 18. | Zwakhalen SM, Hamers JP, Abu-Saad HH, Berger MP. Pain in elderly people with severe dementia: A systematic review of behavioural pain assessment tools. BMC Geriatr 2006;6:3. [Google Scholar] |
| 19. | Hadjistavropoulos T, Herr K, Turk DC, Fine PG, Dworkin RH, Helme R, et al. An interdisciplinary expert consensus statement on assessment of pain in older persons. Clin J Pain 2007;23 (1 Suppl): S1-S43. [Google Scholar] |
| 20. | Abbey J, Piller N, De Bellis A, Esterman A, Parker D, Giles L, et al. The Abbey pain scale: A 1-minute numerical indicator for people with end-stage dementia. Int J Palliat Nurs 2004;10:6-13. [Google Scholar] |
| 21. | van Iersel T, Timmerman D, Mullie A. Introduction of a pain scale for palliative care patients with cognitive impairment. Int J Palliat Nurs 2006;12:54-9. [Google Scholar] |
| 22. | Wary B, Doloplus C. [Doloplus-2, a scale for pain measurement]. Soins Gerontol 1999;19:25-7. [Google Scholar] |
| 23. | Lefebvre-Chapiro S. The DOLOPLUS® 2 scale-evaluating pain in the elderly. Eur J Palliat Care 2001;8:191. [Google Scholar] |
| 24. | Pautex S, Herrmann FR, Michon A, Giannakopoulos P, Gold G. Psychometric properties of the Doloplus-2 observational pain assessment scale and comparison to self-assessment in hospitalized elderly. Clin J Pain 2007;23:774-9. [Google Scholar] |
| 25. | Zwakhalen SM, Hamers JP, Berger MP. The psychometric quality and clinical usefulness of three pain assessment tools for elderly people with dementia. Pain 2006;126:210-20. [Google Scholar] |
| 26. | Hølen JC, Saltvedt I, Fayers PM, Bjørnnes M, Stenseth G, Hval B, et al. The Norwegian Doloplus-2, a tool for behavioural pain assessment: translation and pilot- validation in nursing home patients with cognitive impairment. Palliat Med 2005;19:411-17. [Google Scholar] |
| 27. | Cole LJ, Farrell MJ, Gibson SJ, Egan GF. Age-related differences in pain sensitivity and regional brain activity evoked by noxious pressure. Neurobiol Aging 2010;31: 494-503. [Google Scholar] |
| 28. | Aubin M, Giguère A, Hadjistavropoulos T, Verreault R. [The systematic evaluation of instruments designed to assess pain in persons with limited ability to communicate]. Pain Res Manag 2007;12:195-203. [Google Scholar] |
| 29. | Hølen JC, Saltvedt I, Fayers PM, Hjermstad MJ, Loge JH, Kaasa S. Doloplus-2, a valid tool for behavioural pain assessment? BMC Geriatr 2007;7:29. [Google Scholar] |
| 30. | Pautex S, Michon A, Guedira M, Emond H, Le Lous P, Samaras D, et al. Pain in severe dementia: S elf-assessment or observational scales? J Am Geriatr Soc 2006;54:1040-5. [Google Scholar] |
| 31. | Ando C, Hishinuma M. Development of the Japanese DOLOPLUS-2: A pain assessment scale for the elderly with Alzheimer’s disease. Psychogeriatňcs 2010;10:131-7. [Google Scholar] |
| 32. | Hadjistavropoulos T, Herr K, Prkachin KM, Craig KD, Gibson SJ, Lukas A, et al. Pain assessment in elderly adults with dementia. Lancet Neurol 2014; 13:1216-27. [Google Scholar] |
| 33. | Warden V, Hurley AC, Volicer L. Development and psychometric evaluation of the pain assessment in advanced dementia (PAINAD) scale. J Am Med Dir Assoc 2003;4:9-15. [Google Scholar] |
| 34. | Leong IY, Chong MS, Gibson SJ. The use of a self-reported pain measure, a nurse- reported pain measure and the PAINAD in nursing home residents with moderate and severe dementia: A validation study. Age Ageing 2006;35:252-6. [Google Scholar] |
| 35. | Lane P, Kuntupis M, MacDonald S, McCarthy P, Panke JA, Warden V, et al. A pain assessment tool for people with advanced Alzheimer’s and other progressive dementias. Home Healthc Nurse 2003;21:32-7. [Google Scholar] |
| 36. | Costardi D, Rozzini L, Costanzi C, Ghianda D, Franzoni S, Padovani A, et al. The Italian version of the pain assessment in advanced dementia (PAINAD) scale. Arch Gerontol Geriatr 2007;44:175-80. [Google Scholar] |
| 37. | Schuler MS, Becker S, Kaspar R, Nikolaus T, Kruse A, Basler HD. Psychometric properties of the German ‘Pain Assessment in Advanced Dementia Scale’ (PAINAD- G) in nursing home residents. J Am Med Dir Assoc 2007;8:388-95. [Google Scholar] |
| 38. | Lints-Martindale AC, Hadjistavropoulos T, Lix LM, Thorpe L. A comparative investigation of observational pain assessment tools for older adults with dementia. Clin J Pain 2012;28:226-37. [Google Scholar] |
| 39. | Paulson-Conger M, Leske J, Maidl C, Hanson A, Dziadulewicz L. Comparison of two pain assessment tools in nonverbal critical care patients. Pain Manag Nurs 2011;12:218-24. [Google Scholar] |
| 40. | Helme RD, Gibson SJ. The epidemiology of pain in elderly people. Clin Geriatr Med 2001;17:417-31, v. [Google Scholar] |
| 41. | Zwakhalen SM, Hamers JP, Berger MP. Improving the clinical usefulness of a behavioural pain scale for older people with dementia. J Adv Nurs 2007;58:493-502. [Google Scholar] |
| 42. | Hadjistavropoulos T, Hunter P, Dever Fitzgerald T. Pain assessment and management in older adults: Conceptual issues and clinical challenges. Can Psychol 2009;50: 241-54. [Google Scholar] |
| 43. | Fuchs-Lacelle S, Hadjistavropoulos T. Development and preliminary validation of the pain assessment checklist for seniors with limited ability to communicate (PACSLAC). Pain Manag Nurs 2004;5:37^9. [Google Scholar] |
| 44. | DeWaters T, Faut-Callahan M, McCann JJ, Paice JA, Fogg L, Hollinger-Smith L, et al. Comparison of selfreported pain and the PAINAD scale in hospitalized cognitively impaired and intact older adults after hip fracture surgery. OrthopNurs 2008;27: 21-8. [Google Scholar] |
| 45. | Hutchison RW, Tucker WF Jr, Kim S, Gilder R. Evaluation of a behavioral assessment tool for the individual unable to self-report pain. Am J Hosp Palliat Care 2006;23:328-31. [Google Scholar] |
| 46. | Cohen-Mansfield J, Lipson S. The utility of pain assessment for analgesic use in persons with dementia. Pain 2008;134:16-23. [Google Scholar] |
| 47. | Feldt KS. The checklist of nonverbal pain indicators (CNPI). Pain Manag Nurs 2000;1:13-21. [Google Scholar] |
| 48. | Feldt K. Improving assessment and treatment of pain in cognitively impaired nursing home residents. Ann Long-Term Care 2000;8:36-42. [Google Scholar] |
| 49. | Jones KR, Fink R, Hutt E, Vojir C, Pepper GA, Scott-Cawiezell J, et al. Measuring pain intensity in nursing home residents. J Pain Symptom Manage 2005 ;30:519-27. [Google Scholar] |
| 50. | Nygaard HA, Jarland M. The Checklist of Nonverbal Pain Indicators (CNPI): Testing of reliability and validity in Norwegian nursing homes. Age Ageing 2006;35:79-81. [Google Scholar] |
| 51. | Villanueva MR, Smith TL, Erickson JS, Lee AC, Singer CM. Pain assessment for the dementing elderly (PADE): Reliability and validity of a new measure. J Am Med Dir Assoc 2003;4:1-8. [Google Scholar] |
| 52. | Cohen-Mansfield J. Pain assessment in noncommunicative elderly persons––PAINE. Clin J Pain 2006;22:569-75. [Google Scholar] |
| 53. | Cervo FA, Raggi RP, Bright-Long LE, Wright WK, Rows G, Torres AE, et al. Use of the certified nursing assistant pain assessment tool (CPAT) in nursing home residents with dementia. Am J Alzheimers Dis Other Demen 2007;22:112-19. [Google Scholar] |
| 54. | Cervo FA, Bruckenthal P, Chen JJ, Bright-Long LE, Fields S, Zhang G, et al. Pam assessment in nursing home residents with dementia: Psychometric properties and clinical utility of the CNA pain assessment tool (CPAT). J Am Med Dir Assoc 2009;10:505-10. [Google Scholar] |
Fulltext Views
12,015
PDF downloads
3,232




