Translate this page into:
Bilateral internal jugular vein ectasia: A rare cause of neck swelling
Correspondence to S. JAYENDIRAN, No. 26 Bharathiyar Road, Karaikal, Pondicherry 609602, India; jayendiransubramaniam@gmail.com
[To cite: Srinivasa V, Jayendiran S, Kayarkar D, Aliyar A, Aravind TI. Bilateral internal jugular vein ectasia: A rare cause of neck swelling. Natl Med J India 2023;36:23–5. DOI: 10.25259/NMJI_282_20]
Abstract
Internal jugular vein ectasia or phlebectasia is a condition in which there is an isolated fusiform dilatation of the internal jugular vein. The patient usually presents with swelling in the neck, which aggravates in size while coughing or straining. This is a rare condition and is often mis-diagnosed. It can be diagnosed by proper history, clinical examination and imaging. We report a 5-year-old boy who had bilateral internal jugular vein ectasia aggravating in size while straining and coughing. Ultrasonography and computed tomography scan showed dilatation of internal jugular veins on both sides. Since the patient was asymptomatic and had no complications, he was advised regular follow-up. This rare benign condition should be kept in mind as a differential diagnosis of an expansile neck mass.
INTRODUCTION
Ectasia or phlebectasia of the internal jugular vein (IJV) is rare and is often misdiagnosed and managed inappropriately. ‘Phlebectasia’ is a fusiform dilatation of the vein without tortuosity. The term phlebectasia differs from varix which denotes dilatation of the vein along with tortuosity. More than a hundred patients with phlebectasia are reported in the world literature.1,2 We report a 5-year-old boy with bilateral IJV phlebectasia.
THE CASE
A 5-year-old boy presented with a painless swelling on the right side of the neck which appeared on coughing and while straining. The patient had no history of trauma, previous neck surgery or pain. There was no history of dysphonia, dyspnoea or dysphagia. Family history was non-contributory. All developmental milestones were found to be appropriate for age.
On examination of the patient in a relaxed state, there was no obvious neck swelling. While the patient was performing Valsalva manoeuvre, the swelling appeared on the right side of the neck. It was fusiform, measuring 3×4 cm in size, palpable on the right anterior border of the sternocleidomastoid muscle extending to the anterior triangle of the neck and clavicle, was soft in consistency, non-tender and with no increase in the local temperature. There was no palpable thrill or audible bruit over the swelling.
Oropharyngeal and systemic examination was normal. Flexible fibre-optic laryngoscopy did not show any abnormality.
To confirm the diagnosis, the patient underwent ultrasonography (USG), which showed the luminal diameter of IJV on the right side at rest to be 6 mm while on Valsalva manoeuvre it was 22 mm. The luminal diameter of the left IJV was 5 mm, which increased during Valsalva manoeuvre to 18 mm. This was the case on both sides.
Colour Doppler done for this patient showed turbulent vascular flow in both enlarged veins with no evidence of thrombosis.
The USG findings were confirmed with contrast-enhanced computed tomography (CECT) of the neck, which showed the luminal diameter of IJV on the right side at rest as 15 mm while on Valsalva manoeuvre it was 23.1 mm. The luminal diameter of the left IJV was 6 mm, while during Valsalva manoeuvre, it was 18.3 mm (Fig. 1). Based on the investigations, the final diagnosis was made as phlebectasia of bilateral IJV, with right side more than the left.
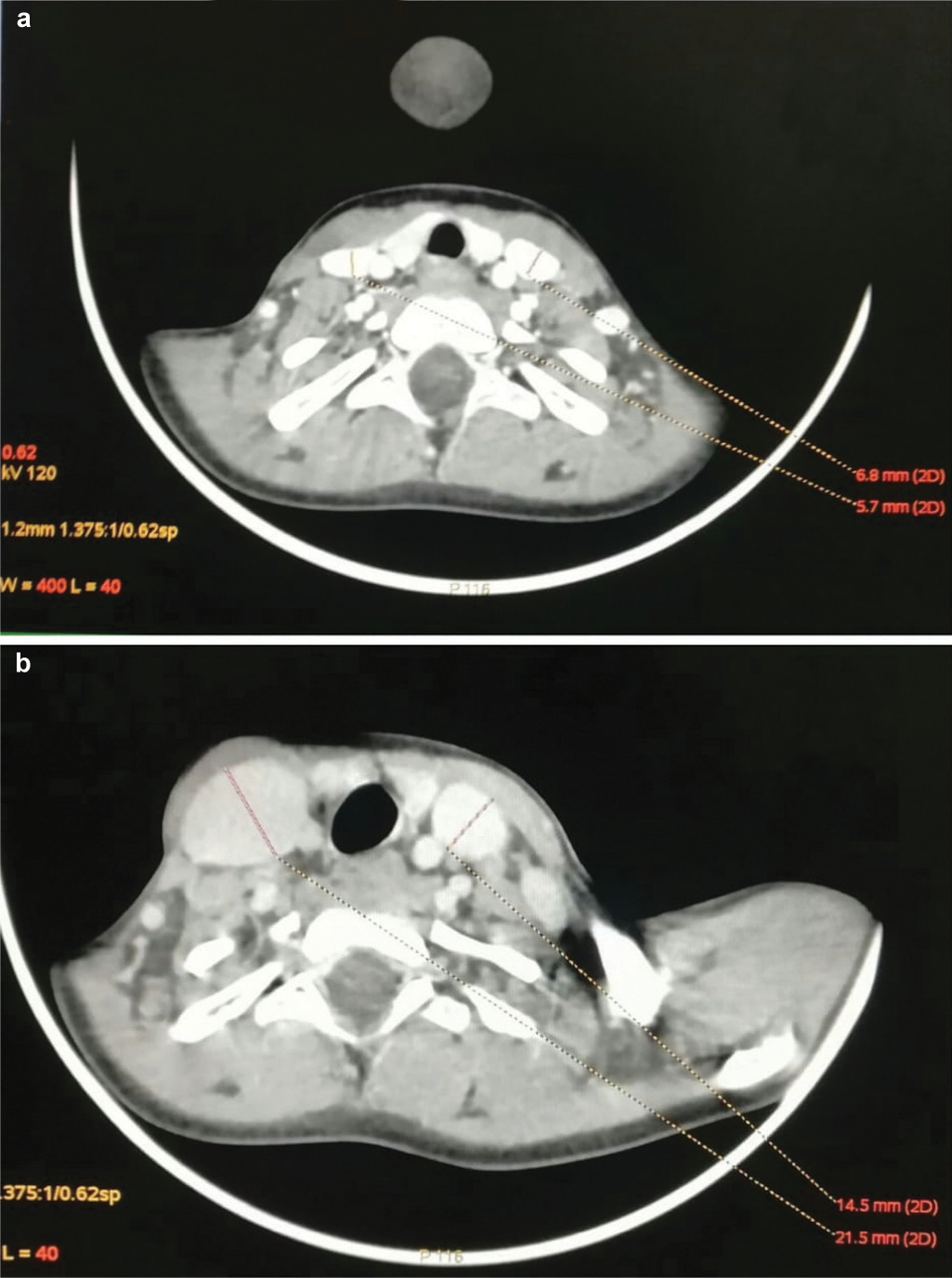
- (a) Cross-section of computed tomography neck showing normal internal jugular vein on both sides when the patient is in normal position; (b) cross-section of computed tomography neck showing dilatation of the internal jugular vein on both sides when the patient is doing the Valsalva manoeuvre
Since the patient was asymptomatic without any complications, the parents were explained about the disease and advised regular follow-up with an early review if there was development of any symptoms or sudden increase in the size of the swelling.
DISCUSSION
Ectasia is an isolated fusiform or saccular dilatation of the vein. It should not be confused with a varix, which is a dilated tortuous vein.3 Other terms used in the literature to describe this entity include phlebectasia, venous cyst, venous aneurysm and venectasia.4
Jugular vein phlebectasia is an anomaly of the vein which usually presents in children as a soft, compressible cystic swelling in the neck during straining, crying, coughing and sneezing. It is provoked by Valsalva manoeuvre and disappears completely at rest.5–7 In 1929, Zukschwerdt8 first described the term internal jugular ectasia. It was characterized by Gerwig in 1952.9 Since then, a variety of hypotheses regarding its aetiology have been proposed, which include: (i) congenital origin;10 (ii) compression of the vein between the cupula of the right lung and the head of clavicle;11 (iii) anomalous reduplication of the IJV;8 and (iv) increased scalenus anterior muscle tone.12 Teodorescu suggested trauma also as a cause of ectasia.3,13
Histopathological examination of a surgical specimen showed a wide range of findings in the literature.10 The characteristic finding of phlebectasia included thinning of the vein wall and carotid sheath, decreased or absence of elastic layer, diffuse fibrosis and minimal muscle layer.10,14–18 However, some studies showed the venous wall to be normal.
Paleri and Gopalakrishnan hypothesized that due to several anatomical factors, intrathoracic pressure could be easily communicated to the right jugular bulb.1 According to LaMonte, phlebectasia is more common on the right side because the right innominate vein lies in contact with the right apical pleura. Therefore, any elevation in intrathoracic pressure can be directly transmitted to the right IJV.11
Diagnosis is usually made by an ultrasound.1,3,10,19,20 Along with ultrasound, colour Doppler flow imaging can be done to confirm vascular flow and thrombus formation in the lumen of the IJV.21 Eksioglu et al. suggested using an anteroposterior diameter >15 mm as a cut-off for both sides for the diagnosis of internal jugular phlebectasia.22 Jianhong et al. believe that it is important to do an ultrasound on both sides and compare, both at rest and on straining or Valsalva manoeuvre.23
For all patients, the opposite side may not be involved and should be measured for comparison. Although it may appear unilateral clinically, internal jugular phlebectasia can occur bilaterally as in our patient. CECT scan and venography are other imaging studies that can be done. CECT can be used to assess the exact extent of the venous abnormalities.24
The differential diagnosis of neck swelling in children are many, but a swelling which occurs on straining decreases the possibilities to phlebectasia, laryngocoele, superior mediastinal cyst and inflation of pulmonary apical bullae. Among these, the most common diagnosis is laryngocoele.25–27
Normal laryngoscopy and the absence of an air-filled sac on plain X-ray can rule out laryngocoele. A thoracic CT scan excludes the possibility of tumour or cyst of the mediastinum.27
An association of the condition with Menkes disease, a rare disorder of copper metabolism, has been reported.28 Kwok et al. reported internal jugular phlebectasia in a patient with bronchial asthma.29
Complications such as thrombosis30 and Horner syndrome31 are rarely reported in the literature. However, rupture has not been reported till now in the literature. In the absence of complications, the patient can be kept under observation. Moreover, surgery should not be the main target of the clinician in this case.24,32
Surgery is usually required for those with complications. Surgical intervention includes ligation or excision of the involved jugular vein or longitudinal constriction suture venoplasty plus encapsulation of the involved part with medical Dacron cloth or polytetrafluoroethylene artificial vessel patch to strengthen the vessel wall.23,27
Conflicts of interest
None declared
References
- Jugular phlebectasia: Theory of pathogenesis and review of literature. Int J Pediatr Otorhinolaryngol. 2001;57:155-9.
- [CrossRef] [PubMed] [Google Scholar]
- Unusual case of focal neck swelling: Phlebectasia of internal jugular vein with intracranial extension. Int J Appl Basic Med Res. 2015;5:58-60.
- [CrossRef] [PubMed] [Google Scholar]
- Internal jugular phlebectasia. Int J Pediatr Otorhinolaryngol. 1986;12:165-71.
- [CrossRef] [PubMed] [Google Scholar]
- Focal ectasia of internal jugular vein. Med J Armed Forces India. 2009;65:282-3.
- [CrossRef] [PubMed] [Google Scholar]
- Congenital phlebectasia of the internal jugular vein (case report) Duhok Med J. 2008;2:155-60.
- [Google Scholar]
- Internal jugular phlebectasia in children: A diagnostic dilemma. Int J Surg. 2008;19:1-4.
- [CrossRef] [Google Scholar]
- An intriguing case of ectasia of external jugular vein presenting as intermittent neck mass. Indian J Otolaryngol Head Neck Surg. 2016;68:367-9.
- [CrossRef] [PubMed] [Google Scholar]
- Seltene lokalisation einer Venektasie. Deutsche Zeitschrift für Chirurgie. 1929;216:283-5.
- [CrossRef] [Google Scholar]
- Internal jugular phlebectasia in two siblings: Manometric and histopathologic studies of the pathogenesis. J Pediatr Surg. 1990;25:762-5.
- [CrossRef] [PubMed] [Google Scholar]
- Internal jugular phlebectasia. A clinicoroentgenographic diagnosis. Arch Otolaryngol. 1976;102:706-8.
- [CrossRef] [Google Scholar]
- Contracture of the scalenus anterior, causing aneurysmal varix of right internal jugular vein: A case report. JBJS. 1946;28:147.
- [Google Scholar]
- Phlebectasie post-traumatique de la jugulaire interne. Ann, OtoLaryngol (Paris). 1978;95:411-16.
- [Google Scholar]
- Internal jugular phlebectasia: Case report and review of the literature. Am J Surg. 1964;108:380-3.
- [CrossRef] [PubMed] [Google Scholar]
- Internal jugular phlebectasia of the infant [(author's transl)] Nihon Jibiinkoka Gakkai Kaiho. 1979;82:1361-4.
- [CrossRef] [PubMed] [Google Scholar]
- Isolated aneurysm of the internal jugular vein: A report of three cases. J Pediatr Surg. 1982;17:130-1.
- [CrossRef] [PubMed] [Google Scholar]
- CT and ultrasonographic findings in jugular vein ectasia. J Ultrasound Med. 1984;3:417-20.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasonic diagnosis of jugular vein aneurysm. J Clin Ultrasound. 1982;10:85-7.
- [CrossRef] [PubMed] [Google Scholar]
- Usefulness of ultrasonography and Doppler color flow imaging in the diagnosis of internal jugular phlebectasia. Heart Vessels. 1992;7:95-8.
- [CrossRef] [PubMed] [Google Scholar]
- Sonographic measurement criteria for the diagnosis of internal jugular phlebectasia in children. J Clin Ultrasound. 2013;41:486-92.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical treatment of jugular vein phlebectasia in children. Am J Surg. 2006;192:286-90.
- [CrossRef] [PubMed] [Google Scholar]
- Phlebectasia of internal jugular vein-a rare differential case of neck swelling with review of literature. Iran J Otorhinolaryngol. 2019;31:239-42.
- [Google Scholar]
- Jugular phlebectasia in children: Is it rare or ignored? J Pediatric Surg. 1999;34:1829-32.
- [CrossRef] [PubMed] [Google Scholar]
- Aneurysm of the internal jugular vein manifesting after prolonged positive pressure ventilation. Head Neck. 1991;13:450-2.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical repair of left internal jugular phlebectasia. J Vasc Surg. 2008;47:1337-8.
- [CrossRef] [PubMed] [Google Scholar]
- Internal jugular phlebectasia in Menkes disease. Int J Pediatr Otorhinolaryngol. 2007;71:1145-8.
- [CrossRef] [PubMed] [Google Scholar]
- Unilateral right-sided internal jugular phlebectasia in asthmatic children. J Paediatrics Child Health. 2000;36:517-19.
- [CrossRef] [PubMed] [Google Scholar]
- Phlebectasia of the jugular system. J Craniomaxillofac Surg. 1989;17:96-8.
- [CrossRef] [PubMed] [Google Scholar]
- Horner's syndrome due to jugular venous ectasia. Childs Nerv Syst. 1995;11:533-5.
- [CrossRef] [PubMed] [Google Scholar]
- Management of internal jugular vein phlebectasia. Otolaryngol Head Neck Surg. 1995;112:473-5.
- [CrossRef] [PubMed] [Google Scholar]




